Abstract
Previous research has demonstrated that older adults prefer less autonomy and seek less information when making decisions on their own relative to younger adults (for a review, see Mather, 2006). Would older adults also prefer fewer options from which to choose? We tested this hypothesis in the context of different decision domains. Participants completed a choice preferences survey in which they indicated their desired number of choices across six domains of healthcare and everyday decisions. Our hypothesis was confirmed across all decision domains. We discuss implications from these results for theories of aging and healthcare policy.
Keywords: Aging, Choice, Decision Making, Preferences
“…we're going to provide a prescription drug benefit, and as we do, we're going to give seniors more choices and more options from which to choose.”
-- Pres. George W. Bush, Feb 17, 2006
“I'm 85, do I have to go through this nonsense? I'm trying to absorb all the information, but it's ridiculous. Not just ridiculous, it's scary. If there was a single card and it was administered by Medicare, and it got the cost of drugs down -- wonderful, marvelous.”
--Senior citizen (cited in Leland, 2004)
November 15, 2005 marked the beginning of what was undoubtedly the largest pseudo-experiment ever conducted on decision-making among an aging population: Forty-three million older adults already enrolled in Medicare were given the opportunity under the nascent Medicare Part D program to select a prescription drug care plan from dozens of alternatives.1 The average number of options increased to 42 in 2006, and continued to grow (to 55 choices) in the following year (Simon, 2007), prompting headlines such as “Medicare Part D: Tyranny of Choice” (Oakland Tribune, 2006) to appear in the popular press. Remarkably, of the 43 million individuals eligible to enroll in Medicare Part D, only slightly more than half of them (22.5 million) had received coverage within seven months of the program's inception (Kaiser, 2006). Moreover, among these 22.5 million, it is likely that only less than half (a little over 10 million) actually made an active decision to enroll in a plan, while a little less than half that number (4.4 million) did not make a choice and remained uninsured for prescription drugs. How could so many seniors fail to sign up for prescription drug plans when there were dozens of options from which to choose? And how likely are those who did sign up for a plan to have preferred less choice than was presented to them?
The proliferation of options appeared to stem from a tacit assumption, as illustrated by the above quote, that older adults would surely benefit (both financially and psychologically) from having more choice. Indeed, the notion that ample choice is not only beneficial to our well-being, but also an essential component of modern life, seems deeply ingrained in the conscience of American society. To be clear, there is support for the value of choice in enhancing our sense of identity and individualism (e.g. Markus & Kitayama, 1991), and, according to advocates of rational choice theory, having more options should lead to objectively better decisions (e.g. see Payne, Bettman, & Johnson, 1993). However, mounting evidence suggests that choice, when excessive, may impair the subjective quality of decisions.
Having too many options not only undermines decision satisfaction, but may also sap our motivation to choose (for a review, see Botti & Iyengar, 2006). For example, Iyengar and Lepper (2000) demonstrated in a series of experiments that individuals who choose from “excessive” choice sets (24 or 30 options) in a range of domains (from chocolates to optional essays) are significantly less likely to commit to a choice and express less satisfaction with their choices than people who select from a relatively limited set (6 options). This inverse relationship between choice and well-being has been dubbed the “paradox of choice” by Schwartz (2000, 2004), who suggested three potential mechanisms whereby excessive choice undermines satisfaction: Inflated expectations or standards, an enhanced sense of personal responsibility for poor outcomes, and excessive difficulty in acquiring and processing information about alternatives. And, although the latter mechanism would seem especially relevant to older adults given age-related declines in working memory capacity (see, e.g., Reuter-Lorenz & Sylvester, 2005), we know of no study that has explored the impact of excessive choice on this age group.
Additionally, to our knowledge, there is no research directly examining whether older adults actually desire as much choice as is provided to them. However, converging evidence of age-related declines in preferred choice autonomy and information-seeking in decision making (for a review, see Mather, 2006) suggest that choice preference should decline with age. For example, older adults report more deferential tendencies and desire less responsibility when making hypothetical healthcare decisions than younger adults (Finucane, Slovic, Hibbard, Peters, Mertz, & MacGregor, 2002). Moreover, when older adults make decisions independently, they seek less information than younger adults and rely more on heuristic strategies (Johnson, 1990). Older adults show this pattern of reduced information-seeking even with regard to decisions that should be of greater personal relevance, such as medical decisions. For instance, when faced with a hypothetical patient's choice of whether to begin Estrogen Replacement Therapy, older women were significantly less likely than younger women to seek a second opinion or gather additional information (Zwahr, Park, & Shifren, 1999). Insofar as added choices entail more information, we expect that older adults would desire fewer choices.
In addition to increasing the amount of information in a decision, added choices may also enhance the likelihood of experiencing regret with one's decision (Schwartz, 2000). According to the theoretical perspective of Schwartz, as the number of options increase so do the perceived tradeoffs (opportunity costs) and expectations for decision quality, both of which may lead to negative affect associated with one's choice (i.e. regret and dissatisfaction). This mechanism seems especially relevant in the context of aging, given prior research findings that older adults' decision strategies, relative to those of younger adults, may serve emotion regulatory goals. According to Socioemotional Selectivity Theory (SST), younger adults are more likely to pursue knowledge-related goals and engage in information seeking, whereas older adults are more likely to pursue emotionally meaningful goals and engage in emotion regulation (Carstensen, Fung, & Charles, 2003). In particular, older adults' regulation strategies are marked by optimization of positive affect and minimization of negative affect leading to an age-related positivity effect (Carstensen & Mikels, 2005). For example, older adults attend to and recall more positive versus negative information than younger adults in decision tasks (Mather, Knight, & McCaffrey, 2005; Löckenhoff & Carstensen, 2007). One avenue by which older adults engage in emotion regulation is through selective information search, as illustrated by Mather et al. (2005) and Löckenhoff and Carstensen (2007). However, another means of preventing potential negative affect in decision-making may be through restricting the choice set. As such, one would expect younger adults to desire more choice (insofar as more choice represents more information), whereas older adults would desire less choice, so as to preserve their satisfaction.
Present Study
While there is ample evidence of age-related changes in decision making style and motivation, we know of no research that has examined how the amount of desired choice varies with age, nor how it varies within age by type of decision. The present study addressed this empirical gap by directly questioning older and younger adults about their ideal level of choice in a variety of domains. Given converging evidence from research on cognitive and motivational aspects of older adults' decision making, we predicted that they would desire fewer options than younger adults. However, in light of the apparent lack of prior research findings or theory regarding domain specificity in preferred choice, we remained agnostic about whether there would be a difference in the degree of choice desired between different domains.
Method
Participants
Ninety-nine undergraduates at Cornell University, aged 18-24 (M = 19.72 years, SD = 1.29) participated in exchange for course extra credit. One hundred and two older adults aged 60-94 years (M = 78.36 years, SD = 7.65) recruited from two senior centers in New York City received ten dollars each for their participation. There was no difference in years of education between younger adults (M = 13.56, SD = .97) and older adults (M = 12.97, SD = 3.46); t(1, 184) = -1.63, n.s.
Materials and Procedure
Participants completed a series of pen-and-paper questionnaires, which included demographic measures and a choice preferences survey. The choice preferences survey asked participants to indicate their desired number of choices in six domains. Half of the domains (prescription drug plans, physicians, and hospitals) involved healthcare and the other half (cars, apartments, and jams) involved everyday decisions. Participants indicated the number of options that they would like to have available for each of the decision domains. Additionally, for each of the domains participants were asked to predict from a list of choice sets (7 sets ranging from 2 options to 26 options in intervals of 4) which set would make them most satisfied.
Results
Responses to the two choice measures (preferred number of options and number of options for greatest satisfaction) were highly correlated (average r > .7). We thus averaged responses to the two questions to create a composite measure of preferred choice for each domain. All subsequent analyses were conducted on this composite measure of choice.
After observing that the distribution of the composite measure was skewed, we performed a log-transformation to normalize the distribution2. To test our hypothesis that older adults would prefer fewer choices across the six decision domains, we conducted a repeated-measures multivariate analysis of variance (MANOVA) on the log-transformed composite measure of choice with age (younger vs. older) as a between-subjects factor and domain type (healthcare vs. everyday) and specific domain (nested within domain type) as within-subjects factors. In order to facilitate interpretation, the means reported below are the raw means, even though the statistical analyses were conducted on log-transformed data.
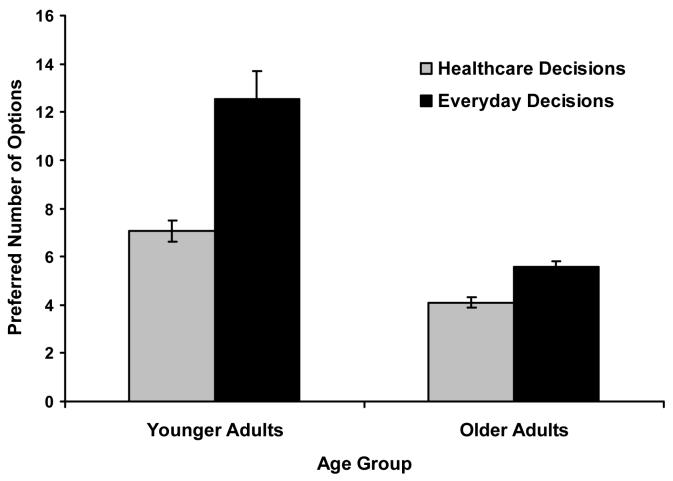
As predicted, older adults preferred significantly fewer options (M = 4.83, SD = 4.12) than younger adults (M = 9.81, SD = 15.16) overall (F(1, 196) = 76.59, p < .001), as well as in each of the six decision domains (see Table 1). To examine the possibility of domain specific effects, we tested differences in preferred number of options between healthcare and everyday domains. As depicted in Figure 1, both older and younger adults preferred significantly fewer options for healthcare decisions (M = 5.59, SD = 5.96) than everyday decisions (M = 9.13, SD = 14.84); F(1, 966) = 180.65, p < .001. However, the gap in preferred choice between healthcare and everyday domains for younger adults exceeded that of older adults; F(1, 966) = 7.22, p < .01.2
Table 1.
Desired number of options for older and younger adults.
| Desired Number of Options | ||||
|---|---|---|---|---|
| Younger | Older | |||
| Domain | Mean | Mean | F | p (2-tailed) |
| Drug Plans | 6.17 (4.71) | 4.22 (3.94) | 21.04 | < .001 |
| Physicians | 9.47 (10.55) | 4.77 (4.16) | 50.46 | < .001 |
| Hospitals | 5.59 (4.33) | 3.60 (3.19) | 24.65 | < .001 |
| Cars | 19.49 (31.02) | 6.04 (5.12) | 118.89 | < .001 |
| Apartments | 9.52 (8.50) | 5.67 (4.30) | 33.94 | < .001 |
| Jams | 8.57 (9.12) | 5.34 (3.89) | 22.63 | < .001 |
Note. Standard deviations are in parentheses
Figure 1.
Mean number of preferred options (+/− SE) by age group and decision domain. There was a significant main effect of age such that older adults preferred fewer options than younger adults, a main effect of domain such that all adults preferred fewer options for healthcare decisions than everyday decisions, and a significant age by domain interaction such that the difference was even greater for younger relative to older adults.
To further investigate the influence of age on the degree of preferred choice and to test the possibility that these differences were simply due to cohort effects, correlational analyses were run within the older adult group.3 As expected, age was negatively correlated with preferred choice for older adults, r = −.45, p < .001.
Discussion
As predicted, older adults preferred significantly less choice than younger adults across six different decision domains in two categories, and even within the older adult group this preference strengthened with age. Additionally, while both age groups preferred fewer options for healthcare decisions than for everyday decisions, we observed a smaller gap between the two domain types for older adults.
Results of the present study raise issues at both the theoretical and applied levels. In the current study, older adults desired (overall) roughly half the number of options that younger adults preferred. Consistent with the work of Iyengar and Lepper (2000) showing increased satisfaction with fewer options and the implications of SST (Carstensen et al., 2003), the reduced choice preference of older adults may reflect the prioritization of emotion regulation. As such, the results of the current study complement those of Lockenhoff and Carstensen (2007) by suggesting an additional means by which older adults may enhance the subjective experience of decision making.
Alternatively, the finding that older adults desire a more manageable amount of choice than their younger counterparts may constitute an adaptive response to the metacognitive recognition of reduced decision making competence. Finucane et al. (2002) reported evidence that older adults rate their abilities in gathering information from tables and charts—skills that may be central to certain forms of complex decision making—lower than younger adults. However, the authors did not examine concordance between these assessments and participants' demonstrated abilities. Thus, while the present findings raise the possibility that older adults may hold more realistic assessments of their decision making abilities than younger adults, additional research would be needed to directly test this implication.
In addition to the predicted main effect of age on choice preference, we also observed an interaction between age and domain type (everyday versus healthcare) such that younger adults demonstrated a greater difference in preferred choice between healthcare and everyday decisions, relative to older adults. This effect may result from differential salience of the domains to the younger and older adults. While everyday domains such as cars and apartments are ostensibly more significant than healthcare decisions for younger adults, the importance of the two domains may be more equated for older adults. However, such a conclusion remains tenuous without direct measures of personal relevance or significance.
As with any study, there are a number of important caveats to keep in mind. First and foremost, given the cross-sectional nature of this study, cohort effects may have influenced our results. Although our samples did not differ in years of education, some of the older adults had not received a college diploma, which most of the younger adults will presumably achieve. And while these potentially discrepant education levels could partially account for the present results, a subset analysis comparing higher-educated older adults with the college student sample yielded similar results to the overall comparison, suggesting that an age-related decline in choice preference exists independently of educational influences. Moreover, the correlational evidence of an age-related decline in preferred choice within the older adult sample further argues against cohort effects. While these safeguards suggest that the results are not entirely driven by cohort effects, without a longitudinal design generational differences may still influence choice preferences. It should be noted, however, that contemporary policy implications of the present study are still highly relevant despite alternate influences to those hypothesized: Today's older adults desire far less choice than is offered to them.
Another potential limitation is that we did not specify how the quality of the options may or may not change with the number of choices when we asked participants about their desired degree of choice. As such, an additional mechanism behind the observed age differences in preferred choice may be diverging intuitions as to the function or correlates of choice. For example, younger adults may believe that greater choice implies higher quality or lower prices for options through market competition, while older adults may not possess such optimistic lay theories of choice. Future research would benefit from directly measuring intuitions about choice or eliminating the potential ambiguity by specifying that the choice sets in question do not differ on cost or quality.
If the hypothetical choice experiment conducted here can be extrapolated to the real-world Medicare Part D decisions that older adults face, these data suggest that the number of prescription drug care plans offered to senior citizens is more than ten times the amount they prefer. In light of previous research on the ill effects of excessive choice (e.g. Botti & Iyengar, 2006; Schwartz, 2000), providing such a large number of drug plan choices to older adults (as happened under Medicare Part D) may actually impair enrollment rates or choice satisfaction, all else held constant. At the outset of this article, we questioned how 4.4 million older adults have failed to choose a heavily subsidized prescription drug plan out of the dozens of plans offered through Medicare Part D. Given the misfit between older adults' choice preferences and the staggering number of Medicare Part D options presented to them, perhaps the real question to ask is how so many older adults (roughly 10 million) succeeded in navigating the sea of choices and selected their plans. While such an answer requires further research, results of the present study highlight a simple reality: For drug plans or jams, 55 choices may be too many, especially for older adults.
Acknowledgments
We thank the Emotion and Cognition Laboratory for assistance with this project. This work was supported by an Innovative Research Project Award from the Bronfenbrenner Life Course Center at Cornell University, and a mini-grant from the Cornell Institute for Translational Research on Aging, an Edward R. Roybal Center for Translational Research funded by the National Institute on Aging (AG022845).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/pag/
Medicare prescription drug coverage was signed into law in December 2003 under the Medicare Modernization Act, and coverage began January 1 2006. Seniors could begin plan selection on November 15th, 2005.
We also tested alternative means of controlling for the skewed distribution, both by omitting outliers in the choice data and recoding them as two standard deviations above the mean. All reported results remained significant for these alternate analyses. Given the equivalence of the three sets of analyses, we reported the log-transformed analyses so as to maintain the integrity of the original raw data as much as possible.
Although these results reveal differences between older and younger adults matched on education, an underlying cohort effect may still be present. Presumably as the younger adults are currently enrolled in college, they will likely achieve a higher level of education than the older adult sample. To safeguard against this possible influence, we conducted a subset analysis comparing the higher-educated older adults to the college students (excluding participants with fewer than 12 years of education), in which no differences emerged from the analysis of the entire sample.
Given the restricted range of ages within the younger cohort, we did not perform a similar test for them.
References
- Botti S, Iyengar SS. The dark side of choice: When choice impairs social welfare. Journal of Public Policy & Marketing. 2006;25:24–38. [Google Scholar]
- Carstensen L, Fung H, Charles S. Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation & Emotion. 2003;27:103–123. [Google Scholar]
- Carstensen LL, Mikels JA. At the intersection of emotion and cognition: aging and the positivity effect. Current Directions in Psychological Science. 2005;14:117–121. [Google Scholar]
- Dijksterhuis A, van Olden Z. On the benefits of thinking unconsciously: Unconscious thought can increase post-choice satisfaction. Journal of Experimental Social Psychology. 2006;42:627–631. [Google Scholar]
- Finucane ML, Slovic P, Hibbard JH, Peters E, Mertz CK, MacGregor DG. Aging and decision-making competence: An analysis of comprehension and consistency skills in older versus younger adults considering health-plan options. Journal of Behavioral Decision Making. 2002;15:441–164. [Google Scholar]
- Iyengar SS, Lepper M. When Choice is Demotivating: Can One Desire Too Much of a Good Thing? Journal of Personality and Social Psychology. 2000;79:995–1006. doi: 10.1037//0022-3514.79.6.995. [DOI] [PubMed] [Google Scholar]
- Johnson MMS. Age differences in decision making: A process methodology for examining strategic information processing. Journal of Gerontology: Psychological Sciences. 1990;45:75–78. doi: 10.1093/geronj/45.2.p75. [DOI] [PubMed] [Google Scholar]
- Leland J. 73 Options for Medicare Plan Fuel Chaos, Not Prescriptions. The New York Times, May 12, 2004. 2004 May 12; Retrieved October 21, 2007, from http://query.nytimes.com/gst/fullpage.html?sec=health&res=9D07E6DA103CF931A25756C0A9629C8B63#.
- Löckenhoff CE, Carstensen LL. Aging, emotion, and health-related decision strategies: Motivational manipulations can reduce age differences. Psychology and Aging. 2007;22:134–146. doi: 10.1037/0882-7974.22.1.134. [DOI] [PubMed] [Google Scholar]
- Markus HR, Kitayama S. Culture and the Self: Implications for Cognition, Emotion, and Motivation. Psychological Review. 1991;98:224–253. [Google Scholar]
- Mather M. A review of decision making processes: Weighing the risks and benefits of aging. In: Carstensen LL, Hartel CR, editors. When I'm 64: Committee on Aging Frontiers in Social Psychology, Personality, and Adult Developmental Psychology. The National Academies Press; Washington, DC: 2006. pp. 145–173. [Google Scholar]
- Mather M, Knight M, McCaffrey M. The Allure of the Alignable: Younger and Older Adults' False Memories of Choice Features. Journal of Experimental Psychology: General. 2005;134:38–51. doi: 10.1037/0096-3445.134.1.38. [DOI] [PubMed] [Google Scholar]
- Tribune Oakland. Medicare Part D: Tyranny of choice. 2006 July 30; [Editorial]. Retrieved October 21, 2007 from http://findarticles.com/p/articles/mi_qn4176/is_20060730/ai_n16654565.
- Payne JW, Bettman JR, Johnson EJ. The Use of Multiple Strategies in Judgment and Choice. In: Castellan NJ, editor. Individual and Group Decision Making. Erlbaum; Mahwah, NJ: 1993. pp. 19–39. [Google Scholar]
- Reuter-Lorenz PA, Sylvester C-YC. The cognitive neuroscience of working memory and aging. In: Cabeza R, Nyberg L, Park DC, editors. Cognitive neuroscience of aging: Linking cognitive and cerebral aging. Oxford University Press; London: 2005. pp. 186–217. [Google Scholar]
- Schwartz B. Self-determination: The tyranny of freedom. American Psychologist. 2000;55:79–88. doi: 10.1037//0003-066x.55.1.79. [DOI] [PubMed] [Google Scholar]
- Schwartz B. The paradox of choice: Why more is less. Ecco; New York: 2004. [Google Scholar]
- Simon KI. Do You Get What You Pay For? The Relationship Between Premiums and Benefits in Medicare Prescription Drug Plans. Cornell University; 2007. Working paper. [Google Scholar]
- The Henry J. Kaiser Family Foundation (KFF Publication No. 7044-05).The Medicare Prescription Drug Benefit - An Updated Fact Sheet. 2006 Retrieved October 21, 2007, from http://www.kff.org/medicare/upload/7044-05.pdf.
- Wilson TD, Lisle D, Schooler J, Hodges SD, Klaaren KJ, LaFleur SJ. Introspecting about reasons can reduce post-choice satisfaction. Personality and Social Psychology Bulletin. 1993;19:331–339. [Google Scholar]
- Zwahr MD, Park DC, Shifren K. Judgments about estrogen replacement therapy: The role of age, cognitive abilities and beliefs. Psychology and Aging. 1999;14:179–191. doi: 10.1037//0882-7974.14.2.179. [DOI] [PubMed] [Google Scholar]