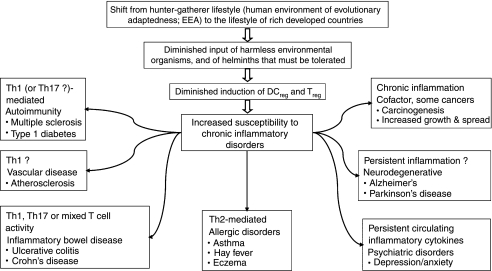
Figure 2.
Pathologies that are increasing, and that might be partly attributable to defective immunoregulation. Human evolution and physiology was shaped by the hunter–gatherer way of life, which is regarded as the human ‘Environment of Evolutionary Adaptedness’ (EEA). Despite increasing human genetic diversity, most human adaptation to novel environments has been cultural and technological rather than genetic, so a gene–environment misfit may be occurring, particularly in the immune system which is not linked to a conscious sensory modality that can warn us of problems. Harmless organisms that were abundant in food and water, and helminths that had to be tolerated, developed a role in the induction of immunoregulatory circuits. Without these there may be a failure to terminate inappropriate inflammatory responses, leading to an increased susceptibility to chronic inflammatory disorders, the precise nature of which depends on the genetics and history of the individual. These disorders may be mediated by T helper type 1 (Th1), Th17 or Th2 lymphocytes, or be mixed, as in ulcerative colitis and Alzheimer's disease, or in individuals with no obvious inflammatory pathology, who have persistently raised circulating cytokines that are associated with depression.