Abstract
The use of accurate and reliable clinical and imaging modalities for quantifying leg-length discrepancy (LLD) is vital for planning appropriate treatment. While there are several methods for assessing LLD, we questioned how these compared. We therefore evaluated the reliability and accuracy of the different methods and explored the advantages and limitations of each method. Based on a systematic literature search, we identified 42 articles dealing with various assessment tools for measuring LLD. Clinical methods such as use of a tape measure and standing blocks were noted as useful screening tools, but not as accurate as imaging modalities. While several studies noted that the scanogram provided reliable measurements with minimal magnification, a full-length standing AP computed radiograph (teleoroentgenogram) is a more comprehensive assessment technique, with similar costs at less radiation exposure. We recommend use of a CT scanogram, especially the lateral scout view in patients with flexion deformities at the knee. Newer modalities such as MRI are promising but need further investigation before being routinely employed for assessment of LLD.
Level of Evidence: Level IV, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Inequality in leg length is commonly associated with compensatory gait abnormalities and may lead to degenerative arthritis of the lower extremity and lumbar spine [29, 40]. Patients with leg-length discrepancy (LLD) can also have angular and torsional deformities as well as soft tissue contractures of the ipsilateral or contralateral extremity that may influence their functional leg lengths. For instance, flexion contractures around the knee and hip can cause apparent shortening of the leg while abduction contractures of the hip and equinus deformity of the ankle tend to functionally lengthen the affected extremity. Besides clinical evaluation, there are several imaging modalities that have been described to quantify LLD. The use of appropriate clinical methods and imaging modalities for measuring the LLD is vital to properly treat a patient with unequal leg lengths or related symptoms.
The currently available imaging modalities include plain radiography, computed radiography, microdose digital radiography, ultrasonography, CT, and MRI. Accuracy of a technique is defined as the variation of the measurement using the imaging method compared with the actual measure, whereas reliability of the technique is the variation between observers and within a single observer in obtaining measurements. One needs to consider the reliability, accuracy, magnification, radiation dose, cost, need for special equipment, convenience, and ability to image the entire extremity when choosing the imaging technique for assessing LLD. Despite many reports, there appears to be no comprehensive review of the various clinical and imaging modalities as the subject of a single manuscript.
The purpose of this article was to (1) identify the various clinical and imaging modalities described for assessing leg length discrepancy; (2) report the available data on the accuracy and interobserver and intraobserver reliability for each assessment tool; (3) compare the reported results for various assessment tools for LLD; and (4) discuss the potential advantages and pitfalls that have been described with each assessment tool.
Search Criteria and Strategies
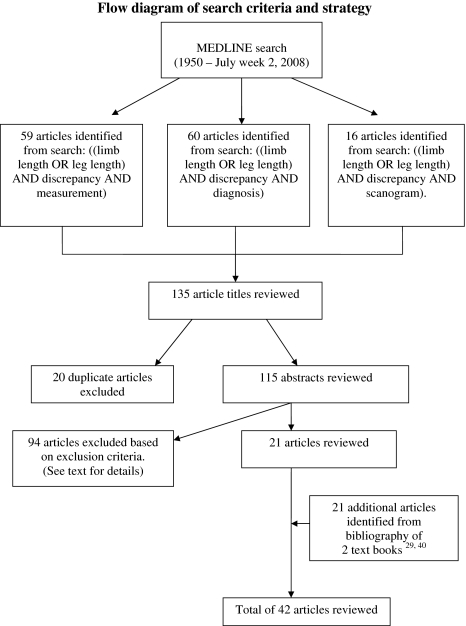
We performed a Medline search of articles published from 1950 to July (week 2) 2008. Three separate search strategies were employed using distinct search terms. The first search, using the terms: ((limb length or leg length) and discrepancy and measurement).mp. [mp = title, original title, abstract, name of substance word, subject heading word] yielded 59 articles. The second search, using the terms: ((limb length or leg length) and discrepancy and diagnosis).mp. [mp = title, original title, abstract, name of substance word, subject heading word] yielded 60 articles. The third search, using the terms: ((limb length or leg length) and discrepancy and scanogram).mp. [mp = title, original title, abstract, name of substance word, subject heading word] yielded 16 articles. There were 20 articles that appeared in more than one of the three searches, yielding a total of 115 unique articles (Fig. 1). We also reviewed relevant book chapters along with the accompanying bibliography from two pediatric orthopaedic textbooks (Morrissy and Weinstein [29], Shapiro [40]). Only those articles that described a method used to assess leg-length discrepancy and/or evaluated the accuracy, and interobserver and intraobserver variability of the assessment tool were included in this review. Articles focusing on the etiology, prediction, and treatment of LLD as well as those with no English abstract were excluded. Any articles that described intraoperative assessment of the length of a single lower extremity without assessing LLD were also excluded. The current review is based on information available from 42 distinct articles (Fig. 1).
Fig. 1.
A flow diagram outlines the search criteria and methodology employed that lead to the 42 pertinent articles on methods for assessing leg length discrepancy.
A brief description of each available method used to determine LLD, results of our literature review, including data comparing two or more measurement techniques, are detailed in the relevant sections. The potential advantages and pitfalls of each modality are presented in the Discussion section.
Methods used for Assessing Leg-length Difference
Clinical Techniques
Tape measure
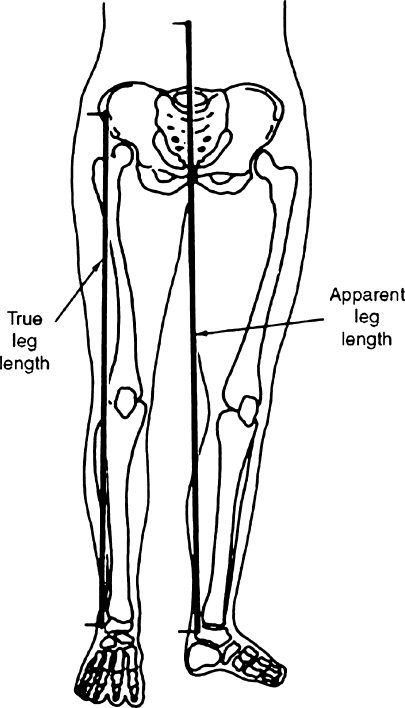
A tape measure is typically used to measure the length of each lower extremity by measuring the distance between the anterior superior iliac spine (ASIS) and the medial malleolus and is referred to as the “direct” clinical method for measuring LLD (Fig. 2). However, differences in the girth of the two limbs, and difficulty in identifying bony prominences as well as angular deformities can contribute to errors using this clinical measurement tool. Moreover, there are certain causes of LLD such as fibular hemimelia and posttraumatic bone loss involving the foot where a significant portion of the limb shortening is distal to the ankle mortise. Thus, it may be more accurate to measure the true length from the pelvis to the bottom of the heel as it is more easily reproducible and can account for shortening distal to the ankle. In some cases, lengths of the appendicular skeleton may be equal, but apparent shortening may result from pelvic obliquity or contractures around the hip and knee joints. An apparent leg length can be measured from the umbilicus to the medial malleoli of the ankle (Fig. 2).
Fig. 2.
A “direct” measurement using a tape measure can be utilized to measure the “true” leg length from the anterior superior iliac spine (ASIS) to the medial malleolus. The “apparent” leg length is measured from the umbilicus to the medial malleolus. Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2006 [29].
Rondon et al. [35] compared true and apparent measurements of LLD using clinical methods with radiographic measurement of LLD in 17 adult patients. Despite high interobserver reliability of the true (ICC, 0.99) and apparent (ICC, 0.88) methods of clinically assessing LLD, the concordance between the true measurement and radiographic assessment (ICC, 0.80) and apparent method and radiographic assessment (ICC, 0.75) was lower. In a prospective study of 10 adults with LLD and nine asymptomatic volunteers, Beattie et al. [7] compared the variability of measurements using tape measure with a scanogram. A single examiner examined the LLD of all 19 subjects using a tape measure from the ASIS to medial malleolus on two separate occasions and compared the clinical results with those obtained using a scanogram. The mean value obtained from the two clinical measurements correlated better with the radiographic measurement of LLD (ICC, 0.793) than those obtained during the first (ICC, 0.683) or second (ICC, 0.790) clinical assessment. The tape measurements were less reliable in the healthy subjects compared to those individuals with LLD. The authors cautioned against relying solely on clinical assessment of LLD and encouraged using the average value of two separate measurements when using a tape measure to assess LLD. In another study, Cleveland et al. [8] compared tape measurements of LLD of 10 erect patients with standing and supine radiographs. They reported a statistically significant difference (p < 0.05) and poor to moderate correlation when comparing the clinical and radiographic techniques.
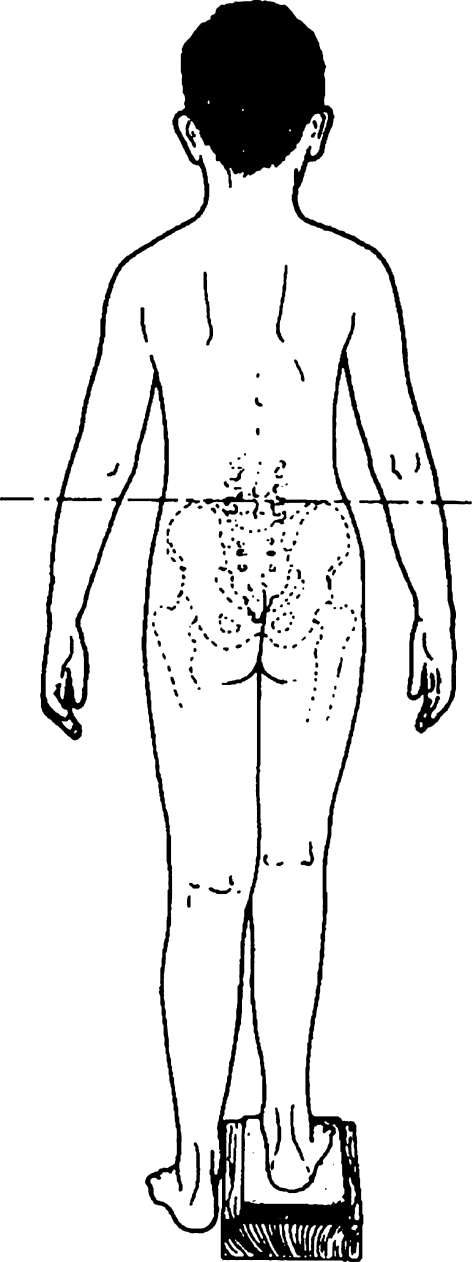
Standing on Blocks
Another method to measure LLD is to level the pelvis of the erect patient by placing blocks of known height under the short limb. This is referred to as the “indirect” clinical method for measuring LLD (Fig. 3). This method takes into account the disparity in foot height between the two limbs and also aids in determining the functional LLD (which may be different from the actual LLD) by using varying heights of the block to establish the additional length required for the patient to feel level.
Fig. 3.
Placing blocks of known height beneath the heel of the short leg to level the pelvis allows “indirect” measurement of leg length discrepancy. This method is slightly more reliable and accurate than use of the tape measure. Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2006 [29].
Hanada et al. [15] assessed the reliability and validity of measuring LLD using “iliac crest palpation and book correction” in adult subjects with simulated LLD ranging from 7 to 53 mm and compared clinical observations with those obtained using a standing AP view of the pelvis. The intraobserver (ICC, 0.98) and interobserver (ICC, 0.91) reliability for the clinical measurement was high with a mean difference of 1.6 mm in the measurement of LLD for the same observer and 1 mm between two observers. The iliac crest palpation method tended to underestimate the induced LLD by an average of 3.8 mm and underestimated the LLD measured on a standing radiograph of the pelvis by an average of 5.1 mm. Jonson and Gross [20] reported reliability data for measuring LLD using the block method in healthy adult Naval officers. Based on the measurements by two experienced physical therapists, the intraobserver (ICC, 0.87) and interobserver (ICC 0.70) reliability was high. The mean absolute difference in measurement was 1.7 mm for intraobserver and 2.2 mm between the two observers. Aspegren et al. [4] compared the visual correction using the block method to assess LLD with two erect AP pelvis radiographs, one with and the other without the same height of the lift that was used to visually level the pelvis on 41 consecutive patients who presented to a chiropractic clinic for back pain. The authors reported a correlation between the two methods (Eta = 0.885). Lampe et al. [24] compared the agreement in measuring LLD between two clinical methods, that is, use of a tape measure and standing blocks with orthoroentgenograms in 190 children attending a limb lengthening clinic. Ninety-five percent of the measurements using the wooden boards were within −14 and +16 mm of the results obtained using radiography. The tape measure had significantly less agreement. Terry et al. [43] assessed interobserver and intraobserver variability of three clinical methods of assessing LLD in 16 patients among four observers with different levels of training. The clinical methods included direct measurement with a tape measure from the ASIS to the lateral malleolus, ASIS to medial malleolus, and standing on blocks. All three clinical measurement techniques had high reliability with intraobserver intraclass correlation coefficients (ICC) of 0.88, 0.78, and 0.86 respectively and interobserver ICC of 0.83, 0.8, and 0.83, respectively. However, the direct measurement using a tape measure on a full-length slit scanogram measurement was more reliable with intraobserver ICC of 0.99 and intraobserver ICC of 0.98. Harris and coworkers [16] compared assessment of LLD using clinical methods including a tape measure from the ASIS to medial malleolus and the block test with CT scanogram findings in 35 adults following a femoral shaft fracture. There was a strong correlation between the two clinical methods (p = 0.003). The tape measurement and block test correlated well with the patient-perceived LLD, while the CT scanogram did not correlate well. Moreover, there was no correlation between the CT scanogram and the two clinical methods with a mean absolute difference of 7.2 mm in assessing LLD between the clinical methods and CT scan. The authors suggested that the physical exam may be more clinically relevant than the CT scanogram.
Authors in the field of chiropractic medicine, physical therapy, and podiatry have described other methods such as the prone leg exam, visual postural analysis [6, 11, 33, 34], and various hand-held devices to check pelvic tilt [30, 31] that have not been adequately studied and we believed were beyond the scope of this publication.
Imaging Methods
Plain Radiography
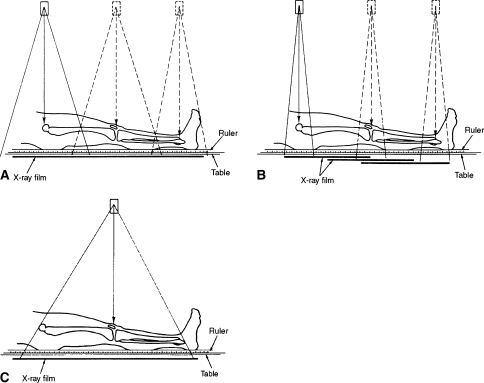
The three distinct techniques for assessing LLD using standard radiography include orthoroentogenogram, scanogram, and teleoroentgenogram (Fig. 4). A description of all three radiographic methods is followed by a review of the reliability and accuracy of these techniques collectively. Some of the studies comparing clinical evaluation with radiographic techniques have already been described in the previous section.
Fig. 4A–C.
(A) An orthoroentgenogram utilizes three radiographic exposures centered over the hip, knee and ankle joints in order to minimize magnification error. A single large cassette is placed under the patient who remains laying still between the three exposures. Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2006 [29]. (B) The scanogram technique also utilizes three radiographic exposures, one each centered over the hip, knee and ankle joint in order to minimize magnification error. The patient remains supine next to a calibrated ruler and unlike the orthoroentgenogram, the standard length radiographic cassette is moved for the three exposures. Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2006 [29]. (C) A teleoroentgenogram consists of a single long cassette placed behind the patient, while the xray beam is centered over the knee joint. It is preferable to do this study with the patient standing. While this technique is subject to magnification, less radiation exposure and opportunity to comprehensively assess the entire extremity for underlying etiology and deformity analysis makes this imaging tool an attractive option for detailed assessment of leg length discrepancy. Reprinted with permission from Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia: Lippincott Williams & Wilkins; 2006 [29].
Orthoroentogenogram
The orthoroentogenogram was initially described by Green in 1946 [13]. This radiographic technique was developed to minimize measurement error secondary to magnification by using three distinct exposures centered over the hip, knee, and ankle [13]. This imaging method differs from a scanogram in that a longer cassette is required for the orthoroentogenogram, with an additional burden of cost, storage, and special equipment (Fig. 4A).
Scanogram
There is some inconsistency in the literature regarding the term “scanogram.” The term “scanogram” may have been derived from the technique of slit scanography, described in 1937 [28], in which the xray beam is tightly collimated to a thin transverse slit that exposes the film as the xray tube is moved from one end of the limb to another. Others have used the term “scanogram” [29, 38, 40] to describe a modification of the orthoroentgenogram taken with three separate exposures centered at the hip, knee, and ankle using a standard-sized cassette (35 × 43 cm) as opposed to the long cassette (35 × 110 cm) as was originally described for an orthoroentgenogram [13]. A technique quite similar to the currently used scanogram was described by Merrill in 1942, although the term “scanogram” was not used [27]. He described a specially constructed 18 × 48 inch plywood grid with copper wires that were incorporated 1 inch apart along with lead numbers placed on the even-numbered wires. The patient lay supine on the wooded grid with sandbags at the feet and straps across the thighs. Three radiographic exposures were made, one each centered over the ankle, knee and hip joints while the patient lay still. Currently, the scanogram is made with the lower limbs similarly positioned with both patellae pointing towards the ceiling and a radio-opaque ruler taped to the table between the limbs. The patient-to-tube distance is typically 101 cm. Three separate AP images are obtained centered over the hip, knee, and ankle joints, using three separate 35 × 43-cm cassettes (Fig. 4B). The film cassette is moved under the patient between exposures while the patient remains motionless between the three exposures.
Teleoroentgenogram
The teleoroentgenogram is a full-length standing AP radiograph of the lower extremity. It consists of a single radiographic exposure of both lower limbs, with the xray beam centered at the knee from a distance of approximately 6 feet (180 cm) while the patient stands erect with both patellae pointing directly anteriorly (Fig. 4C). An attempt is made to level the pelvis with an appropriately sized lift placed under the short limb. If both iliac crests are at the same level, indicating equalization of LLD, one can simply measure the height of the lift under the short limb to calculate the LLD.
Several authors [13, 18, 29, 38] have mentioned magnification error related to assessment of limb lengths when using a teleoroentgenogram. The magnitude of the magnification error is dependent on various factors including the length and girth of the limb, distance of the xray source to the cassette, and divergence of the xray beam. Green et al. [13] compared the magnification produced by a teleoroentgenogram with a supine orthoroentgenogram. Using 10 adult human skeletons they reported a mean magnification of 4.5% (1.8 cm) for the femoral segment and 3% (0.9 cm) for the tibial segment. Because these specimens did not have LLD, the authors were unable to comment on the difference in limb lengths measured by the two imaging techniques. However, based on their clinical experience, they did comment that although the teleoroentgenogram may not measure the true length of the bone, it “fairly accurately” assesses the relative lengths of the two extremities at a single exam [13].
Machen and Stevens [26] cited seven cases of children with LLD in which, compared to the scanogram, the standing full-length radiograph (teleoroentgenogram) revealed more information regarding underlying diagnosis and lower-limb alignment. They suggested that the scanogram may be superfluous and that the teleoroentgenogram was more clinically relevant in evaluating patients with LLD. Cleveland et al. [8] compared the LLD measurements using digital standing (teleoroentgenogram) and supine (orthoroentgenogram) radiographs in 10 adults with back pain. Using 10 mm as the threshold for meaningful difference, they reported no difference between the two tests. Linear regression analysis of the calculated LLD using the standing and supine radiographs demonstrated moderate correlation (r2 = 56.75). Despite a magnification of approximately 5%, the measurement of LLD using full-length standing AP radiographs is very similar in accuracy to the scanogram, especially on the absence of significant mechanical axis deviation [38]. In another study, Sabharwal et al. [36] compared the measurements based on full-length standing radiographs (teleoroentgenograms) before and after removal of a circular external fixator. They found the mean absolute difference in the radiographic measurement of limb lengths between the two radiographs to be 20 mm (p < 0.0001) for the ipsilateral and 20.2 mm (p < 0.0001) for the contralateral unaffected extremity. The authors cautioned clinicians against relying on the teleoroentgenogram for assessing lower-limb length and alignment in patients with an overlying circular external fixator. Other techniques such as a lateral scanogram or a biplanar CT scan [1, 12, 19] may improve the accuracy of LLD measurement in such patients.
Computed Radiography
Computed radiography (CR) is a relatively recent advance in the measurement of leg-length discrepancy that is gaining popularity [37, 38] (Fig. 5). In order to obtain a full-length standing radiograph of the lower extremities, the minimum patient-to-tube distance is 203 cm, and is increased for taller individuals. A latent image is produced that is stored on a photostimulatable phosphor receptor contained in a standard radiographic cassette. The images are recorded on a computed radiography long-length imaging system utilizing a vertical cassette holder with three individual 35 × 43-cm CR storage phosphor cassettes. The three images are then stitched at the CR reader console, using customized software. The composite image thus obtained is transferred digitally and can be manipulated by an automated system such as a picture archiving and communication system (PACS) resulting in a film radiograph. The operator can enhance the final image by using the computer to adjust the image parameters. As a result, quality radiographs can be obtained consistently with a significant reduction in the radiation dose compared to standard film screen systems, a feature that is very useful for patients who require repeated radiographic examination due to leg-length discrepancy [21, 38].
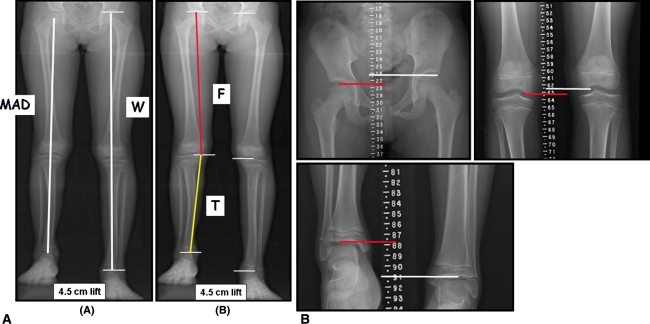
Fig. 5A–B.
(A) Standing AP radiograph of the lower extremity (modified teleoroentgenogram) performed using computed radiography on a young child with a congenital shortening of the tibia of approximately 4.5 cm. This radiograph is made with the child standing on a appropriate height lift under the short leg to level the pelvis. Besides assessing leg length discrepancy, along with length of the whole leg (W) as well as femur (F) and tibia (T), this imaging modality can be used to measure mechanical axis deviation (MAD) and joint orientation angles around the knee. (B) The modified scanogram of the same child as shown in A performed using computed radiography. Unlike a teleoroentgenogram, this imaging modality requires three radiographic exposures; one each centered over the hip, knee and ankle joints. Although a scanogram has less magnification error compared to a teleoroentgenogram, the scanogram is performed supine, is typically associated with greater radiation exposure, does not allow visualization of the entire length of the femur (F) and tibia (T) and fails to account for any shortening related to the foot. Reprinted with permission from the Journal of Bone and Joint Surgery, Inc., from Sabharwal S, Zhao C, McKeon JJ, McClemens E, Edgar M, Behrens F. Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J Bone Joint Surg Am. 2006;88:2243–2251 [38].
Sabharwal et al. [38] evaluated 111 patients with LLD who had undergone CR-based scanogram and teleoroentgenogram on the same day. Despite a 4.6% (33 mm) magnification noted when measuring the absolute length of the lower extremity with the standing radiograph, the mean difference in LLD measurement between the two CR techniques was only 5 mm. There was a strong correlation (r = 0.96) in the measurement of LLD between the two methods. Patients with less than 20 mm of mechanical axis deviation on the standing radiograph had better correlation with the scanogram than those with larger magnitude of malalignment. The mean radiation dose was 1.6 to 3.8 times greater for the CR-based scanogram study than the teleoroentgenogram and the charges of both studies were identical. Thus, the authors supported using a CR-based standing full-length radiograph as the initial imaging study when assessing a patient with LLD. In another study, Sabharwal et al. [37] reported on the intraobserver and interobserver reliability among five blinded observers with varying degrees of experience to assess LLD using CR-based supine scanograms and standing teleoroentgenograms of 70 patients. The intraobserver reliability for all five observers was high for scanogram (ICC, 0.975–0.995) as well as teleoroentgenogram (ICC, 0.939–0.996). The mean absolute difference for intraobserver reliability was 1.5 to 2.6 mm for scanogram and 1.5 to 4.6 mm for the standing radiograph. The interobserver reliability among the five observers was also high for scanogram (ICC, 0.979) and teleoroentgenogram (ICC, 0.968). The mean absolute difference for interobserver reliability was 2.6 mm for scanogram and 3 mm for the standing radiograph. The authors recommended using the teleoroentgenogram for evaluating patients with LLD since the reliability was as good as the scanogram and allowed for a more comprehensive examination of the lower extremity.
Microdose Digital Radiography
Microdose digital radiography is another form of computer-aided imaging that substantially reduces the radiation exposure to patients in comparison with conventional radiographic techniques [3]. Using a vertical gantry, the patient stands in front of the xray assembly and remains stationary during the 20-second scanning process [3]. A continuous series of photon beams collimated to act as a point source are projected through the patient to strike a computerized detector. The source assembly and detector move together, scanning the field in a line-by-line motion so that the beam is always horizontal to the patient. As the detector is extremely efficient in detecting and processing the point source of xray photons, a patient receives an exposure of only 1 to 2 mrad during the scan. This nearly negligible radiation exposure to the patient makes the technique especially attractive for problems that require serial radiograph evaluation such as progressive leg-length inequalities.
In a study of 25 children with LLD, Altongy et al. [3] found microdose digital radiography more accurate than orthoroentgenograms. Compared to the digital radiography, orthoroentgenographic measurements of leg lengths and LLD were larger by an average of 3 mm and 4 mm. The largest reported interobserver difference in measurement of leg length and LLD was 4 mm and 6 mm respectively for orthoroentgenograms and 6 mm and 8 mm for microdose digital radiographs.
Ultrasound
Ultrasound has been used to measure leg length discrepancy by various authors from Europe [22, 23, 42]. In this technique, the ultrasound transducer is used to identify the bony landmarks at the hip, knee, and ankle joints [42].
Terjesen et al. [42] compared the measurements of LLD using real-time ultrasonography in 45 patients with the results obtained using standing radiographs. There was a linear relationship between the findings of the two techniques (r = 0.94) with a mean difference of −1.9 mm, and the limits of agreement were −9.1 to 5.3 mm. The mean difference in the measurement of LLD between two examiners using ultrasound was 1.7 mm. Although the ultrasound was slightly less reliable than the standing radiograph, given the lack of radiation, the authors recommended the ultrasound as the initial screening tool in patients being evaluated for LLD. Defrin et al. [9] reported high intraobserver reliability (ICC, 0.99) of measuring LLD using ultrasound in 33 patients with low back pain. Krettek et al. [23] compared the LLD measurements obtained with ultrasonography with two clinical methods (tape measure and standing blocks) and with teleoroentgenogram in 50 patients. The mean divergence in measurement of LLD between the ultrasound and standing radiograph was 0.9 mm, with a maximum of 6.4 mm. The clinical methods with mean divergence of −1.2 mm (tape measure) and −1 mm (standing block) were slightly less accurate than ultrasound measurement.
CT Scanogram
Digitalized images obtained with a CT scan have also been used for measuring LLD [1, 2, 12, 17, 19, 44]. Typically, an anteroposterior (AP) scout view of the bilateral femurs (Fig. 6) and tibias are obtained, although use of lateral view CT scanograms has also been reported [1, 12]. Cursors are placed over the superior aspect of the imaged femoral head and the distal portion of the medial femoral condyle [2, 17, 19] with the distance between these two cursors representing the length of the individual femur. The tibial length is similarly determined by measuring the distance between cursors placed at the medial tibial plateau and the tibial plafond. When obtaining these measurements, the patient lays supine on the CT scanner tabletop, which moves through a collimated xray beam from a stationary source.
Fig. 6.
An AP CT scanogram of an adult patient following surgical treatment of fractures of the pelvis and right femoral shaft demonstrates a mild (2 mm) LLD in the femoral segment (courtesy of Dr Mark C. Reilly).
Huurman et al. [19] studied in-vitro precision and accuracy of CT scanogram and orthoroentgenogram using adult femoral and tibial specimens that were placed flat on a table top. The accuracy and interobserver variability for both techniques was very similar, with less than 3 mm difference in measurement, compared to the actual length of the specimens that was measured using calipers. However, when the specimens were angled in the vertical plane, the lateral CT scanogram was significantly more accurate (p = 0.005), while the orthoroentgenogram underestimated length related to apparent foreshortening of the bone. Aaron et al. [1] compared orthoroentgenography and lateral CT scanogram for assessing LLD using 10 adult lower limb cadaveric specimens at four predetermined degrees of knee flexion of 0, 15°, 30°, and 45°. They reported no significant difference between the actual length of the measured specimen and that assessed by the lateral CT scanogram for all measurements, while the orthoroentgenogram was less accurate in measuring length of the tibia and the entire limb in specimens with knee flexion of 30° or greater. Moreover, the radiation dose with the CT scanogram was 80% less than that delivered during the orthoroentgenogram. The length of time required to complete the imaging and cost was comparable for the two radiographic evaluation methods. Temme et al. [41] compared the measurements of CT scanogram and orthoroentgenogram using dried femur specimens and also found the CT scanogram more accurate. Aitken et al. [2] compared AP CT scanogram using a scout view and conventional scanogram using plain radiography in 24 patients (18 children, six adults). All studies were evaluated by two radiologists independently and revealed high correlation (r = 0.99) for both techniques. While no statistical differences in measurements were found between the two imaging techniques, there was a trend for underestimation of length by 2 mm using the CT scan in patients with bony segments that were greater than 30 cm long. The cost of the two studies was similar although the radiation dose was three to six times less with the CT scan compared to a scanogram. Porat and Fields [32] compared the accuracy of conventional orthoroentgenography with CT scanogram for measuring LLD in 17 patients and reported similar accuracy of both techniques with a 66% reduction in radiation dose with a CT scanogram. Badii et al. [5] reviewed pelvic asymmetry based on the AP scout view of abdominal CT scans in 323 patients. Pelvic asymmetry ranged from −11 to 7 mm. Pelvic asymmetry greater than 5 mm was found in 17 (5.3%) and greater than 10 mm in two (0.6%) of the patients. Based on assessment of 30 CT scans by three examiners, the interobserver reliability of measuring pelvic asymmetry on abdominal CT scans was high (ICC, 0.91).
MRI Scan
Although traditionally used for soft tissue imaging, MRI has become an increasingly popular method to evaluate bony abnormalities as well. MRI images were obtained using a T1 weighted spin echo sequence and the best coronal images were selected for standardized assessment of femoral length using the classic bony landmarks of the femoral head and medial femoral condyle [25].
In a recent study, Leitzes et al. [25] compared MRI scanogram with CT and radiographic scanogram using 12 cadaveric femoral specimens to assess the potential for assessing LLD. Three orthopaedists with different levels of training performed two separate measurements using each technique. Accuracy was also assessed by comparing the measurements obtained with the imaging techniques and true measurement of the femoral length using an electronic caliper. The intraobserver and interobserver reliability was very high (ICC, 0.99) for all three techniques and all examiners. However, compared to the true length of the femur, the mean absolute difference was 0.52 mm for the radiographic scanogram, 0.68 mm for the CT scanogram, and 2.90 mm for the MRI scanogram.
Discussion
While there are several different methods available to the clinician for the assessment of LLD, we were unable to find an in-depth review of the various clinical and imaging modalities as the subject of a single manuscript. Our goal was to enumerate the various modalities that have been described for assessing leg length discrepancy, including the accuracy and interobserver and intraobserver reliability for each technique, to compare the reported results for various assessment tools for LLD, and discuss the potential advantages and pitfalls that have been described with each method. We identified certain trends that were noted across several studies discussed below, along with the potential advantages and pitfalls of each method.
While using a tape measure is an easy, safe, and noninvasive means of assessing LLD, it is less reliable when compared to radiographic techniques such as a scanogram [7, 8, 10, 43]. The average of two tape measurements of the distance between the ASIS and medial malleolus appears to have acceptable validity and reliability when used as a screening tool for assessing LLD [14]. However, there are potential sources of error with tape measurements related to differences in leg circumference, angular deformities, and difficulty in accurately palpating bony prominences as well as joint contractures. While the use of standing blocks under the short leg to level the pelvis is slightly more reliable than tape measurement, such a method may still not be precise enough for serial monitoring of LLD [43].
There is general consensus that radiographs are more accurate and reliable than clinical exam for analysis of LLD [8, 24, 43]. Several authors have reported the results of LLD measurement using a variety of imaging techniques such as orthoroentgenogram [13], CR-based teleoroentgenogram [38], slit scanogram [28], microdose digital radiography [3], CT scanogram [1, 2, 19], ultrasound [42], and MRI scanogram [25]. One needs to consider several issues such as reliability, accuracy, magnification, radiation dose, cost, need for special equipment, convenience, and opportunity to image the entire extremity when choosing the imaging technique for evaluating patients presenting with LLD (Table 1).
Table 1.
Comparison of methods for assessing leg length discrepancy
| Methods | Reliability* | Accuracy* | Magnification | Approximate radiation exposure (mrads) [26] | Approximate charges (U.S. dollars) | Radiographic deformity analysis | Incorporation of height of the foot and pelvis | Typical availability in U.S. | Weight bearing |
|---|---|---|---|---|---|---|---|---|---|
| Clinical | |||||||||
| Supine tape measure—“Real” (ASIS to malleolus) | + | + | None | None | Office visit | Not applicable | No | Yes | No |
| Supine tape measure—“Apparent” (umblicus to malleolus) | + | + | None | None | Office visit | Not applicable | Partial | Yes | No |
| Standing blocks | + + | + | None | None | Office visit | Not applicable | Yes | Yes | Yes |
| Imaging | |||||||||
| Teleoreontgenogram | + + + + | + + + | ~5% | 42 | $95 [26] | Yes | Yes | Varies | Yes |
| Orthoroentgenogram | + + + | + + + | Minimal | 200 | $110 [26] | Minimal | No | Varies | No |
| Scanogram | + + + + | + + + | Minimal | 200 | $110 [26] | No | No | Varies | No |
| CR | + + + + | + + + | Varies with technique (scanogram versus teleoroengenogram) | Varies with technique, less exposure than standard radiography | $137 [38] | Varies with technique (scanogram versus teleoroengenogram) | Varies with technique | Varies | Varies with technique (scanogram versus teleoroengenogram) |
| MDR | + + + | + + + + | None | 2 | $75 [26] | Yes | Yes | No | Yes |
| Ultrasound | + + + | + + | None | None | Not reported | No | No | No | Yes |
| CT scan (digital localization image) | + + + + | + + + + | Minimal | 60 | $60 [26] | Minimal | None | Varies | No |
| MRI | + + + + | + + + | Minimal | None | Not reported | Not reported | Not reported | No | No |
CR = computed radiography; MDR = microdose digital radiography.
* Please see text for detailed analysis. For simplicity, the increasing number of “+” signs indicate greater degree of reliability/accuracy.
A scanogram is one of the most commonly used methods for assessing LLD. It has excellent reliability [37] and minimal, if any, magnification error [38]. However, as supine radiographs that require the patient to remain still between the three radiographic exposures, an orthoroentogenogram and a scanogram are prone to errors related to the patient moving between the exposures. The radiation exposure with scanogram and orthoroentgenogram is also substantially greater than that associated with a full-length standing radiograph and a CT scanogram [1, 26, 38]. This may be related to the need for three separate radiographic exposures with the scanogram and orthoroentgenogram compared to the single exposure centered at the knee with the standing radiograph as well as the closer xray tube-to-patient distance utilized while performing a scanogram. While taking a scanogram, the xray tube must be centered precisely over the joint since even a minor deviation of the beam can result in measurement error of several millimeters due to distortion by magnification [26]. Errors in measurement are often seen in patients with clinically important limb-length inequalities when the individual joints of the two limbs are at substantially different levels and thus not visualized on the same radiograph [26]. Moreover, a scanogram cannot detect angular deformities of the lower limb and may underestimate the LLD in patients with discrepancies in foot height [26, 38]. Patients presenting with unequal leg lengths often have associated angular deformities of the lower limb. Since the entire lower extremity is imaged on a single radiograph with the patient in the erect position, a comprehensive analysis of limb deformities can be performed as well, along with the assessment of LLD [26, 38, 39]. Furthermore, unlike a scanogram, the difference in height of the feet is incorporated in the measurement of LLD when using the full-length standing radiograph. There are certain prerequisites that should be met in order to avoid potential errors in using this measurement for clinical decision making. For the standing full-length radiograph, the patient should be stood erect with the pelvis clinically level and the feet plantigrade by using an appropriate-sized lift under the short limb. This will avoid underestimation of the LLD that can occur with the patient plantarflexing the ankle on the short side and flexing the contralateral knee in an attempt to level the pelvis. Similarly, any lower extremity joint contractures or overlying external fixators can diminish the accuracy of LLD measurement using either of the two imaging techniques [36]. However, there are potential pitfalls with using this radiograph, including the need for special radiographic equipment such as grids, filters, and processors along with the need for long radiographic cassettes that may not be readily available with recent advances in digital imaging and can be difficult to store.
Computed radiography (CR) does not require these additional tools while at the same time uses standard radiographic equipment. The full-length images obtained using CR are readily available on personal computers for preoperative planning and patient/ family education [26, 38]. Despite a 5% magnification “error” in the measurement of the entire length of the lower extremity, there is minimal effect on assessment of LLD. Furthermore, by placing magnification markers and a ruler next to the patient, this magnification error can be further reduced (Fig. 7). Proper training and supervision of the radiology technicians regarding the correct technique and patient positioning for performing standing radiographs, especially with rapidly changing technology, is also critical to ensure appropriate and reproducible imaging studies.
Fig. 7.

A standing full-length computed radiograph (modified teleoroentgenogram) of a 14 year old patient following right sided tibial lengthening for a 6 cm LLD. Note the use of a midline ruler and magnification markers adjacent to the right hip, knee and ankle joints to decrease the magnification error in measuring the residual LLD in this child. Use of a small lift under the right leg to level the pelvis may also have been useful.
The cost of microdose digital radiography (MDR) is comparable to other imaging techniques [3, 26], although special equipment is necessary. Moreover, unlike a CT scan, the digital scan has a field length of 150 cm that is sufficient for imaging the entire lower extremity in a single exposure for most patients [3]. However, this technique is not readily available and not as convenient as a full-length standing AP radiograph that is obtained using computed radiography.
The benefits of ultrasound are that it is inexpensive, does not involve any radiation exposure, is reliable in the hands of experienced users, and is thus a convenient and useful method of assessing LLD [22, 23]. However, unlike a full-length standing radiograph, an ultrasound does not allow for a comprehensive analysis of the lower extremity including angular deformities and may be less accurate than radiographic methods. This technique may be a useful screening tool in the hands of experienced users [42].
A CT scanogram has the advantages of displaying the entire lengths of the femurs and tibias while minimizing the measurement error. There is no magnification when the structure to be measured is centered in the computerized axial tomographic gantry [19]. While possibly needing longer setup time, a CT scanogram has similar costs and may be more accurate, with excellent reliability and less gonadal radiation, than some of the plain radiographic techniques [1, 2, 17, 19, 26, 41]. In order to avoid underestimation of limb length, it may also be useful to perform a lateral CT scanogram in patients with flexion contractures of the hip or knee [1, 19]. However, periarticular and diaphyseal angular deformities as well as joint subluxation and mechanical axis deviations are not as well ascertained on these supine images compared to a standing radiograph. Moreover, this technique is not readily available and usually requires prior scheduling in the department of radiology or an imaging center.
Although an MRI scanogram does not expose patients to ionizing radiation, the measurements obtained using this technique are slightly less accurate than those obtained with a radiographic scanogram or a CT scanogram [25]. Furthermore, an MRI scanogram has not been well-studied in the clinical setting as an assessment tool for LLD, is probably more expensive, may require sedation in some children, typically requires a longer time to schedule and to complete the study, and may be contraindicated in patients with certain implantable devices. Thus, at this time a supine MRI scanogram remains an investigational tool that requires clinical validation before it can be recommended for general use. Recently, MRI scanners that allow the patient to weight bear during imaging have been introduced in the U.S. market. Such an emerging technique may be an attractive option to comprehensively assess length and alignment of the lower extremities while avoiding radiation exposure to the patient.
Based on our review of the literature, we found several limitations in the available articles dealing with different assessment tools for LLD. The majority of the studies were retrospective case series with multiple confounding variables that were not clearly stated by the investigators. Factors such as magnitude of LLD, level of training and experience of observers, lack of blinding of observers, undocumented body habitus (such as BMI) of subjects, presence of angular deformities and contractures, use of cadaveric and synthetic bone specimens versus live subjects as well as limited number of patients can affect the validity of the authors’ conclusions. Certainly, there are ethical concerns with subjecting patients to multiple diagnostic modalities, especially those involving radiation. However, future investigators can strengthen their research methodology by employing more robust study design and methodology. Our suggestions would include the following: use well-designed prospective, multicenter studies involving a larger number of subjects, clearly state and discuss the confounding variables, perform appropriate statistical analysis, perform adequate tests for reliability and accuracy amongst blinded observers with different levels of training and study emerging technologies that do not involve radiation hazards, such as standing MRI and ultrasound. Hopefully, such efforts can further aid clinicians in performing safe, reliable and accurate assessment of patients presenting with LLD.
An ideal method for assessing LLD should be readily available, accurate, reliable, and affordable, allow visualization of the entire lower extremity, minimize radiation exposure, and have no magnification error. Although at present there is no single imaging method that can be considered ideal, based on our review of the literature, the standing full-length AP computed radiograph of both lower extremities with the pelvis level, along with use of a magnification marker, should be the primary imaging modality for the initial evaluation of LLD in the majority of the patients. A CR teleoroentgenogram is not only an accurate and reliable imaging tool, but the measurements can be obtained with limited radiation exposure in a cost-effective manner [20, 21]. However, other techniques such as a lateral scout CT scan may be more useful in cases with severe angular deformities, especially those associated with flexion deformities around the knee. In the upcoming years other imaging modalities such as a standing MRI of the lower extremities may prove a viable alternative, without exposing patients to radiation hazards. On the other hand, despite rapidly advancing technology, it is important to consider that the accuracy and ease of obtaining measurements of the patient using any imaging modality is not a substitute for a thorough clinical assessment of the patient presenting with LLD [18]. Moreover, clinical evaluation of the patient with long-standing limb shortening, especially with associated muscle weakness, using blocks under the short limb can be used to estimate the amount of correction that feels optimal, as this may be different from the true LLD assessed with an imaging modality. Thus, a judicious use of a comprehensive imaging method combined with an astute clinical assessment is the most optimal means of evaluating a patient presenting with leg-length discrepancy.
Acknowledgments
We thank Dr. Caixia Zhao and Ms. Emily McClemens, PA-C, for their assistance in preparing this manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Aaron A, Weinstein D, Thickman D, Eilert R. Comparison of orthoroentgenography and computed tomography in the measurement of limb-length discrepancy. J Bone Joint Surg Am. 1992;74:897–902. [PubMed]
- 2.Aitken GF, Flodmark O, Newman DE, Kilcoyne RF, Shuman WP. Mack LA. Leg length determination by CT digital radiography. AJR Am J Roentgenol. 1985;144:613–615. [DOI] [PubMed]
- 3.Altongy JF, Harcke HT, Bowen JR. Measurement of leg length inequalities by Micro-Dose digital radiographs. J Pediatr Orthop. 1987;7:311–316. [DOI] [PubMed]
- 4.Aspegren DD, Cox JM, Trier KK. Short leg correction: a clinical trial of radiographic vs. non-radiographic procedures. J Manipulative Physiol Ther. 1987;10:232–238. [PubMed]
- 5.Badii M, Shin S, Torreggiani WC, Jankovic B, Gustafson P, Munk PL, Esdaile JM. Pelvic bone asymmetry in 323 study participants receiving abdominal CT scans. Spine. 2003;28:1335–1339. [DOI] [PubMed]
- 6.Baylis WJ, Rzonca EC. Functional and structural limb length discrepancies: evaluation and treatment. Clin Podiatr Med Surg. 1988;5:509–520. [PubMed]
- 7.Beattie P, Isaacson K, Riddle DL, Rothstein JM. Validity of derived measurements of leg-length differences obtained by use of a tape measure. Phys Ther. 1990;70:150–157. [DOI] [PubMed]
- 8.Cleveland RH, Kushner DC, Ogden MC, Herman TE, Kermond W, Correia JA. Determination of leg length discrepancy. A comparison of weight-bearing and supine imaging. Invest Radiol. 1988;23:301–304. [DOI] [PubMed]
- 9.Defrin R, Ben Benyamin S, Aldubi RD, Pick CG. Conservative correction of leg-length discrepancies of 10 mm or less for the relief of chronic low back pain. Arch Phys Med Rehabil. 2005;86:2075–2080. [DOI] [PubMed]
- 10.Fisk JW, Baigent ML. Clinical and radiological assessment of leg length. N Z Med J. 1975;81:477–480. [PubMed]
- 11.French SD, Green S, Forbes A. Reliability of chiropractic methods commonly used to detect manipulable lesions in patients with chronic low-back pain. J Manipulative Physiol Ther. 2000;23:231–238. [DOI] [PubMed]
- 12.Glass RB, Poznanski AK. Leg-length determination with biplanar CT scanograms. Radiology. 1985;156:833–834. [DOI] [PubMed]
- 13.Green WT, Wyatt GM, Anderson M. Orthoroentgenography as a method of measuring the bones of the lower extremities. J Bone Joint Surg Am. 1946;28:60–65. [PubMed]
- 14.Gurney B. Leg length discrepancy. Gait Posture. 2002;15:195–206. [DOI] [PubMed]
- 15.Hanada E, Kirby RL, Mitchell M, Swuste JM. Measuring leg-length discrepancy by the “iliac crest palpation and book correction” method: reliability and validity. Arch Phys Med Rehabil. 2001;82:938–942. [DOI] [PubMed]
- 16.Harris I, Hatfield A, Walton J. Assessing leg length discrepancy after femoral fracture: clinical examination or computed tomography? ANZ J Surg. 2005;75:319–321. [DOI] [PubMed]
- 17.Helms CA, McCarthy S. CT scanograms for measuring leg length discrepancy. Radiology. 1984;151:802. [DOI] [PubMed]
- 18.Horsfield D, Jones SN. Assessment of inequality in length of the lower limb. Radiography. 1986;52:223–227. [PubMed]
- 19.Huurman WW, Jacobsen FS, Anderson JC, Chu WK. Limb-length discrepancy measured with computerized axial tomographic equipment. J Bone Joint Surg Am. 1987;69:699–705. [PubMed]
- 20.Jonson SR, Gross MT. Intraexaminer reliability, interexaminer reliability, and mean values for nine lower extremity skeletal measures in healthy naval midshipmen. J Orthop Sports Phys Ther. 1997;25:253–263. [DOI] [PubMed]
- 21.Kogutt MS. Computed radiographic imaging: use in low-dose leg length radiography. AJR Am J Roentgenol. 1987;148:1205–1206. [DOI] [PubMed]
- 22.Konermann W, Gruber G. Ultrasound determination of leg length [in German]. Orthopade. 2002;31:300–305. [DOI] [PubMed]
- 23.Krettek C, Koch T, Henzler D, Blauth M, Hoffmann R. A new procedure for determining leg length and leg length inequality using ultrasound. II: Comparison of ultrasound, teleradiography and 2 clinical procedures in 50 patients [in German]. Unfallchirurg. 1996;99:43–51. [PubMed]
- 24.Lampe HI, Swierstra BA, Diepstraten AF. Measurement of limb length inequality. Comparison of clinical methods with orthoradiography in 190 children. Acta Orthop Scand. 1996;67:242–244. [DOI] [PubMed]
- 25.Leitzes AH, Potter HG, Amaral T, Marx RG, Lyman S, Widman RF. Reliability and accuracy of MRI scanogram in the evaluation of limb length discrepancy. J Pediatr Orthop. 2005;25:747–749. [DOI] [PubMed]
- 26.Machen MS, Stevens PM. Should full-length standing anteroposterior radiographs replace the scanogram for measurement of limb length discrepancy? J Pediatr Orthop B. 2005;14:30–37. [DOI] [PubMed]
- 27.Merrill OE. A method for the roentgen measurement of the long bones. Am J Roentgenol Radium Ther Nucl Med. 1942;48:405–406.
- 28.Millwee RH. Slit scanography. Radiology. 1937;28:483–486.
- 29.Moseley CF. Leg length discrepancy. In: Morrissy RT, Weinstein SL, eds. Lovell and Winter’s Pediatric Orthopedics. Philadelphia, PA: Lippincott Williams & Wilkins; 2006;1213–1256.
- 30.Okun SJ, Morgan JW Jr, Burns MJ. Limb length discrepancy: a new method of measurement and its clinical significance. J Am Podiatry Assoc. 1982;72:595–599. [DOI] [PubMed]
- 31.Petrone MR, Guinn J, Reddin A, Sutlive TG, Flynn TW, Garber MP. The accuracy of the Palpation Meter (PALM) for measuring pelvic crest height difference and leg length discrepancy. J Orthop Sports Phys Ther. 2003;33:319–325. [DOI] [PubMed]
- 32.Porat S, Fields S. Limb length discrepancy determined by computerized tomography and radiography [in Hebrew]. Harefuah. 1989;116:515–516. [PubMed]
- 33.Rhodes DW, Mansfield ER, Bishop PA, Smith JF. Comparison of leg length inequality measurement methods as estimators of the femur head height difference on standing Xray. J Manipulative Physiol Ther. 1995;18:448–452. [PubMed]
- 34.Rhodes DW, Mansfield ER, Bishop PA, Smith JF. The validity of the prone leg check as an estimate of standing leg length inequality measured by Xray. J Manipulative Physiol Ther. 1995;18:343–346. [PubMed]
- 35.Rondon CA, Gonzalez N, Agreda L, Millan A. Observer agreement in the measurement of leg length. Rev Invest Clin. 1992;44:85–89. [PubMed]
- 36.Sabharwal S, Badarudeen S, McClemens E, Choung E. The effect of circular external fixation on limb alignment. J Pediatr Orthop. 2008;28:314–319. [DOI] [PubMed]
- 37.Sabharwal S, Zhao C, McKeon J, Melaghari T, Blacksin M, Wenekor C. Reliability analysis for radiographic measurement of limb length discrepancy: Full-length standing anteroposterior radiograph versus Scanogram. J Pediatr Orthop. 2007;27:46–50. [DOI] [PubMed]
- 38.Sabharwal S, Zhao C, McKeon JJ, McClemens E, Edgar M, Behrens F. Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph comared with scanogram. J Bone Joint Surg Am. 2006;88:2243–2251. [DOI] [PubMed]
- 39.Saleh M, Milne A. Weight-bearing parallel-beam scanography for the measurement of leg length and joint alignment. J Bone Joint Surg Br. 1994;76:156–157. [PubMed]
- 40.Shapiro F. Pediatric Orthopedic Deformities. Basic Science, Diagnosis, and Treatment. San Diego, CA: Academic Press; 2001;606–732.
- 41.Temme JB, Chu WK, Anderson JC. CT scanograms compared with conventional orthoroentgenograms in long bone measurement. Radiol Technol. 1987;59:65–68. [PubMed]
- 42.Terjesen T, Benum P, Rossvoll I, Svenningsen S, Floystad Isern AE, Nordbo T. Leg-length discrepancy measured by ultrasonography. Acta Orthop Scand. 1991;62:121–124. [DOI] [PubMed]
- 43.Terry MA, Winell JJ, Green DW, Schneider R, Peterson M, Marx RG, Widmann RF. Measurement variance in limb length discrepancy: Clinical and radiographic assessment of interobserver and intraobserver variability. J Pediatr Orthop. 2005;25:197–201. [DOI] [PubMed]
- 44.Tokarowski A, Piechota L, Wojciechowski P, Gajos L, Kusz D. Measurement of lower extremity length using computed tomography [in Polish]. Chir Narzadow Ruchu Ortop Pol. 1995;60:123–127. [PubMed]