Abstract
Objective: To determine the effects of tilt-in-space seating on outcomes for people with neurological or neuromuscular impairment who cannot walk.
Data sources: Search through electronic databases (MEDLINE, Embase, CINAHL, AMED). Discussions with researchers who are active in field.
Review methods: Selection criteria included interventional studies that investigated the effects of seat tilt on outcome or observational studies that identified outcomes for those who had used tilt-in-space seating in populations with neurological or neuromuscular impairments. Two reviewers independently selected trials for inclusion, assessed quality and extracted data.
Results: Nineteen studies were identified which fulfilled the selection criteria. Seventeen of these were essentially before–after studies investigating the immediate effects of tilting the seating. All studies looked at populations with neurological impairment, and most were on children with cerebral palsy (n = 8) or adults with spinal cord injury (n = 8).
Reviewer's conclusion: Posterior tilt can reduce pressures at the interface under the pelvis.
Introduction
Tilt-in-space wheelchairs and seats are increasingly used by people with neurological or neuromuscular impairments who cannot walk. Tilt-in-space systems may be considered for a variety of reasons, including low sitting tolerance or discomfort, a requirement to rest in the seat, and to assist with manual handling.1 Drawbacks to these systems compared with conventional wheelchairs and seats include purchase costs, size and complexity of equipment. Tilt-in-space wheelchairs are also heavier and less manoeuvrable than more standard wheelchairs due to a longer wheelbase, and this may restrict access to transport.2
A backwards-tilted sitting position has been suggested to improve head and trunk posture,3,4 and to reduce the loading under the buttocks5–7 or through the spine.8 There are concerns that seating that is excessively tilted back limits communication, upper limb function and the ability to stand up from the chair.9
A forward-tilted sitting position has also been proposed to maintain lumbar lordosis, decrease posterior pelvic tilt, reduce the effect of tight hamstrings on the position of the pelvis and to position a person within reach of the desk or table.10,11 Forward-tilted positions have been incorporated into some paediatric seating.12
With no evidence-based criteria or guidelines for provision and use of these systems, practices around the provision of tilt-in-space seating systems vary widely. Tilt-in-space seating may be provided by statutory service in some areas. Systems are also available for purchase directly by the user.
In a qualitative study2 of severely disabled wheelchair users with multiple sclerosis and significant spasticity themes such as wheelchair size and manoeuvrability, transport difficulties, comfort, pressure ulcers, sitting up during day for prolonged periods and fatigue emerged from in-depth interviews. Seven tilt-in-space and 16 conventional wheelchair users participated.
With this background it was thought that a systematic review on the effects of tilt-in-space seating might inform clinical practice on seating provision and use within these populations, and identify what further research studies on this topic are required in order to establish evidence-based guidelines for provision.
Objective
To identify the effects of seat orientation on physiology; body parts and systems; and on activity for adults and children with neurological or neuromuscular impairments who cannot walk.
Method
Search strategy
A search was carried out in December 2006 of electronic databases including MEDLINE (1950–2006), Embase (1980–2006), CINAHL (1982–2006), AMED (1985–2006) using thesaurus terms ‘wheelchair’, ‘wheelchairs’, ‘seat’, ‘seating’ and free text words ‘tilt$’ and ‘tip$’ looking for articles in English on humans. Reference lists in studies and review articles were examined for other appropriate articles. A search for unpublished studies was conducted via contact with experts in the field.
Selection criteria
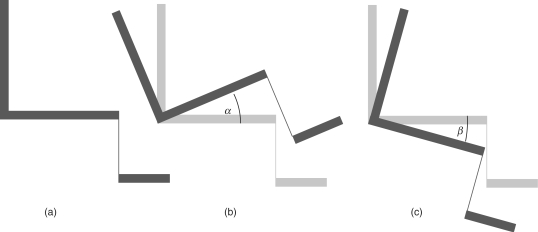
Studies were identified that investigated the effects of seat tilt on outcome for the seated individual. Experimental studies that compared outcomes at different angles of tilt were included as were observational studies that compared outcomes for those that had used tilt-in-space seating to those that had used a seat in a fixed orientation. A tilt of the seat was taken to be a rotation of the complete seat about a mediolateral axis, and tilt angle is as described in Figure 1.
Figure 1.
Schematic lateral views of seat showing (a) upright, (b) posteriorly and (c) anteriorly tilted seat orientations. α = posterior tilt angle, β = anterior tilt angle.
Studies with both randomized and non-randomized allocation of subjects to seat or seat orientation were selected for review.
Studies included only participants who were non-ambulant and who had a congenital or acquired neurological or neuromuscular condition. Participants could be of any age.
Any outcome was considered that described the effects of seat tilt on physiology; body parts and systems; and on human activity including fulfilment of societal roles.
Data collection and analysis
The two reviewers independently selected trials for inclusion, assessed quality and extracted data.
The methodological strength of each study was evaluated using a commonly used hierarchy of study designs from the NHS Centre for Reviews and Dissemination.13 Methodological strength was graded on a scale from 1 to 5 where 1 is the highest level (Table 1).
Table 1.
Levels of evidence13
| Level | |
|---|---|
| 1 | Experimental study (e.g. RCT with concealed allocation) |
| 2 | Quasi-experimental study (e.g. experimental study without randomization) |
| 3 | Controlled observational study: (a) cohort study, (b) case–control study |
| 4 | Observational study without control group |
| 5 | Expert opinion based on pathophysiology, bench research or consensus |
Quality was also assessed in addition to methodological strength. This was based on: whether the study was properly controlled; what methods of randomization or allocation to intervention groups were used; and whether the groups were comparable at baseline. The roles of chance, confounding and bias in the study were also considered. Attempts were made to contact authors to obtain any important data that were missing and necessary for the review.
The studies included in this systematic review were not only randomized control trials. This is because studies have tended to focus on instantaneous outcomes as a result of being tilted compared with upright and alternative designs have often been used (e.g. cross-over trials). However, in appraising such studies particular attention was given to identifying potential sources of bias. Cross-over trials could be rated at levels 1, 2, 4 or 5 depending on samples size and homogeneity; whether the effects of order, timing and knowledge of the intervention on outcome were controlled and validity of outcome measures.
A generally descriptive analysis was selected as most appropriate for the research question, because of the heterogeneity of the studies that were identified. However, a meta-analysis was also carried out involving published and unpublished results from five studies which looked specifically at body/support interface pressure under the ischial tuberosities. A more conservative random effect model was used rather than a fixed effect model due to the presence of heterogeneity across the studies.14
It was not possible to directly combine all the data in one meta-analysis as two of the studies15,16 had reported measurements taken from the same participants while sitting on different cushion configurations and therefore the data sets were not considered truly independent of one another. However two separate meta-analyses were carried out, using the results for specific cushions in each study corresponding to the best and worse case scenarios (i.e. most and least pressure reduction).
Results
Of the 389 publications identified in the electronics database searches, only 15 fulfilled the selection criteria (Appendix 1). An additional five publications were identified by other means. Two publications referred to the same study.
Nineteen studies were identified (Table 2). All of the studies were on populations with neurological impairment. Ten of the studies were on young people: with cerebral palsy (n = 8), neural tube defect (n = 1), or unspecified neurological impairment (n = 1). Nine of the studies were on adults: with spinal cord injury (n = 8) or multiple sclerosis (n = 1).
Table 2.
Summary of methods
| Ref. | Study design | Participants | Type of seat | Tilt angles | Timing and order of tilt | Comments | Evidence level |
|---|---|---|---|---|---|---|---|
| (a) Studies involving posterior tilt | |||||||
| 3 | Case study | 1, 9-year old with CP | Wheelchair including head rest, lateral and anterior trunk support, foot support. 90° seat-to-back angle | 0°, 15° and 30° posterior tilt | 10 sessions with 20 min at each tilt angle in variable order | 5 | |
| 4 | 1: Cross-over study | 10 adults with MS | Same manual wheelchair | 0° and 25° posterior tilt | 15 min upright then 15 min tilted | 4 | |
| 2: RCT | 20 adults with MS | 0° and 25° or 45° posterior tilt | Upright then tilted. No acclimatization period | Subjects randomly assigned to 25° or 45° tilt angle | 2 | ||
| 5, 20 | Cross-over study | 12 adults with complete SCI | Reclining/tilting wheelchair with seat cushion, arm and foot rests. 100° seat-to-back angle | 0°, 10° and 20° posterior tilt | Set order for testing positions. 15 min acclimatization in each position | 6 other positions tested within session | 4 |
| 6 | Cross-over study | 2 adults with C5 quadriplegia | Subjects’ own wheelchairs with 100° seat-to-back angle | 0°, 35° and 45° posterior tilt | Single session with set order for positions: 0°, 35°, 45° and 0° (repeated) | 2 other positions tested. Repeated on 3 seat cushions | 5 |
| 7 | Cross-over study | 15 children (7–18 years) with myelo- meningocele | Chair with back and head rest, foam cushion on base, 90° seat-to-back angle | 0° and 25° posterior tilt | Randomized order for positions with each position repeated twice. 30 seconds data collection in each position | 3 other positions also tested | 2 |
| 15 | Cross-over study | 16 adults, SCI, motor complete tetraplegia | Subjects’ own powered wheelchairs. 95° median seat-to-back angle | 5° median and 45° posterior tilt | Upright for 1 min, then tilted for 1 min | Repeated on 2 seat cushions. Inter-subject position variations | 4 |
| 16 | Cross-over study | 18 adults with complete SCI (C5–L2) | Powered wheelchair with 90° seat-to-back angle | 5°, 15° and 25° posterior tilt | 3 sessions with all conditions tested in random order in session. 15 seconds in each condition | Testing repeated at 3 cushion inflation pressures | 2 |
| 17 | Cross-over study | 11 children (4–8 years) with spastic CP | 90° seat-to-back angle, head rest, lateral trunk supports, adductor wedge; foot rest | 0° and 150 posterior tilt | Single session with random order to positions. 3 min acclimatization in each position | 5 other positions also tested | 2 |
| 19 | Cross-over study | 20 adults with complete thoracic SCI | Chair with back and foot rests, 100° seat-to-back angle | 0°, 7° and 12° posterior tilt | Single session with random tilt order. Each position repeated twice | 1 other position tested. Subjects undertook reaching task during measurement | 2 |
| 21 | Cross-over study | 14 adults, C6-T10 motor complete SCI | E&J Premier (upright) and Quickie Breezy 500 (4° posterior tilt) wheelchairs. 90° seat-to-back angle | 0° and 4° posterior tilt | Single session, with random order for testing chairs. Time in chairs not specified | Additional differences between wheelchairs. Chair with acute seat-to-back angle also tested | 4 |
| 25 | Cross-over study | 10 adults with SCI | Subjects’ own wheelchair with seat cushion | 0°, 35° and 65° posterior tilt | Single session with set order for positions: 0°, 35°, 65° | Another position also tested | 4 |
| 27 | Cross-over study | 12 children (6–18 years) with CP (spastic diplegia) | As in ref. 18. Hip abductor also included | 0° and 30° posterior tilt | Single session with random tilt order. 5 min acclimatization in each position | 2 | |
| 29 | Cross-over study | 6 children with spastic CP, mean age 6 years | Upholstered seat base, foot rests. No back rest nor arm rests | 0° and 10° anterior tilt | 2–3 min acclimatization, 5 min upright 5 min tilted. Repeated at 3 sessions | Subjects independent sitters and ambulatory | 4 |
| (b) Studies involving anterior and posterior tilt | |||||||
| 22 | Case series | 23 children with CP (2–16 years) | Range of seats, providing foot, pelvic and trunk support. Seat-to-back angle ranging from 9° to 130° | 0–30° posterior (mean 8°) and 0–15° anterior tilt (mean 8°) | Single session with random order to positions and 5 min in each position | Tilt angles varied between subjects. Seats also varied between subjects and tilts. Repeated with table and abductor | 5 |
| 24 | Cross-over study. | 10 children with spastic CP | 90° seat-to-back angle, head rest, lateral trunk supports, chest panel, foot rest | 0°, 15°, 30° posterior and 15° anterior tilt | Random order to tilt positions, then repeated in reverse order. 5 min acclimatization in each position | 3 children with athetoid CP also measured (analysed separately) | 2 |
| 28 | Cross-over study | 10 children with spastic CP (4–15 years) | Chair with back rest and foot support. 90° seat-to-back angle changed to 95° for anterior tilt | 0°, 5° posterior and 5° anterior tilt | 3 sessions with one randomly selected tilt angle per session | Measurements during ‘quiet sitting’ and during upper extremity activity | 2 |
| (c) Studies involving anterior tilt | |||||||
| 18 | Cross-over study | 15 children (2–6 years) with developmental delay and/or CP | Adjustable bench with non-skid surface | 0°, 20° and 30° anterior tilt | Single session of 30 min. Random order for testing positions with 1 min acclimatization in each position | 2 other positions/seats measured. Limited control over bench postures | 4 |
| 26 | Cross-over study | 20 adults with complete thoracic SCI | Chair with flat/ramped seat base, foot support, and support behind trunk. | 0° and 10° anterior tilt | Single session. Upright then tilted | Base only tilted. Subjects undertook reaching task | 4 |
| 23 | Cross-over study | 14 children with CP (5–11 years) | Upholstered seat base, foot rests. No back rest nor arm rests | 0°, 10° and 15° anterior tilt | Four 20-minute sessions each at 2 tilt angles (0–10°, 10–0°, 0–15°, 15–0°) | Subjects independent sitters and ambulatory | 2 |
CP, cerebral palsy; MS, multiple sclerosis; SCI, spinal cord injury.
The seat was tilted anteriorly by up to 30° in three of the studies, was tilted posteriorly by up to 45° in 13 studies and was tilted in both directions in three studies.
Several studies included additional interventions. Additional seat configurations and postures were included in the studies of Nwaobi et al.17 Miedaner,18 Pellow,6 Vaisbuch et al.,7 Janssen-Potten et al.19 and Hobson.5,20 The seat cushions also varied in the studies of Burns and Betz15 and Spijkerman et al.,16 who examined effects on interface loading. Hastings et al.21 compared three designs of wheelchair, two of which had different, fixed tilt angles. Myhr and von Wendt22 compared postures in individuals’ own seats with postures in an alternative seat which was adjusted to provide a more forward-inclined position.
Seventeen of the studies were essentially cross-over trials comparing seat orientation (Table 2). Myhr and von Wendt's study22 can be considered as a series of case reports because of the range of seats and orientations involved in the intervention. In another study3 a single child was seated at three angles of tilt. In the second part of Chan and Heck's study4 subjects were randomly assigned to two groups that were tilted back to two different angles of tilt.
In 10 studies the order of tilt was randomized at each measurement session. Two studies23,24 looked at ordering effects by repeating the measurements in a reverse order and comparing outcomes. In one study the full set of seat positions were measured over multiple sessions23. In the other studies all seat positions seemed to be measured in a single session. The measurement period in each position varied between a few seconds to 20 minutes. It was not possible to blind the subject or the researcher to the intervention(s) in any of the studies.
Outcomes included: interface pressure,5–7,15,16,20,25 shear force,5,20 surface EMG,17,19,23,26,27 postural measurements,4,18,21,23,26 change in head position23,28, timed upper extremity activity,24,28 respiratory measurements,4,29 voice volume4 and perceived exertion4 (Table 3).
Table 3.
Evidence of effect in studies: outcomes measures
| Ref. | Outcome measure | Tilt away from vertical | Mean change with tilt from vertical | Significance level reported (P = 0.05) |
|---|---|---|---|---|
| Interface loading | ||||
| 5, 20 | Maximum pressure under ischial tuberosities | 20° posterior tilt | −11% | Yes [in ref. 20] |
| Tangential shear force through seat | −85% | Yes [in ref. 20] | ||
| 6 | Pressure at ischial tuberosities and sacrum (averaged over the 3 locations, mean over 1 minute of measurements) | 45° posterior tilt | −34% | Not reported (2 participants) |
| 7 | Maximum interface pressure | 25° posterior tilt | −22% | Yes (P < 0.01) |
| Mean interface pressure (mean of 2 measurements) | −8% | No | ||
| 15 | Pressure under ischial tuberosity (side of highest pressure, mean of 10 measurements) | 45° posterior tilt | −33% | Yes (P < 0.001) |
| 16 | Maximum pressure under right ischial tuberosity; average for 3 cushion inflation pressures, 3 measurements at each | 20° posterior tilt | −5% | Yes (P = 0.012) |
| 25 | Pressure over ischial tuberosities, mean over 1 minute of measurements | 35° posterior tilt | −27% | No |
| Posture and stability | ||||
| 4 | Thoraco-lumbar distance | 25° posterior tilt | +3% | No |
| Cervico-thoracic distance | −36% | Yes | ||
| 21 | Thigh length (indirect measure of pelvic tilt), shoulder position and head orientation from photographs | 14° posterior tilt | −1.1−1.6 cm, +6.5°, respectively | No |
| 28 | Mean displacement of the head,# shoulder,# hip knee, ankle | 5° posterior tilt, 5° anterior tilt | Variable. Maximum change was 4 cm increase | Yes# (in some segments with anterior tilt) |
| 26 | Sagittal pelvic orientation | 10° anterior tilt | <2° more anterior. Variable | No |
| 18 | Distance from pelvis to spinous process | 30° anterior tilt | −8% | Yes |
| 23 | Sitting height | 15° anterior tilt | −0.21 cm | No |
| Radius of head position (stability) | −0.97 cm | Yes (P = 0.037) | ||
| Muscle activity | ||||
| 17 | EMG (lumbar erector spinae) | 15° posterior tilt | + 37% | No |
| 19 | EMG (erector spinae at T3, T9 and L3, serratus anterior,† oblique abdominals,† pectoralis major,† latissumus dorsi,† trapezius) | 12° posterior tilt | Variable. Increased in some groups. Decrease in others | Yes† in some muscles and injury levels, no for others |
| 27 | EMG (iliocostalis lumborum, adductor magnus and gastrocnemius) | 30° posterior tilt | +51, +19, +1%, respectively | Yes (back and hips) |
| 23 | EMG (erector spinae, average from four bilateral paraspinal sites) | 15° anterior tilt | +73% | Not reported |
| 26 | EMG (erector spinae at T3,* T9* and L3,* oblique abdominals, serratus anterior, pectoralis major, latissumus dorsi, trapezius*) | 10° anterior tilt | Up to −50% depending on anatomical location and level of injury | Yes* in some muscles and injury levels, no for others |
| Respiratory function | ||||
| 4 | Forced vital capacity | 25° posterior tilt | +20% | Yes (P < 0.001) |
| Chest expansion | +7% | Yes (P = 0.014) | ||
| 29 | Tidal volume, respiration rate, minute ventilation | 10° anterior tilt | +12, +3, +3%, respectively | No |
| Other functional activity | ||||
| 19 | Maximum unsupported forward reach distance | 12° posterior tilt | <5 cm difference | No |
| 3 | Time with head directed to activity | 15° posterior tilt | +22% | Not reported |
| 4 | Voice volume | 25° posterior tilt | −0.1% | No |
| Perceived exertion on Borg's scale of 6–20 | −4.96% | No | ||
| 24 | Timed switch use with upper extremity | 30° posterior 15° anterior tilt | +39%, +44%, respectively | Yes Yes |
| 28 | Upper extremity activity (6 timed tasks) | 5° posterior 5° anterior tilt | Improved in 1 of 6 tasks in each tilt condition | Yes for only 1 task No for 5 tasks. |
| 22 | Time with head upright | 0–15° anterior tilt (mean 8°) | +93% mean duration | Yes (P = 0.001) |
| Sitting assessment score 5–20 | +56% median score | Yes (P = 0.001) | ||
| Number of pathological movements | −75% median number | Yes (P = 0.002) | ||
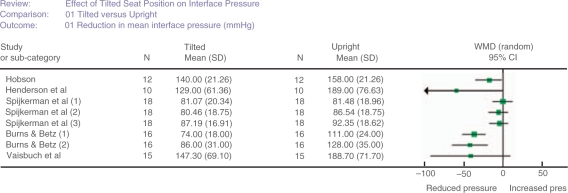
Meta-analysis of interface pressure
Figure 2 shows a forest plot for five of the six studies that investigated interface pressure under the ischial tuberosities.5,7,15,16,25 It was not possible to include Pellow's study6 as insufficient data were reported and there were only two participants. Spijkerman's16 unpublished data were used in the analysis and it was necessary to make a conservative calculation of the standard deviation from the reported significance level for Hobson's study.5,20 Multiple results shown for particular studies15,16 relate to the use of different seat cushions. An inspection of Figure 2 suggests a reduction in interface pressure when participants were posterior tilted (between 20° and 45°) compared with upright.
Figure 2.
Forest plot showing results of studies investigating body/support interface pressure under the ischial tuberosities. The participants in the studies by Hobson5,20 and Vaisbuch et al.7 were sitting on foam seat cushions while the participants in the study by Henderson et al.25 remained sitting on their own personal cushions. Spijkerman et al.16 used dry flotation seat cushions and repeated measurements with the same participants sitting on cushions inflated to 20 mmHg (1), 30 mmHg (2) and 40 mmHg (3). Burns and Betz15 repeated measurements with participants sitting on a dry flotation seat cushion (1) and a gel seat cushion (2).
The worst case scenario in terms of pressure reduction suggested a reduction of 24.00 (95% confidence interval (CI) 4.19–43.80) mmHg (P = 0.02). The best case scenario was a reduction of 24.80 (95% CI 7.16–42.44) mmHg (P = 0.006).
Discussion
The restriction of the search to papers written in English may have limited the findings of the review. The comparative difficulty in identifying unpublished studies compared to published work may also have limited the findings.
Wide search criteria were used in the systematic review because there was not thought to be much evidence available on the effects of tilted positions. Therefore selection included studies on a range of populations, interventions, experimental methodologies and outcomes.
Studies on different populations (spinal cord injury and neural tube defect) and at different tilt angles were included in the meta-analysis. There were insufficient data to rigorously test the validity of this strategy.
Studies included in the meta-analysis were randomized7,16 and non-randomized5,15,25 trials where participants acted as their own controls. Ideally the order of tilt orientation should have been randomized in all the studies that were included in the meta-analysis as this would remove a potential source of bias.
Experimental design
Most of the studies were cross-over trials looking at the immediate effects of seat orientation on the seated person. With a cross-over experimental design there is potential for tilt order to affect outcome due to fatigue and other physiological responses. Tilt order will also affect outcome if there are changes to the baseline sitting posture during the experimental procedure due to sliding in the seat. In a cross-over study it is feasible to control the effects of order of tilt through experimental design. Measurement at different tilt angles may take place in different sessions. Alternatively, the tilt sequence may be randomized across the sample or the measurements at each tilt angle may be repeated in a different order. These approaches are recommended in future cross-over studies.
It is also possible for knowledge of the seat orientation during the experimental protocol to affect the outcome. Unfortunately it is not practical to blind the subject or experimenter to the orientation of the seat.
The quantitative studies which compared outcomes on different seats (or at different tilt angles) involved small samples of fewer than 20 people. There is potential for actual differences between tilt angles or seats not to be identified as significant because of the distribution of data within the small samples (a type II error). As the number of reported results increase, there will be scope for additional meta-analysis.
In some of the studies on the effects of an anterior seat tilt the intervention comprised a forward tilt of the seat base without additional support about the pelvis or trunk.18,23,26 The variation in findings between studies may be because protocols did not control for other influences on posture.
The number of seating systems on the market providing an anterior tilt is limited, and such seating is not widely used. This may be due to difficulties using these systems in vehicle transport and using them with desks and powered mobility systems. For this reason an investigation into the effects of forward tilt may not be the highest priority for the next stage of research.
No cohort studies were identified which investigated longer term effects of tilt-in-space usage with a quantitative methodology. This approach may be worth considering for future work.
Outcomes
Outcomes measures in most of the studies were related to abnormality of anatomical structure or function (impairment). There was little consideration of the importance of any differences that were identified to the health or social participation of the user.
Six studies reported that tilting the seat back reduced the pressure under the ischial tuberosities in a range of conditions. However the sample sizes involved in the above studies were relatively small and the methods of statistical analysis and levels of significance (when reported) varied noticeably. Pooling data across five of these studies in a meta-analysis produced more robust evidence of a statistically significant reduction in pressure under the ischial tuberosities when participants are tilted backward compared to when upright.
Hobson's5,20 finding of reduced frictional shear stress underneath the seat base with a 200 posterior tilt, is consistent with a generalized biomechanical analysis of a seated person.30
Loading at the interface with the seat is likely to influence susceptibility to pressure ulcers and comfort during sitting. A cohort study on pressure ulcer prevalence in tilt-in-space wheelchair users compared with in a control group of conventional wheelchair users would identify whether the reduction in loading when tilted backwards results in reduced pressure ulcer prevalence for tilt-in-space users.
Studies in different muscle groups and in the cerebral palsy and spinal cord-injured populations have reported that EMG activity in some muscle groups is affected by tilt.19,26,27 In populations and muscle groups where raised activity restricts functional movements and leads to the development of contractures, decreased activity may be advantageous. Reduced muscle activity may also be associated with reduced effort during movements or with the maintenance of position. However in other populations and circumstances, increased muscle activity may be associated with increased functional movements and improved posture. Overall, the effect of seat tilt on EMG activity and how that affects functional outcomes has not been established.
Postural measurements were either between anatomical markers, or between an anatomical marker and the seat surface and were focused on trunk and head position in the sagittal plane. In the studies where measurements were taken from photographs or video frames21,28 there was potential for error from neglected out-of-plane components of position. The postural results overall were inconclusive (Table 3).
Head control has been assessed from measurements23,28 of head position over time. Sochaniwskyj23 used a potentiometric linkage, however the measurements were not set into a functional context. Head control has also been assessed from observations of head position over time,3,22 but in Myhr and von Wendt's study22 the inter-rater reliability of the observers was reported for only two of six positions and ranged from 0.9 to 0.31 using Spearman's rank correlation coefficient.
Ability to perform an activity from the seat is a key aspect of any study on the effects of seat tilt. Nwaobi24 used timed switch operation and McClenaghan et al.28 used timed tasks as measures of upper extremity function. Myhr and von Wendt 22 evaluated hand and arm function using observational techniques and a rating scale. Respiratory measurements were included as an outcome in only two of the studies identified by this review. Reid and Sochaniwsky29 made indirect measurements of tidal volume via plethysmography whereas Chan and Heck4 took measurements of vital capacity using lung function spirometry. Additional studies on capabilities in tilted postures for specific populations would be worth while.
No studies on ability to transfer into and out of the seat were identified in the populations of interest. Studies on other more ambulatory populations31 have suggested that ability to independently transfer may be reduced by a posteriorly tilted position. However many people within the populations that are covered by this review have to use a hoist to transfer into and out of the seat, so the effect should be investigated separately.
Effects within populations
No studies were identified on the effects of seat tilt on people with progressive neuromuscular conditions (e.g. muscular dystrophy). This population would benefit from study, as the question of whether to provide a tilt facility on a wheelchair is a common clinical issue.
The studies with cerebral palsy were on young people and tended to measure posture and muscle activity. However it was not possible to identify consistent finding from these studies due to variation in interventions, outcome measures and heterogeneity of the population. The use of the Gross Motor Function Classification System32 in future investigations to identify the participants’ level of physical ability would enable clinicians to judge the advantages and disadvantages of varying angles of tilt for specific children.
Most of the studies in populations with spinal cord injury and neural tube defect were on the effects of seat tilt on interface loading. This is an important outcome in populations that are prone to pressure ulcers.
The only quantitative study that was identified was one on people with multiple sclerosis by Chan and Heck.4 Themes which emerged from in-depth interviews2 with this population included prolonged sitting up during day and fatigue. Chan and Heck4 attempted to identify the immediate effects of a change in orientation on fatigue using Borg's Rating of Perceived Exertion scale. However, the increase in fatigue with tilt that was identified is likely to be affected by their protocol, which involved a fixed order of tilt.
Previous cohort studies on how fatigue, duration of sitting, other health and social factors are affected by long-term use of a tilted position have not been identified. Future cohort studies on tilt-in-space seat usage, compared with standard seat usage would greatly inform clinical practice.
Clinical messages.
Evidence is lacking on the effects of tilted seat positions on health, function and participation outcomes.
Studies on progressive neurological/neuromuscular populations are particularly scarce.
There is some evidence to suggest a posterior seat tilt reduces pressures under the pelvis for people with neurological impairment.
Conclusions
Results from studies on populations with spinal cord injury and neural tube defect suggest that a posterior seat tilt of 20° or more reduces pressures under the pelvis.
Overall there is a lack of quality evidence to support and guide the use of the tilted position in seating for populations with neurological and neuromuscular impairment. Current evidence is weakened by mixed interventions and confounding factors. Outcome measures, participants and interventions need to be determined more rigorously to ensure that confounders do not reduce the quality and usefulness of future studies.
A priority area for future studies might be effect of posterior seat tilt on functional activity and seat use, in populations with progressive neuromuscular conditions.
Competing interests
None declared.
Appendix 1 Literature search: main terms and publications identified
| Total found | New publications selected | Duplicates | ||
|---|---|---|---|---|
| 1 | Wheelchairs/and tilt$.mp (MEDLINE, CINAL, AMED) | 57 | 9 | 0 |
| 2 | Wheelchair/and tilt$.mp (Embase) | 42 | 1 | 8 |
| 3 | Seat/and tilt$.mp (Embase) | 31 | 2 | 4 |
| 4 | Seating/and tilt$.mp (CINAL, AMED) | 28 | 0 | 6 |
| 5 | Sitting/and tilt$.mp (Embase, CINAL, AMED) | 116 | 0 | 5 |
| 6 | Wheelchairs/and tip$.mp, (MEDLINE, CINAL, AMED | 39 | 2 | 0 |
| 7 | Wheelchair/and tip$.mp (Embase) | 30 | 0 | 1 |
| 8 | Seat/and tip$.mp (Embase) | 6 | 0 | 1 |
| 9 | Seating/and tip$.mp, (CINAL, AMED) | 4 | 1 | 1 |
| 10 | Sitting/and tip$.mp (Embase, CINAL, AMED) | 36 | 0 | 3 |
| Hand search of reference lists, consultation with experts in the field | – | 5 | – |
References
- 1.Lacoste M, Weiss-Lambrou R, Allard M, Dansereau J. Powered tilt/recline systems: why and how are they used? Assist Technol. 2003;15:58–68. doi: 10.1080/10400435.2003.10131890. [DOI] [PubMed] [Google Scholar]
- 2.Dewey A, Rice-Oxley M, Dean T. A qualitative study comparing the experiences of tilt-in-space wheelchair use and conventional wheelchair use by clients severely disabled with multiple sclerosis. Br J Occup Ther. 2004;67:65–74. [Google Scholar]
- 3.Angelo J. Using single-subject design in clinical decision making: the effects of tilt-in-space on head control for a child with cerebral palsy. Assist Technol. 1993;5:46–49. doi: 10.1080/10400435.1993.10132206. [DOI] [PubMed] [Google Scholar]
- 4.Chan A, Heck CS. The effects of tilting the seating position of a wheelchair on respiration, posture, fatigue, voice volume and exertion outcomes in individuals with advanced multiple sclerosis. J Rehabil Outcomes Meas. 1999;3:1–14. [Google Scholar]
- 5.Hobson DA. Comparative effects of posture on press and shear at the body-seat interface. J Rehabil Res Dev. 1992;29:21–31. doi: 10.1682/jrrd.1992.10.0021. [DOI] [PubMed] [Google Scholar]
- 6.Pellow TR. A comparison of interface pressure readings to wheelchair cushions and positioning: A pilot study. Can J Occup Ther. 1999;66:140–49. doi: 10.1177/000841749906600306. [DOI] [PubMed] [Google Scholar]
- 7.Vaisbuch N, Meyer S, Weiss PL. Effect of seated posture on interface pressure in children who are able-bodied and who have myelomeningocele. Disabil Rehabil. 2000;22:749–55. doi: 10.1080/09638280050200241. [DOI] [PubMed] [Google Scholar]
- 8.Ham R, Aldersea P, Porter D. Wheelchair users and postural seating. first. Churchill Livingston; 1998. [Google Scholar]
- 9.Pountney TE, Mulcahy CM, Clarke SM, Green EM. The Chailey approach to postural management. second. Chailey Heritage Clinical Services; 2004. [Google Scholar]
- 10.Bendix T, Biering-Sorensen F. Posture of the trunk when sitting on forward inclining seats. Scand J Rehabil Med. 1983;15:197–203. [PubMed] [Google Scholar]
- 11.Mandal AC. The correct height of school furniture. Physiotherapy. 1984;70:48–53. [PubMed] [Google Scholar]
- 12.Pope PM, Bowes CE, Booth E. Postural control in sitting. The Sam system: evaluation of use over three years. Dev Med Child Neurol. 1994;36:241–52. doi: 10.1111/j.1469-8749.1994.tb11837.x. [DOI] [PubMed] [Google Scholar]
- 13.NHS Centre for Reviews and Dissemination. York (UK): University of York; 2001. Undertaking systematic reviews of research effectiveness, CRD Report No. 4. [Google Scholar]
- 14.Khan KS, Kunz R, Kleijnen J, Antes G. Systematic reviews to support evidence-based medicine. Royal Society of Medicine Press; 2003. pp. 54–55. [Google Scholar]
- 15.Burns SP, Betz KL. Seating pressures with conventional and dynamic wheelchair cushions in tetraplegia. Arch Phys Med Rehabil. 1999;80:566–71. doi: 10.1016/s0003-9993(99)90201-0. [DOI] [PubMed] [Google Scholar]
- 16.Spijkerman DCM, Terburg M, Goossens RHM, Stijnen T. Effects of inflation pressure and posture on the body-seat interface pressure of spinal cord injured patients seated on an air-filled wheelchair cushion. J Rehabil Sci. 1995;8:8–12. [Google Scholar]
- 17.Nwaobi OM, Brubaker CE, Cusick B, Sussman MD. Electomyographic investigation of extensor activity in cerebral-palsied children in different seating positions. Dev Med Child Neurol. 1983;25:175–83. doi: 10.1111/j.1469-8749.1983.tb13741.x. [DOI] [PubMed] [Google Scholar]
- 18.Miedaner JA. The effects of sitting positions on trunk extension for children with motor impairment. Pediatr Phys Ther. 1990;2:11–14. [Google Scholar]
- 19.Janssen-Potten YJ, Seelen HA, Drukker J, Reulen JP. Chair configuration and balance control in persons with spinal cord injury. Arch Phys Med Rehabil. 2000;81:401–408. doi: 10.1053/mr.2000.3859. [DOI] [PubMed] [Google Scholar]
- 20.Hobson DA. PhD thesis. University of Strathclyde; 1988. Contributions of posture and deformity to the body-seat interface conditions of a person with spinal cord injuries. [Google Scholar]
- 21.Hastings JD, Fanucchi ER, Burns SP. Wheelchair configuration and postural alignment in persons with spinal cord injury. Arch Phys Med Rehabil. 2003;84:528–34. doi: 10.1053/apmr.2003.50036. [DOI] [PubMed] [Google Scholar]
- 22.Myhr U, von Wendt L. Improvement of functional sitting position for children with cerebral palsy. Dev Med Child Neurol. 1991;33:246–56. doi: 10.1111/j.1469-8749.1991.tb05114.x. [DOI] [PubMed] [Google Scholar]
- 23.Sochaniwskyj A, Koheil R, Bablick K, Milner M, Lotto W. Dynamic monitoring of sitting posture for children with spastic cerebral palsy. Clin Biomech. 1991;6:161–67. doi: 10.1016/0268-0033(91)90028-O. [DOI] [PubMed] [Google Scholar]
- 24.Nwaobi OM. Seating orientations and upper extremity function in children with cerebral palsy. Phys Ther. 1987;67:1209–12. doi: 10.1093/ptj/67.8.1209. [DOI] [PubMed] [Google Scholar]
- 25.Henderson JL, Price SH, Brandstater ME. Efficacy of three measures to relieve pressure in seated persons with spinal cord injury. Arch Phys Med Rehabil. 1994;75:535–39. [PubMed] [Google Scholar]
- 26.Janssen-Potten YJ, Seelen HA, Drukker J, Huson T, Drost MR. The effect of seat tilting on pelvic position, balance control, and compensatory postural muscle use in paraplegic subjects. Arch Phys Med Rehabil. 2001;82:1393–402. doi: 10.1053/apmr.2001.25989. [DOI] [PubMed] [Google Scholar]
- 27.Nwaobi OM. Effects of body orientation in space on tonic muscle activity of patients with cerebral palsy. Dev Med Child Neurol. 1986;28:41–44. doi: 10.1111/j.1469-8749.1986.tb03828.x. [DOI] [PubMed] [Google Scholar]
- 28.McClenaghan BA, Thombs L, Milner M. Effects of seat-surface inclination on postural stability and function of the upper extremities of children with cerebral palsy. Dev Med Child Neurol. 1992;34:40–48. doi: 10.1111/j.1469-8749.1992.tb08561.x. [DOI] [PubMed] [Google Scholar]
- 29.Reid DT, Sochaniwskyj A. Effects of anteriorly-tipped seating on respiratory function of normal children and children with cerebral palsy. Int J Rehabil Res. 1991;14:203–13. doi: 10.1097/00004356-199109000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Goossens RHM, Snijders CJ. Design criteria for the reduction in shear forces in beds and seats. J Biomech. 1995;28:225–30. doi: 10.1016/0021-9290(94)00052-6. [DOI] [PubMed] [Google Scholar]
- 31.Alexander NB, Koester DJ, Grunawalt JA. Chair design affects how older aldults rise from a chair. J Am Geriatr Soc. 1996;44:356–62. doi: 10.1111/j.1532-5415.1996.tb06402.x. [DOI] [PubMed] [Google Scholar]
- 32.Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]