Abstract
Purpose
The aim of the study was to compare the efficacy of parecoxib for postoperative analgesia after endoscopic turbinate and sinus surgery with the prodrug of acetaminophen, proparacetamol.
Materials and Methods
Fifty American Society of Anesthesiology (ASA) physical status I-II patients, receiving functional endoscopic sinus surgery (FESS) and endoscopic turbinectomy, were investigated in a prospective, randomized, double-blind manner. After local infiltration with 1% mepivacaine, patients were randomly allocated to receive intravenous (IV) administration of either 40 mg of parecoxib (n = 25) or 2 g of proparacetamol (n = 25) 15 min before discontinuation of total IV anaesthesia with propofol and remifentanil. A blinded observer recorded the incidence and severity of pain at admission to the post anaesthesia care unit (PACU) at 10, 20, and 30 min after PACU admission, and every 1 h thereafter for the first 6 postoperative h.
Results
The area under the curve of VAS (AUCVAS) calculated during the study period was 669 (28 - 1901) cm·min in the proparacetamol group and 635 (26 - 1413) cm·min in the parecoxib group (p = 0.34). Rescue morphine analgesia was required by 14 patients (56%) in the proparacetamol group and 12 patients (48%) in the parecoxib (p ≥ 0.05), while mean morphine consumption was 5 - 3.5 mg and 5 - 2.0 mg in the proparacetamol groups and parecoxib, respectively (p ≥ 0.05). No differences in the incidence of side effects were recorded between the 2 groups. Patient satisfaction was similarly high in both groups, and all patients were uneventfully discharged 24 h after surgery.
Conclusion
In patients undergoing endoscopic nasal surgery, prior infiltration with local anaesthetics, parecoxib administered before discontinuing general anaesthetic, is not superior to proparacetamol in treating early postoperative pain.
Keywords: Postoperative pain, parecoxib, proparacetamol, analgesia, nasal surgery
INTRODUCTION
Functional endoscopic sinus surgery (FESS) and endoscopic turbinectomy have been developed in recent years in order to minimize surgical invasiveness.1,2 These procedures are assumed to be more comfortable and less painful to patients; nonetheless, they are somehow associated with mild to moderate postoperative pain, which is related to both surgical trauma and nasal packing.3
When the expected postoperative pain ranges from mild to moderate, routine analgesic treatment is usually based on non-opioid analgesics with rescue opioids.4 However, the optimal analgesic regimen after endoscopic nasal surgery has not been wholly accepted and an opioid-oriented treatment is still often used.5
Acetaminophen is an effective and safe non-opioid analgesic used to relieve mild to moderate pain. It is poorly soluble and unstable in aqueous solution, however its prodrug, proparacetamol, is water-soluble and can be administered intravenously for the treatment of postoperative pain. In the blood, proparacetamol is rapidly and completely converted by plasma esterase into 50% paracetamol.6
Parecoxib is a water-soluble prodrug which undergoes complete and rapid biotransformation to valdecoxib, a potent selective inhibitor of cyclooxygenase-2 (anti-COX-2 agent).7,8 The COX-2 inhibitors offer the advantage of less gastric toxicity and bleeding complications than traditional nonsteroidal anti-inflammatory drugs (NSAIDs).9 Studies on oral administration of rofecoxib (COX-2 inhibitor) and the combination of hydrocodone/acetaminophen after endoscopic ENT surgery have shown to be safe and effective postoperative analgesia,5,10 but oral administration may limit the use of these agents in the early postoperative period. The parenteral formulations of valdecoxib and acetaminophen have never been compared after endoscopic nasal surgery. We, therefore, conducted this prospective, randomized, double-blinded study to compare the efficacy of parecoxib for early postoperative analgesia after endoscopic turbinate and sinus surgery with the efficacy of proparacetamol for the same postoperative pain.
MATERIALS AND METHODS
With institutional ethics committee approval and patients' written consent, 50 ASA physical status I-II patients, aged 18 - 65 years, undergoing FESS (uncinectomy, middle antrostomy, and further procedures like ethmoidectomy and sphenoid exploration when indicated) and turbinate surgery were prospectively enrolled. Patients unable to cooperate or had history of gastric bleeding, impaired liver (transaminases ≥ twice upper limit) and/or renal function (creatinine ≥ 2.0 mg/dL), history of drug or alcohol abuse, chronic pain requiring major analgesics, sedatives, or corticosteroids, prothrombotic tendencies, and known allergy to NSAIDs or other drugs used in the study were excluded.
No premedication or prophylactic antiemetic drugs were given. All patients received total IV anaesthesia with propofol (2 mg/kg bolus IV, followed by a continuous infusion at 4 - 6mg/kg/h) and remifentanil (infusion rate ranging between 0.1 and 0.25 µg/kg/min). Muscle relaxation with rocuronium (0.6 mg/kg) was given to facilitate tracheal intubation and mechanical ventilation. Standard monitoring was used including electrocardiography (lead II), heart rate, noninvasive arterial blood pressure, and pulse oximetry. The attending anaesthesiologist who managed intraoperative anaesthesia was blinded to patient grouping. The same 2 surgeons performed all surgical procedures. Preoperative surgical field infiltration with 100 mg of 1% mepivacaine and 0.25mg of epinephrine was performed by a surgeon.
Fifteen min before stopping remifentanil infusion, patients were randomly allocated to receive either 40 mg of parecoxib (group parecoxib, n = 25) or 2g of proparacetamol (group proparacetamol, n = 25) using a computer generated sequence of random numbers. Since treatment drugs have different presentations and mode of administration, a double-dummy design was applied. Proparacetamol was administered by slow infusion over 15 min whereas parecoxib was injected by rapid bolus. Each patient received both an active product and the placebo of the other product. The physicians preparing the placebo and the study drugs were not further involved in patient management.
At the end of surgery, bilateral nasal packs (Merocel-hydroxylated polyvinyl acetate, Medtronic Xomed, Jacksonville, FL, USA) were placed in all patients. IV anaesthetics were then discontinued, the patients were extubated after recovery of adequate spontaneous ventilation, and transferred to the PACU.
An independent blinded observer recorded the degree of pain at PACU admission and after 10, 20, and 30 min, then at every h for the first 6 h after surgery. At the same time, hemodynamic variables and occurrence of untoward events were also recorded. The degree of pain was measured using a 10 cm visual analogue scale (VAS, where "0" is no pain, "10" the worst imaginable pain). In case of inadequate pain relief (VAS ≥ 4 cm), rescue IV analgesia was given with 2 mg of boluses of morphine injected at 10-min intervals until adequate pain relief, and morphine consumption during the first 6 h after surgery was recorded.
After 6 h, patients meeting PACU discharge criteria were transferred to the surgical ward. Pain was evaluated by surgical nursing staff. Following the 6th postoperative h, rescue analgesia for VAS ≥ 4 was no longer morphine but 2 g of proparacetamol IV since this drug is the standard postoperative pain medication on ward for patients undergoing FESS and turbinates surgery. The intensity of pain reported at 12 and 24 h after surgery was also recorded by surgical nursing staff, since it as is routine at our institution.
Patient satisfaction was evaluated at 24 h after surgery using a 4-point numeric verbal scale (1 = not satisfied; 2 = partially satisfied; 3 = satisfied; 4 = extremely satisfied). Both on the day of surgery and at 24 h, a surgeon who was blinded to patient grouping evaluated the presence of excessive bleeding with a subjective scale based on clinical experience.
Statistical analysis
The hypothesis under test was that IV administration of parecoxib before completion of endoscopic ENT surgery might reduce the degree of pain compared to proparacetamol. To objectify the exposition to pain of patients, we calculated the AUCVAS. The AUC for pain was estimated using the trapezium method by multiplying the time interval between 2 VAS measurements by their average, and is reported as a summary measure with cm·min as the units; we calculated the AUC for pain during the first 6 h (AUCVAS-6h) and 24 h after surgery (AUCVAS-24 h).
To calculate the sample size required, we considered the results of previous studies that evaluated the degree of pain reported after endoscopic ENT surgery.5,10 The main outcome variable was the AUCVAS-24 h. We considered a reduction in median AUCVAS-24 h of 800 cm·min with an effect size to standard deviation ratio (E/S) of 0.8 as clinically relevant. A total of 25 patients per group were required to detect the designed difference in the AUCVAS, accepting a 2-tailed α error of 5% and β error of 20%.11
Statistical analysis was based on an intention-to-treat analysis and performed using the program Systat 7.0 (SPSS Inc., Chicago, IL, USA). Gaussian distribution of collected data was first evaluated using the Kolmogorov-Smirnov test. Continuous variables were then analysed using student's t-test or Mann-Whitney U-test as appropriate. Changes over time were also assessed using a 2-way non-parametric analysis for repeated measures. Fisher's exact test and Sheffe's test were also used for post hoc analysis. Categorical variables were analyzed using contingency table analysis and Fisher's exact test. Data are presented as mean (± SD), median (range) and number (percentage) as appropriate. A p value ≤ 0.05 was considered significant.
RESULTS
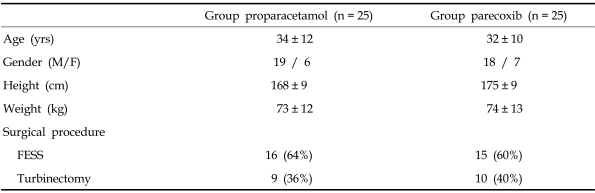
No differences in demographic parameters (Table 1) as well as in intraoperative and postoperative hemodynamic variables (data not presented) were observed between the 2 groups.
Table 1.
Anthropometric Parameters of Studied Patients
Results are presented as mean (± SD) or number (%).
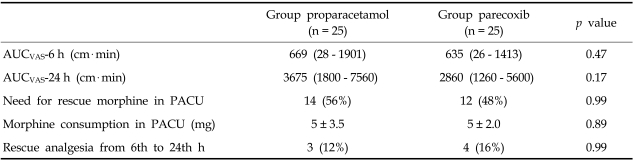
No differences were reported between the 2 groups in the median (range) AUCVAS calculated during the first 6 and 24 h, or in the proportion of patients requiring rescue morphine and total morphine consumption before PACU discharge, and need for rescue analgesia during the first 24 h after surgery (Table 2). Fig. 1 shows mean VAS changes during the first 6 h after surgery in the 2 groups.
Table 2.
Area Under the Curve of Pain, Need for Rescue Morphine and Morphine Consumption
Area under the curve of pain over time during the first 6 (AUCVAS-6 h) and 24 hours (AUCVAS-24 h), need for rescue morphine and morphine consumption before post anaesthesia care unit (PACU) discharge, and need for rescue analgesia after PACU discharge during the first day after surgery in patients receiving either proparacetamol (group Proparacetamol, n = 25) or parecoxib (group Parecoxib, n = 25) after endoscopic ENT surgery. Results are presented as mean (± SD) or median (range) based on normal distribution of data or number (%).
Fig. 1.
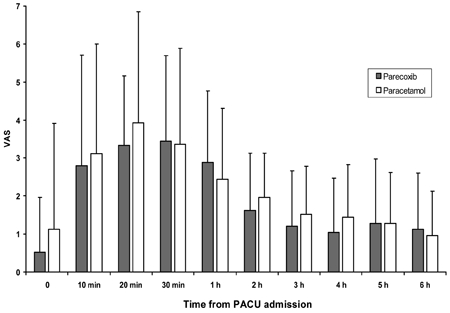
Mean postoperative VAS measured at PACU admission for the first 6 h.
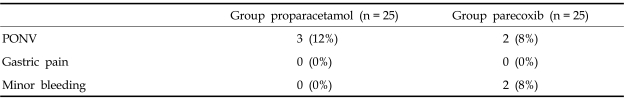
Table 3 shows the incidence of side effects recorded in the 2 groups. Side effects were not related to the need for rescue doses of morphine, and bleeding was controlled simply by changing nasal cavity packing without surgical revision.
Table 3.
Incidence of Adverse Events Reported during First 24 h After Surgery in Patients Receiving Proparacetamol or Parecoxib After Endoscopic ENT Surgery
PONV, post operative nausea and vomit.
Results are presented as number (%).
Patient satisfaction was similarly high in both groups [4 (3 - 4) in group paracetamol and 4 (3 - 4) in group precoxib (p = 0.99)], and all patients were discharged uneventfully 24 h after surgery. However, satisfaction of patients who did not require rescue analgesia during the first day after surgery (morphine during the first 6 h and proparacetamol thereafter) was significantly higher than that of patients who received supplementary analgesia [4 (4 - 4) vs 3 (3 - 4), respectively, (p < 0.001)].
DISCUSSION
This study compared the analgesic efficacy and tolerability of COX-2 selective inhibitor parecoxib to proparacetamol for postoperative analgesia after endoscopic ENT surgery. The results of this prospective, randomized, double-blinded investigation showed that the administration of 40 mg of parecoxib IV was not preferable to 2 g of proparacetamol IV in managing postoperative pain. The proportion of patients requiring rescue morphine and total morphine consumption as well as the incidence of side effects did not differ between the 2 groups.
The degree of pain reported after endoscopic sinus surgery was of moderate intensity,3,10 nonetheless, routine use of local anaesthetic infiltration or topical bupivacaine packing is not sufficient for the treatment of postoperative pain after nasal surgery, requiring additional systemic analgesia to achieve an opioid-sparing effect.3,12 Friedman et al. reported no differences in postoperative pain after endoscopic sinus surgery between infiltration with long acting (bupivacaine) or short acting (lidocaine) local anaesthetics.3 Postoperative pain score and the need for systemic analgesics were similar between the 2 groups.
Pain after nasal and sinus surgery is usually maximal in the first few postoperative h.3 During this time, oral opioids are commonly prescribed as analgesics for symptomatic relief, but these drugs are frequently associated with adverse effects such as sedation, nausea, vomiting, urinary retention, pruritus, and respiratory depression.5 For this reason, commonly used protocols of postoperative analgesia are based on a multimodal approach including non-opioid analgesics in order to achieve an opioid-sparing effect with concomitant reduction of opioid-related side effects.13 NSAIDs are the most commonly used non-opioid analgesics for such purposes.13
Although parecoxib and proparacetamol belong to the same pharmacological family, they act by different mechanisms. The analgesic action of parecoxib results from the inhibition of the COX-2 isoenzyme that plays an important role in the synthesis of prostaglandin E2 while proparacetamol only weakly inhibits of prostaglandine synthesis and minimizes the typical actions of NSAIDs such as antiplatelet activity and gastrotoxicity.7,14 The efficacy of parecoxib in postoperative pain relief is still controversial. Ng et al.15 reported that 40 mg of parecoxib IV is less effective than 30mg of ketorolac IV in the first h after minor gynaecological laparoscopic surgery. On the contrary, Bikhazi et al.16 reported that a single dose of 40 mg of parecoxib was as effective as 30 mg of ketorolac after open gynaecologic surgery while Papadima et al.19 reported that 40 mg of parecoxib and 8 mg of lornoxicam were equianalgesic in the management of pain after laparoscopic cholecystectomy.17 Concerning proparacetamol, Van Aken et al. showed a similar analgesic efficacy between single dose of 2 g of proparacetamol IV and 10 mg of morphine IM in controlling acute postoperative pain after dental surgery.18 Peduto et al.19 demonstrated a significant morphine sparing effect of proparacetamol after orthopaedic surgery while Varrassi et al.20 and Zhou et al.21 reported similar analgesic efficacy between proparacetamol and ketorolac after gynaecologic and orthopaedic surgery.19-21
Parenteral formulations of valdecoxib and acetaminophen allow intraoperative administration with a short onset of action6,7 while postoperative parenteral formulation of acetaminophen provides a significantly better and longer analgesic effect than the same dosage in oral form.6
Little information is available in the current literature evaluating the comparative efficacy of parecoxib and proparacetamol. A recently published trial compared the effects of these 2 drugs only after inguinal hernia repair.22 The authors investigated the intensity of postoperative pain, morphine consumption, and patient satisfaction after a single injection of 40 mg of parecoxib or 2 injections of 2 g of proparacetamol within the first 12 postoperative h. Total morphine consumption did not differ between the 2 groups, and pain was slightly less intense in the parecoxib group at rest, but pain did not differ while coughing. The incidence of side effects was similar and patient satisfaction was higher in the parecoxib group, although at an increased cost.22,23
In conclusion, this prospective, randomized, double blinded study showed that 40 mg of parecoxib administered IV before discontinuing general anaesthesia is not superior to 2 g of proparacetamol IV in covering early postoperative pain after endoscopic ENT surgery.
References
- 1.Slack R, Bates G. Functional endoscopic sinus surgery. Am Fam Physician. 1998;58:707–718. [PubMed] [Google Scholar]
- 2.May M, Schaitkin BM. Erasorama surgery. Curr Opin Otolaryngol Head Neck Surg. 2002;10:19–21. [Google Scholar]
- 3.Friedman M, Venkatesan TK, Lang D, Caldarelli DD. Bupivacaine for postoperative analgesia following endoscopic sinus surgery. Laryngoscope. 1996;106:1382–1385. doi: 10.1097/00005537-199611000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89:409–423. [PubMed] [Google Scholar]
- 5.Church CA, Stewart C, 4th, O-Lee TJ, Wallace D. Rofecoxib versus hydrocodone/acetaminophen for postoperative analgesia in functional endoscopic sinus surgery. Laryngoscope. 2006;116:602–606. doi: 10.1097/01.MLG.0000208341.30628.16. [DOI] [PubMed] [Google Scholar]
- 6.Rømsing J, Møiniche S, Dahl JB. Rectal and parenteral paracetamol, and paracetamol in combination with NSAIDs, for postoperative analgesia. Br J Anaesth. 2002;88:215–226. doi: 10.1093/bja/88.2.215. [DOI] [PubMed] [Google Scholar]
- 7.Cheer SM, Goa KL. Parecoxib (parecoxib sodium) Drugs. 2001;61:1133–1143. doi: 10.2165/00003495-200161080-00010. [DOI] [PubMed] [Google Scholar]
- 8.Dalpiaz AS, Peterson D. Parecoxib: a shift in pain management? Expert Rev Neurother. 2004;4:165–177. doi: 10.1586/14737175.4.2.165. [DOI] [PubMed] [Google Scholar]
- 9.Dannhardt G, Kiefer W. Cyclooxygenase inhibitors-current status and future prospects. Eur J Med Chem. 2001;36:109–126. doi: 10.1016/s0223-5234(01)01197-7. [DOI] [PubMed] [Google Scholar]
- 10.Turan A, Emet S, Karamanlioğlu B, Memis D, Turan N, Pamukcu Z. Analgesic effects of rofecoxib in ear-nose-throat surgery. Anesth Analg. 2002;95:1308–1311. doi: 10.1097/00000539-200211000-00039. [DOI] [PubMed] [Google Scholar]
- 11.Browner WS, Black D, Newman B, Hulley SB. Estimating sample size and power. In: Hulley SB, Cummings SR, editors. Designing clinical research-an epidemiologic approach. Baltimore: Williams & Wilkins; 1988. pp. 139–150. [Google Scholar]
- 12.Buchanan MA, Dunn GR, Macdougall GM. A prospective double-blind randomized controlled trial of the effect of topical bupivacaine on post-operative pain in bilateral nasal surgery with bilateral nasal packs inserted. J Laryngol Otol. 2005;119:284–288. doi: 10.1258/0022215054020322. [DOI] [PubMed] [Google Scholar]
- 13.American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2004;100:1573–1581. doi: 10.1097/00000542-200406000-00033. [DOI] [PubMed] [Google Scholar]
- 14.Chandrasekharan NV, Dai H, Roos KL, Evanson NK, Tomsik J, Elton TS, et al. COX-3 a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci U S A. 2002;99:13926–13931. doi: 10.1073/pnas.162468699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng A, Temple A, Smith G, Emembolu J. Early analgesic effects of parcoxib versus ketorolac following laparoscopic sterilization: a randomized controlled trial. Br J Anaesth. 2004;92:846–849. doi: 10.1093/bja/aeh161. [DOI] [PubMed] [Google Scholar]
- 16.Bikhazi GB, Snabes MC, Bajwa ZH, Davis DJ, LeComte D, Traylor L, et al. A clinical trial demonstrates the analgesic activity of intravenous parecoxib sodium compared with ketorolac or morphine after gynecologic surgery with laparotomy. Am J Obstet Gynecol. 2004;191:1183–1191. doi: 10.1016/j.ajog.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Papadima A, Lagoudianakis EE, Antonakis PT, Pattas M, Kremastinou F, Katergiannakis V, et al. Parecoxib vs. Lornoxicam in the treatment of postoperative pain after laparoscopic cholecystectomy: a prospective randomized placebo-controlled trial. Eur J Anaesthesiol. 2007;24:154–158. doi: 10.1017/S0265021506001293. [DOI] [PubMed] [Google Scholar]
- 18.Van Aken H, Thys L, Veekman L, Buerkle H. Assessing analgesia in single and repeated administrations of propacetamol for postoperative pain: comparison with morphine after dental surgery. Anesth Analg. 2004;98:159–165. doi: 10.1213/01.ANE.0000093312.72011.59. [DOI] [PubMed] [Google Scholar]
- 19.Peduto VA, Ballabio M, Stefanini S. Efficacy of propacetamol in the treatment of postoperative pain. Morphine-sparing effect in orthopaedic surgery. Italian Collaborative Group on Propacetamol. Acta Anaesthesiol Scand. 1998;42:293–298. doi: 10.1111/j.1399-6576.1998.tb04919.x. [DOI] [PubMed] [Google Scholar]
- 20.Varrassi G, Marinangeli F, Agro F, Aloe L, De Cillis P, De Nicola A, et al. A double-blinded evaluation of propacetamol versus ketorolac in combination with patient-controlled analgesia morphine: analgesic efficacy and tolerability after gynecologic surgery. Anesth Analg. 1999;88:611–616. doi: 10.1097/00000539-199903000-00028. [DOI] [PubMed] [Google Scholar]
- 21.Zhou TJ, Tang J, White PF. Propacetamol versus ketorolac for treatment of acute postoperative pain after total hip or knee replacement. Anesth Analg. 2001;92:1569–1575. doi: 10.1097/00000539-200106000-00044. [DOI] [PubMed] [Google Scholar]
- 22.Beaussier M, Weickmans H, Paugam C, Lavazais S, Baechle JP, Goater P, et al. A randomized, double-blind comparison between parecoxib sodium and propacetamol for parenteral postoperative analgesia after inguinal hernia repair in adult patients. Anesth Analg. 2005;100:1309–1315. doi: 10.1213/01.ANE.0000150972.88708.13. [DOI] [PubMed] [Google Scholar]
- 23.Tilleul P, Weickmans H, Sean PT, Lienhart A, Beaussier M. Cost analysis applied to postoperative analgesia regimens: a comparison between parecoxib and propacetamol. Pharm World Sci. 2007;29:374–379. doi: 10.1007/s11096-006-9083-x. [DOI] [PubMed] [Google Scholar]