Abstract
Objectives
We examined differential preventive health behavior among grandmothers who recently began raising a grandchild, grandmothers raising a grandchild for at least 2 years, and grandmothers not raising a grandchild.
Methods
Data came from the 2000, 2002, and 2004 waves of the Health and Retirement Study. We ran multivariate logistic regression models to assess receipt of influenza vaccination, cholesterol screening, monthly breast self-exam, mammography, and Papanicolaou (Pap) tests among grandmothers aged 50 to 75.
Results
Grandmothers who recently began raising a grandchild were significantly less likely to report influenza vaccination and cholesterol screening than grandmothers not raising grandchildren, even after we controlled for increased emotional and financial strains within the household. We also observed this association for Pap tests, although this finding was only marginally significant. Grandmothers who had been raising a grandchild for at least 2 years were significantly more likely to report influenza vaccination and monthly breast self-exam than grandmothers not raising grandchildren.
Discussion
The enhancement of preventive behavior seen among long-term grandparent caregivers does not fully offset the suppression of preventive behavior during the transition into care; support groups should target a range of interventions toward the promotion of healthy behavior among new grandparent caregivers.
Keywords: Grandparents Raising Grandchildren, Intergenerational Relations, Preventive Behavior, Health and Retirement Study
RESEARCH has shown that grandparents raising grandchildren are at elevated risk for many health problems, including activity limitation, chronic conditions, and coronary heart disease (Lee, Colditz, Berkman, & Kawachi, 2003; Minkler & Fuller-Thomson, 1999; Strawbridge, Wallhagen, Shema, & Kaplan, 1997). These people are predisposed to poor health outcomes even before care of a grandchild begins due to their generally low socioeconomic status and the difficult family circumstances that precipitated their involvement in care (Hughes, Waite, LaPierre, & Luo, 2007). As custodial grandparents have increased in prevalence nearly twofold since 1970, reaching a total of 2.4 million grandparents (Bryson & Casper, 1999; Simmons & Lawler-Dye, 2003), this group has emerged as an important public health concern. However, little is known about how the assumption of custodial care for a grandchild may influence the health of grandparent caregivers. We propose that raising a grandchild may influence health indirectly through the suppression of healthy behaviors during the initial transition into the caregiving role. In this article, we focus on differential use of preventive behaviors for grandmothers who are not raising a grandchild as compared to long-term grandmother caregivers and those transitioning into the role of custodial grandmother caregiver.
Health and Health Behavior Among Grandmother Caregivers
Because most grandparents provide care to grandchildren in the absence of viable alternative caregivers, a grandparent who becomes unable to care for a grandchild due to health problems may be forced to leave the child in the care of an unreliable parent or place the child in foster care (either temporarily or permanently). Such placements have adverse effects on the well-being of children and impose financial costs on the public sector. Thus, the poor health of caregiving grandparents, in combination with the consequences should they not be able to provide care, makes health maintenance a priority for grandparents raising grandchildren, particularly among grandmothers who play a greater role than grandfathers in providing household maintenance and child care (Coltrane, 2000; Ferree, 1990).
Prior studies have shown that grandparents raising grandchildren have poor health outcomes as compared to noncaregivers (Lee et al., 2003; Minkler & Fuller-Thomson, 1999; Strawbridge et al., 1997). A large part of this discrepancy is likely due to a natural predisposition to poor health outcomes among this group; in other words, because grandparents raising grandchildren tend to be of low socioeconomic status and come from racial/ethnic minority groups, they are likely to experience poor health outcomes well before a grandchild enters their household. There is evidence that once socioeconomic status and demographic characteristics are controlled, grandparents raising grandchildren are no more likely to experience a change in health outcomes as compared to noncaregivers (Hughes et al., 2007). Unfortunately, it is difficult to interpret these findings, as limited longitudinal data are available to examine health change among custodial grandparents. Given that longitudinal data in this area rely on relatively short intervals of time, it is unlikely that experts will observe dramatic shifts in the profiles of morbidity, disability, and mortality among custodial grandmothers. This does not mean that these shifts do not occur; rather, it is possible that raising a grandchild may induce subtle changes in the health behavior of a grandparent that could lead to poor health outcomes later in life.
In order to better understand the influence of raising a grandchild on the health behavior of grandparents, one must first examine the utilization of health services more broadly. According to the health belief model, people reach the decision to perform health behaviors after balancing three factors. People must (a) be motivated to improve or maintain their health, (b) believe that they are susceptible to the condition they are trying to prevent, and (c) acknowledge that the perceived benefits of the behavior outweigh the perceived barriers (Rosenstock, 1966; Rosenstock, Strecher, & Becker, 1988). We propose that raising a grandchild simultaneously influences grandparents' motivation to maintain their health and the perceived barriers to health behavior.
Qualitative research on this topic suggests that there are opposing influences on health behavior among grandmothers raising grandchildren. Custodial caregiving grandparents often do not have time to care for themselves due to the demands of raising a grandchild (Minkler & Roe, 1993). Grandmothers may feel selfish taking time for themselves; instead, they may feel compelled to focus their energy on the grandchild's needs while neglecting their own. In this way, raising a grandchild may influence a grandparent's health by increasing the perceived barriers to preventive behavior. This could lead to a suppression of recommended health behaviors, particularly in the form of missed doctor's appointments (Roe, Minkler, Saunders, & Thomson, 1996). Conversely, grandmothers feel the conflicting need to keep themselves healthy so that they will be prepared to care for the child in the future (Minkler & Roe, 1993). A grandmother who permanently begins raising her infant or toddler grandchild has many years of dependency ahead. If a health crisis prevents a grandmother from being able to provide care, there will be a direct and detrimental effect on the well-being of the grandchild. These factors may influence a grandparent's health by increasing a grandparent's motivation to maintain his or her health. This could lead to an enhancement of recommended health behaviors among grandmother caregivers.
We suggest that these opposing influences operate sequentially. According to the family adjustment and adaptation response model, during periods in which a family's demands outweigh the family's capabilities, the family may be thrust into a period of upheaval known as a crisis (Patterson, 1988, 2002). We suggest that just such a process occurs for grandparents raising grandchildren during the transition into care. When grandparents first begin raising a grandchild, they may be overwhelmed by the demands of care, leading to a decline in preventive health behaviors exacerbated by increased depressive symptoms, worsening financial strain, and, if adjustments are made to work schedules to accommodate the grandchild's schedule, loss of health insurance coverage (Minkler & Roe, 1993). But, over time, grandmothers will develop new strategies to cope with the demands of care, they may be introduced to new resources (such as support groups or public assistance programs), or the demands of care themselves may lessen. This will lead to a period of adaptation during which the family returns to an equilibrium (Patterson, 1988, 2002). As a grandmother adapts to the caregiving role, time constraints may begin to be overshadowed by the grandmother's desire to stay healthy for the sake of her grandchild. A grandmother who is concerned that her grandchild will be placed in foster care if she is no longer physically able to provide care will have strong motivation to maintain a healthy lifestyle and engage in preventive behaviors, a motivation that is not present for other older adults.
Hypotheses
The current study examined preventive health behaviors in a national sample of grandmothers and took timing into account by comparing those who recently began raising a grandchild, long-term grandmother caregivers, and those not raising a grandchild. Specifically, we hypothesized the following:
During the transition into care, grandmother caregivers will experience a temporary decrease in preventive health behaviors; this decrease will not be observed for breast self-exam, as this behavior is performed exclusively within the home and requires minimal time and effort.
This temporary decrease in preventive health behavior will be partially explained by co-occurring changes in depression, financial status, and health insurance coverage.
As a grandmother adapts to raising a grandchild, time constraints may be overshadowed by the grandmother's desire to stay healthy for her grandchild, leading to an increase in healthy behavior, particularly for those health behaviors that require the least time and effort.
METHODS
Participants
Data came from the Health and Retirement Study (HRS), a nationally representative study conducted by the University of Michigan and funded by the National Institute on Aging. We used the Rand HRS data file, an accessible longitudinal version of the HRS, for analysis in combination with family structure variables merged from raw HRS files. We limited the current sample to female respondents between the ages of 50 and 75 who had at least one grandchild, had complete information on the dependent variable, and were interviewed (proxies excluded) in 2000, 2002, and 2004 (N = 5,298). We chose these years for analysis as they represent the only waves during which change in grandparent caregiving status and preventive health behavior were measured during the same time period and for the full sample.
Measures
Reports of preventive behavior were measured in 2004 and represent the respondent's self-report of five types of preventive behavior in the 2 years prior to the survey; therefore, reports provided in 2004 represent behavior occurring between 2002 and 2004. Preventive behavior was assessed by using the following question: “In the last two years, have you had any of the following medical tests or procedures: 1) Flu shot? 2) Blood test for cholesterol? 3) Checked your breasts for lumps monthly? 4) Mammogram or x-ray of the breast? 5) Pap smear?” These behaviors represent the most important and most widely available interventions for detecting and deterring serious diseases in middle-aged and older women. We assessed each as a separate dependent variable in the analyses.
Grandmother caregiver status was assessed with a series of questions to ascertain whether she (and/or her spouse) was raising a grandchild younger than age 18 who was living in the grandmother's household in 2004. We should note that we did not use household headship of the grandparent and parental presence as proxies for custodial care, as is the case with many national samples of grandparent caregivers. Rather, respondents in the HRS are asked to identify any children (beyond their own) whom they are “raising.” We feel that this provides a more accurate representation of custodial grandparents. The identification of grandmother caregivers was anchored primarily on their status in 2004; that is, we coded those who reported raising a grandchild in 2004 as grandmother caregivers, whereas we coded those who did not report raising a grandchild in 2004 as noncaregivers. We subsequently split into two groups grandmothers who reported raising a grandchild in 2004: (a) recent grandmother caregivers—those who reported raising a grandchild in 2004 but not in 2002, and (b) long-term grandmother caregivers—those who reported raising a grandchild in 2002 and 2004. Grandmothers who were not raising a grandchild in 2004 were the reference category. This categorization ensured that the relevant change in household structure overlapped with the time period during which preventive behavior was assessed (i.e., the 2-year period between 2002 and 2004; a more detailed description of our identification of grandparents raising grandchildren using the HRS is in Baker & Silverstein, in press).
Control variables included (a) demographic characteristics: age in years, race/ethnicity (non-Hispanic Black, non-Hispanic other race, and Hispanic vs non-Hispanic White), marital status (1 = married), and labor force participation (working full time, working part time vs not currently working); (b) health and well-being: number of chronic conditions (0-6) and depressive symptoms as measured by the revised 8-item Center for Epidemiologic Studies-Depression scale (0-8; Turvey, Wallace, & Herzog, 1999); (c) socioeconomic status: household income-to-needs ratio (logged) and insurance status (1 = insured); and (d) prior preventive behavior: indicator that the relevant behavior was previously used (1 = yes). All control variables were measured in 2002 with the exception of prior preventive behavior, which was measured in 2000, as the HRS includes the preventive behavior module for the full sample only every other wave.
We also assessed three dynamic variables that may mediate the relationship between caregiving and health behaviors. As a result of entering the caregiving role, grandparents may suffer from increased depressive symptoms, lowered socioeconomic status, and loss of health insurance, each of which will inhibit the use of preventive health practices. Therefore, we examined these changes by using three binary variables indicating the following changes between 2002 and 2004: an increase of at least 2 points on the revised 8-item Center for Epidemiologic Studies-Depression scale, a decrease of at least 0.5 in the household income-to-needs ratio (reduction of half the poverty income for a given household size), and a loss of health insurance between waves.
Analysis
We estimated logistic regression models to examine the effects of grandparent caregiving status on each binary self-reported preventive behavior in 2004. We imputed missing data by using SOLAS 3.2 (as we retained variables imputed by RAND and HRS, the amount of missing data on each variable was minimal; imputations accounted for less than 1% of data on each variable). As we did not impute missing data for the dependent variables, sample size varies between each of the five models. In order to correct for oversampling, we applied weights provided by the HRS. In addition, we used the SVYLOGIT procedure in STATA 9.2 to correct for the multistage area probability sample design of the HRS. As this research looked only at a subgroup of HRS respondents, we used the subpop option to ensure that the calculation of the standard errors was based on all respondents, not just those in the subgroup of interest; this option allows for more accurate estimates of the standard errors but does not affect regression estimates. Given the low power to detect effects in relatively small “treatment groups” of caregiving grandmothers, and the substantial health benefits of preventive practices relative to their costs (particularly with regard to cancer screening) in this population, we discuss trend-level significance (Freiman, Chalmers, Smith, & Kuebler, 1978).
RESULTS
Sample Characteristics
As shown in Table 1, the demographic characteristics, socioeconomic status, and health/well-being of grandmothers who recently began raising a grandchild were quite similar to those of long-term grandmother caregivers. Consistent with prior research, these groups were both disproportionately non-Hispanic Black and Hispanic, were of low socioeconomic status, and showed above average levels of chronic conditions and depression. Despite these similarities, the groups reported dramatically different levels of preventive behavior in 2004. Only 40% of recent grandmother caregivers received an influenza vaccination in 2004 as compared to nearly 60% of long-term caregivers. Similarly, around 60% of recent caregivers received a cholesterol screening whereas more than 80% of long-term caregivers received this test. Turning to a comparison with grandmothers not raising a grandchild, both recent and long-term grandmother caregivers showed dramatic differences from this group in demographic characteristics, socioeconomic status, and health/well-being. Specifically, nearly 83% of noncaregivers were non-Hispanic White as compared to only 41% of recent caregivers and 42% of long-term caregivers. Similarly, noncaregivers reported significantly higher rates of marriage, fewer chronic conditions, and higher income-to-needs ratios than both recent and long-term caregivers. As expected from these demographic dissimilarities, noncaregivers had higher rates of influenza vaccination, cholesterol screening, and Pap tests as compared to recent caregivers. However, we did not observe this large differential for noncaregivers versus long-term caregivers. For example, approximately 65% of long-term caregivers reported a Pap test in 2004 as compared to 64% of noncaregivers; among recent caregivers the proportion reporting a Pap test was well under 50%. So, despite the fact that long-term grandmother caregivers most closely resembled recent caregivers (demographically and socioeconomically), their reports of preventive behavior in 2004 were more similar to the reports of noncaregivers. One exception to this was in reports of breast self-exam. Nearly three fourths of long-term caregivers reported monthly breast self-exam as compared to 72% of recent caregivers and only 60% of noncaregivers.
Table 1.
Comparative Profile of Sample Characteristics for Grandmothers Raising Grandchildren vs Grandmothers not Raising Grandchildren
| Characteristic | Total (N = 5,298) | Raising Grandchild—Recent (n = 55) | Raising Grandchild—Long Term (n = 112) | Not Raising Grandchild (n = 5,131) |
|---|---|---|---|---|
| Age***, M (SD) | 62.8 (6.8) | 61.7 (6.6) | 59.2 (5.5) | 62.9 (6.8) |
| Black non-Hispanic***, % | 9.9 | 34.3 | 38.4 | 9.0 |
| Other non-Hispanic*, % | 2.0 | 9.9 | 3.3 | 1.9 |
| Hispanic**, % | 6.5 | 14.2 | 16.2 | 6.2 |
| Married***, % | 66.2 | 43.4 | 48.9 | 66.8 |
| Working full time, % | 25.0 | 20.5 | 25.6 | 25.0 |
| Working part time, % | 9.1 | 7.2 | 12.4 | 9.1 |
| Chronic conditions*, M (SD) | 1.8 (1.4) | 2.2 (1.4) | 2.0 (1.3) | 1.8 (1.4) |
| CES-D†, M (SD) | 1.6 (2.1) | 1.9 (2.0) | 2.0 (2.2) | 1.6 (2.1) |
| Income-to-needs ratio logged***, M (SD) | 1.5 (0.7) | 1.3 (0.6) | 1.1 (0.6) | 1.6 (0.7) |
| Insured, % | 89.0 | 81.1 | 85.5 | 89.1 |
| Increase in CES-D, % | 13.6 | 17.8 | 16.2 | 13.5 |
| Decrease in income-to-needs ratio**, % | 34.4 | 60.4 | 31.3 | 34.3 |
| Loss of insurance, % | 3.4 | 4.6 | 5.8 | 3.4 |
| Influenza vaccination (2004)* | 63.8 | 39.0 | 59.0 | 64.2 |
| Cholesterol screening (2004)** | 84.2 | 60.6 | 81.3 | 84.5 |
| Breast self-exam (2004)* | 60.4 | 71.5 | 74.3 | 60.0 |
| Mammogram (2004) | 66.8 | 76.4 | 77.4 | 77.3 |
| Pap test (2004) | 63.6 | 45.9 | 64.5 | 63.8 |
Notes: Chi-square (categorical variables); analysis of variance (continuous variables); centered weights used for analysis. CES-D = revised 8-item Center for Epidemiologic Studies-Depression scale.
p < .10
p < .05
p < .01
p < .001
Preventive Health Behaviors
Table 2 details the results of a series of longitudinal multivariate logistic regressions that assessed the effects of grandparent caregiving status on self-reported preventive health behaviors controlling for demographic characteristics, health and well-being, socioeconomic status, and prior preventive behavior. Grandparents who recently began raising a grandchild were less likely to report receiving an influenza vaccination (odds ratio = .42) and were less likely to report a cholesterol screening (odds ratio = .24) as compared to the reference group of noncaregiving grandparents. In addition, recent grandparent caregivers were less likely to receive a Pap test, although this finding was significant at the trend level only (p = .07). A very different picture emerged for grandmothers raising a grandchild for at least 2 years. The odds of influenza vaccination and monthly breast self-exam were more than 2 times higher for these grandmothers as compared to grandmothers not raising grandchildren. Cholesterol screening, mammography, and Pap tests did not differ significantly for grandmothers raising their grandchildren for at least 2 years.
Table 2.
Logistic Regression Results of Effect of Raising a Grandchild on Preventive Behavior
| Variable | Influenza Vaccination | Cholesterol Screening | Breast Self-Exam | Mammogram | Pap Test |
|---|---|---|---|---|---|
| Not raising grandchild (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Raising grandchild—recent | 0.42 (0.2, 0.9)* | 0.24 (0.1, 0.4)*** | 1.12 (0.5, 2.5) | 0.73 (0.3, 1.7) | 0.49 (0.2, 1.1)† |
| Raising grandchild—long term | 2.21 (1.1, 4.3)* | 0.99 (0.6, 1.7) | 2.11 (1.0, 4.3)* | 1.39 (0.7, 2.7) | 0.98 (0.6, 1.7) |
| Age | 1.04 (1.0, 1.1)*** | 1.02 (1.0, 1.0)* | 0.99 (1.0, 1.0) | 0.99 (1.0, 1.0) | 0.97 (0.9, 1.0)*** |
| White non-Hispanic (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black non-Hispanic | 0.54 (0.4, 0.7)*** | 0.90 (0.7, 1.2) | 1.74 (1.3, 2.3)*** | 1.12 (0.9, 1.4) | 1.18 (0.9, 1.5) |
| Other non-Hispanic | 1.38 (0.9, 2.1) | 2.48 (1.0, 5.5)* | 1.01 (0.5, 1.9) | 1.50 (0.7, 3.1) | 1.44 (0.6, 3.3) |
| Hispanic | 0.57 (0.4, 0.8)** | 0.67 (0.5, 0.9)** | 1.03 (0.8, 1.3) | 0.84 (0.6, 1.1) | 1.37 (0.9, 2.0) |
| Married | 1.15 (0.9, 1.4) | 1.16 (0.9, 1.4) | 1.27 (1.1, 1.5)** | 1.04 (0.8, 1.3) | 1.12 (0.9, 1.4) |
| Not working (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Working full time | 0.80 (0.6, 1.1) | 0.72 (0.6, 0.9)** | 1.10 (0.9, 1.3) | 0.82 (0.6, 1.1) | 0.98 (0.8, 1.2) |
| Working part time | 1.07 (0.8, 1.5) | 0.92 (0.6, 1.3) | 0.94 (0.7, 1.2) | 0.72 (0.5, 1.0)† | 0.78 (0.6, 1.0)† |
| Chronic conditions | 1.20 (1.1, 1.3)*** | 1.39 (1.3, 1.5)*** | 1.04 (1.0, 1.1) | 1.04 (1.0, 1.1) | 0.98 (0.9, 1.0) |
| CES-D | 0.96 (0.9, 1.0)† | 0.96 (.0.9, 1.0)† | 0.98 (0.9, 1.0) | 0.93 (0.9, 1.0)** | 0.95 (0.9, 1.0)** |
| Income-to-needs ratio logged | 1.26 (1.1, 1.5)** | 1.48 (1.3, 1.7)*** | 0.96 (0.9, 1.1) | 1.56 (1.4, 1.8)*** | 1.26 (1.1, 1.5)** |
| Insured | 1.13 (0.9, 1.4) | 1.49 (1.0, 2.2)* | 1.02 (0.8, 1.3) | 1.24 (0.9, 1.7) | 1.09 (0.8, 1.4) |
| Prior influenza vaccination | 14.07 (11.3, 17.5)*** | ||||
| Prior cholesterol screening | 4.75 (3.9, 5.8)*** | ||||
| Prior breast self-exam | 11.05 (9.8, 12.5)*** | ||||
| Prior mammogram | 8.24 (7.0, 9.7)*** | ||||
| Prior Pap test | 5.95 (5.2, 6.8)*** | ||||
| N | 5,294 | 5,257 | 5,292 | 5,287 | 5,278 |
| F (df) | 80.29*** (14, 39) | 36.96*** (14, 39) | 121.92*** (14, 39) | 54.48*** (14, 39) | 42.32*** (14, 39) |
Notes: Data are odds ratios (95% confidence intervals). We performed preliminary analyses to include other possible covariates, including education and multiple measures of physical and functional health. As these variables did not contribute to the explanatory power of the model, we excluded them from the final analysis. CES-D = revised 8-item Center for Epidemiologic Studies-Depression scale.
p < .10
p < .05
p < .01
p < .001
In order to determine whether emotional and financial strains on the household were responsible for the lower levels of preventive behavior among grandmothers who recently began raising a grandchild, we also tested the effects of possible mediating variables (changes in depression, poverty level, and insurance status; see Table 3). We included all covariates from Table 2 in this analysis, but, as estimates and p values of substantive variables did not change dramatically, we do not show their effects. Results showed that an increase in depressive symptoms was significantly associated with lower preventive health behavior for all three types of cancer screening, and loss of insurance suppressed all health behaviors except breast self-exam. However, these variables did not explain why preventive behaviors were less prevalent among grandmothers who recently began raising a grandchild.
Table 3.
Logistic Regression Results of Effect of Raising a Grandchild on Preventive Behavior: Mediating Effects of Changes in Depression, Poverty Level, and Insurance Status
| Variable | Influenza Vaccination | Cholesterol Screening | Breast Self-Exam | Mammogram | Pap Test |
|---|---|---|---|---|---|
| Not raising grandchild (ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Raising grandchild—recent | 0.41 (0.2, 0.9)* | 0.23 (0.1, 0.4)*** | 1.13 (0.5, 2.5) | 0.76 (0.3, 1.8) | 0.52 (.2, 1.1)† |
| Raising grandchild—long term | 2.20 (1.1, 4.3)* | 0.99 (0.6, 1.7) | 2.11 (1.00, 4.3)* | 1.40 (0.7, 2.7) | 1.00 (0.6, 1.8) |
| Increase in CES-D | 0.87 (0.7, 1.1) | 1.04 (0.8, 1.4) | 0.76 (0.6, 1.0)† | 0.70 (0.5, 0.9)** | 0.77 (0.6, 1.0)* |
| Decrease in income-to-needs ratio | 1.10 (0.9, 1.4) | 1.03 (0.8, 1.3) | 1.01 (0.9, 1.2) | 0.88 (0.7, 1.0) | 0.86 (0.7, 1.0) |
| Loss of insurance | 0.43 (0.2, 0.8)** | 0.60 (0.3, 1.0)† | 0.78 (0.5, 1.3) | 0.58 (0.4, 0.9)* | 0.61 (0.4, 1.0)* |
| N | 5,294 | 5,257 | 5,292 | 5,287 | 5,278 |
| F (df) | 80.16 (17, 36)*** | 33.13 (17, 36)*** | 120.68 (17, 36)*** | 41.88 (17,36)*** | 33.03 (17, 36)*** |
Notes: Data are odds ratios (95% confidence intervals). Covariates included in analysis, but not reported in table, include age, race/ethnicity, marital status, labor force participation, number of chronic conditions, CES-D score, income-to-needs ratio, insurance status, and prior preventive behavior. CES-D = revised 8-item Center for Epidemiologic Studies-Depression scale.
p < .10
p < .05
p < .01
p < .001
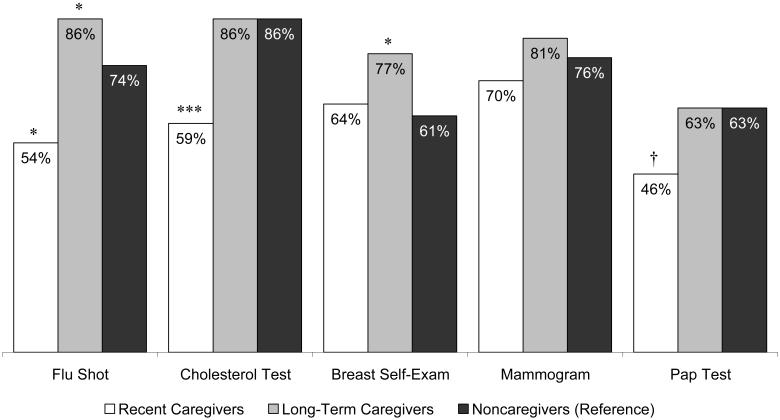
Figure 1 illustrates the predicted probabilities of each preventive behavior by grandmother caregiver status. We based calculations on logistic regression results from Table 3; characteristics reflect sample averages. Therefore, it is important to keep in mind that these differences in predicted probabilities reflect only the difference due directly to grandparent caregiver status; that is, we held constant demographic and socioeconomic differentials (in addition to all other controls) in the calculation of these probabilities. The predicted probability of receiving a flu shot among grandmothers who recently began raising a grandchild was approximately 54% as compared to more than 86% among long-term caregivers and nearly 74% among noncaregivers. The model predicted that less than 60% of recent caregivers would receive a cholesterol test as compared to around 86% of both long-term caregivers and noncaregivers. Turning to breast self-exam, long-term grandmother caregivers had the highest predicted probability of monthly breast self-exam at nearly 77%, whereas recent caregivers and noncaregivers had predicted probabilities of only 64% and 61%, respectively. Finally, among recent grandmother caregivers the predicted probability of receiving a Pap test was approximately 46%, whereas the probability for long-term caregivers and noncaregivers was equal at 63%. However, preventive behaviors that showed a decrease in usage among recent caregivers did not necessarily show a corresponding increase among long-term caregivers. Therefore, this research suggests that grandmother caregivers who have difficulty caring for themselves during the transition into care do not necessarily correct for this once they have adapted to care, but rather return only to prior levels of usage. Even in cases in which long-term caregivers showed a corresponding increase in usage (such as with influenza vaccinations), this increase was not proportional to the decrease seen during the transition into care.
Figure 1.
Predicted probabilities of preventive health behaviors for recent caregivers, long-term caregivers, and noncaregivers. †p < .10; *p < .05; ***p < .001.
An interesting pattern emerged in the calculation of the predicted probabilities. Regardless of statistical significance, grandmothers who recently began raising a grandchild had lower predicted probabilities as compared to noncaregivers for each preventive behavior assessed (with the exception of breast self-exam). In contrast, long-term grandmother caregivers had predicted probabilities that were equal to or higher than those of noncaregivers for each preventive behavior. So, the overall pattern for each of these preventive behaviors was consistent with our hypotheses. We point this out not to suggest that these nonsignificant findings should be interpreted, but rather to highlight the consistency and stability of the association of grandparent caregiving with preventive behavior.
DISCUSSION
This research examined whether raising a grandchild suppresses or elevates preventive health behavior based on the duration of time spent in that role. The results supported our hypothesis that contradictory pressures faced by caregiving grandmothers—time constraints and concern for the long-term well-being of the grandchild—differentially influence prevention, suppressing preventive behaviors among those transitioning into the caregiving role and enhancing preventive health behavior among long-term caregivers. Grandmothers who recently began raising a grandchild were less likely to report receipt of influenza vaccination, cholesterol screening, and Pap tests, but not breast self-exam or mammography. In view of our hypothesis that time constraints are the primary cause of the reduction in preventive health behavior, it is not surprising that grandmother caregivers did not report a reduction in breast self-exams, as this behavior requires minimal time and effort. In addition, it is worth noting that the pattern of mammography utilization, although not statistically significant, does reflect our hypothesized outcome. It is possible that, due to the high levels of media attention surrounding breast cancer awareness and prevention, grandmother caregivers are particularly motivated to make time for preventive behaviors linked to breast cancer, a motivation that is not present (or at least not as strong) for the other preventive behaviors measured in this study.
We found little evidence to support the hypothesis that emotional and financial strain mediates the suppression of health behaviors caused by the transition into care. Thus, even grandparents and grandchildren in households traditionally seen as stable (and therefore not generally targeted by state and federal programs) may be at adverse risk if lower use of health screening results in greater prevalence of disease and disability among caregiving grandparents.
Our results also show that grandmothers who had been raising a grandchild for at least 2 years were more likely to receive an influenza vaccination and to report monthly breast self-exams. This supports our hypothesis that long-term caregivers would be motivated to maintain a healthy lifestyle, thus compensating for the negative influence of time constraints. However, this seems to be the case only for preventive services that require minimal effort; those services that are most likely to require a doctor's visit are not affected. Only for influenza vaccination does increased use of preventive services among long-term grandmother caregivers partially offset the decreased use among grandmothers who recently began raising a grandchild; for cholesterol and Pap tests, grandmothers raising grandchildren do not appear to experience an increase in preventive service use following the transition into care.
The Centers for Disease Control and Prevention recommends that all persons older than age 50, particularly those with chronic conditions, receive annual influenza vaccinations (Fiore et al., 2007). Taking into consideration the fact that grandmothers who recently began raising a grandchild are particularly vulnerable to influenza-related complications and hospitalizations due to the higher levels of chronic conditions seen in this group, their lower receipt of influenza vaccination as compared to that of grandmothers not raising a grandchild is especially troubling. Compounding this situation is the fact that the majority of grandparent care households include at least one child of preschool age (Mutchler, Lee, & Baker, 2006), another age group at increased risk of influenza-related complications (Fiore et al., 2007). In fact, the Centers for Disease Control and Prevention recommends that everyone who either lives with or cares for a child younger than age 5 receive annual influenza vaccination (Fiore et al., 2007). So, grandmothers raising grandchildren who do not receive annual influenza vaccination not only are placing themselves at risk, but also are placing their grandchildren at risk both through the possibility of exposure to the influenza virus and through the possibility of being unable to provide care for the grandchild.
Low receipt of cholesterol screening and Pap tests among grandmothers who recently began raising a grandchild is equally troubling. Routine cholesterol screening is recommended for all women in this age group and is an important tool in identifying a person's risk of coronary heart disease (National Cholesterol Education Program, 2001; U.S. Preventive Services Task Force, 2006). Similarly, a Pap test is recommended for women in this age group at least every 2 to 3 years; the importance of the Pap test in early detection of cervical cancer has been well established (Etzioni et al., 2003; Smith, Cokkinides, & Eyre, 2007; Wingo et al., 2003). Missing even one recommended screening, either for cholesterol or cancer, might delay both diagnosis and treatment of a serious health problem. Even if the grandmother's preventive service use returns to normal levels after an adjustment period, the consequences of a delay in treatment may be severe.
Readers should also interpret our results within the context of several limitations of our study. First, our sample of grandmothers raising grandchildren, although nationally representative, was relatively small. Consequently, we accepted results that were marginally significant. Given the high cost of missed Pap tests, we feel that even trend-level significance is worthy of discussion and warrants further investigation, though this effect should be interpreted with caution. In addition, given the constraints of the data, we are not as yet able to follow one group of caregivers across time. Therefore, our conclusions about the timing of role adoption are necessarily comparative across sets of grandparents with different time exposures, when it would be more precise to examine fluctuations in health behaviors along the continuum of the caregiving career. It is quite possible that our results for long-term caregivers would differ if we had focused on one group of caregivers across multiple time points.
Our study is also limited by the fact that we could not identify a specific point in time at which the grandmother began raising a grandchild. Therefore, it is possible that some grandmothers who recently began raising a grandchild reported receiving preventive care before the grandchild entered the household. Although this measurement is necessary to capture the effects of the recency of care, it may limit the extent to which we can capture behavioral changes among grandmothers who recently began raising a grandchild. Furthermore, this study is not able to make a direct link between decreases in preventive behavior and concrete health outcomes; we can only make assumptions about the influence of altered preventive behavior on the health and well-being of grandmother caregivers.
Future Research
Future research should focus on the long-term consequences of poor health behavior during the transition into raising a grandchild for grandmothers, as well as for grandfathers. Does low receipt of preventive services during the transition into raising a grandchild lead directly to poor health outcomes among grandparents raising grandchildren? If so, are grandparents who experience poor health outcomes likely to transition out of the caregiving role as a result? As more waves of the HRS become available, it will be possible to track the health and caregiving trajectories of grandparent caregivers by following one group of caregivers past the transition into care and into the adaptation phase. Therefore, it will be possible to directly assess the sequential nature of our hypotheses. Furthermore, it will be important to determine if the influence of raising a grandchild on preventive behavior is unique or if other caregivers (such as spousal/parental caregivers or new parents) experience similar outcomes.
Policy Implications
Increased illness, hospitalization, and in severe cases mortality have direct costs for all older adults. However, within the population of grandparents raising grandchildren, the indirect costs may be as, if not more, severe. Grandparents often raise grandchildren in cases when there is no other viable alternative; many cite parental substance abuse or imprisonment as primary reasons they begin raising a grandchild (Jendrek, 1994; Johnson & Waldfogel, 2002). If a grandparent cannot provide care because of a serious health problem, the grandchild may be temporarily or permanently placed back in the care of a parent or may be placed in the foster care system. Even if grandparents raising grandchildren return home, they may be deemed an unsuitable placement for children if severe health problems persist.
Support groups targeted toward grandparents raising grandchildren could be an important tool in keeping grandparent caregivers informed on the importance of health maintenance. In fact, the positive health behavior observed among long-term caregivers may be due in part to participation in these support groups, either through direct health interventions or through a broader influence on adaptation to the caregiving role. During the transition into care, overwhelmed grandparent caregivers may lose sight of the fact that their health maintenance may directly influence the future of their grandchild, instead regarding proper self-care as selfish or expendable. Reinforcing the view that positive health behaviors can delay deterioration of the grandparent's health (and in turn diminish the possibility that the grandparent will become unable to provide care due to health concerns) may go far to help many grandparent caregivers realize the importance of their own health and well-being. In addition, support groups that have additional resources may want to organize health fairs or plan field trips to community health fairs. These health fairs often offer influenza vaccination and cholesterol screening at minimal or no cost to the recipient. As these preventive services seem to be the ones most negatively influenced by caring for a grandchild, increasing access through measures such as those described may help new grandparent caregivers avoid a lapse in proper health behavior.
ACKNOWLEDGMENTS
This research was supported by National Institute on Aging Grant T32-AG00037. Preliminary findings were presented at the 60th Annual Scientific Meeting of The Gerontological Society of America, San Francisco, CA, November 2007. We thank Laurie MacDougall for helpful comments on an earlier draft.
L.A. Baker designed the study, performed the data analysis, and was the primary manuscript author. M. Silverstein provided consultation and contributed to revising the manuscript.
REFERENCES
- Baker LA, Silverstein M. Depressive symptoms among grandparents raising grandchildren: The impact of participation in multiple roles. Journal of Intergenerational Relationships. doi: 10.1080/15350770802157802. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryson K, Casper LM. Co-resident grandparents and grandchildren. Census Bureau; Washington, DC: U.S.: 1999. (Publication No. P23-198). Available at www.census.gov/prod/99pubs/p23-198.pdf. [Google Scholar]
- Coltrane S. Research on household labor: Modeling and measuring the social embeddedness of routine family work. Journal of Marriage and Family. 2000;62:1208–1233. [Google Scholar]
- Etzioni R, Urban N, Ramsey S, McIntosh M, Schwartz S, Reid B, et al. The case for early detection. Nature Reviews Cancer. 2003;3:1–10. doi: 10.1038/nrc1041. [DOI] [PubMed] [Google Scholar]
- Ferree MM. Beyond separate spheres: Feminism and family research. Journal of Marriage and Family. 1990;52:866–884. [Google Scholar]
- Fiore AE, Shay DK, Haber P, Iskander JK, Uyeki TM, Mootrey G, et al. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP) 2007. Morbidity and Mortality Weekly Report. 2007;56:1–54. [PubMed] [Google Scholar]
- Freiman JA, Chalmers TC, Smith H, Kuebler RR. The importance of beta, the type II error and sample size in the design and interpretation of the randomized control trial. Survey of 71 “negative” trials. New England Journal of Medicine. 1978;299:690–694. doi: 10.1056/NEJM197809282991304. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, LaPierre TA, Luo Y. All in the family: The impact of caring for grandchildren on grandparents' health. Journal of Gerontology: Social Sciences. 2007;62B:S108–S119. doi: 10.1093/geronb/62.2.s108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jendrek MP. Grandparents who parent their grandchildren: Circumstances and decisions. The Gerontologist. 1994;34:206–216. doi: 10.1093/geront/34.2.206. [DOI] [PubMed] [Google Scholar]
- Johnson EI, Waldfogel J. Parental incarceration: Recent trends and implications for child welfare. Social Service Review. 2002;76:460–479. [Google Scholar]
- Lee S, Colditz G, Berkman L, Kawachi I. Caregiving to children and grandchildren and risk of coronary heart disease in women. American Journal of Public Health. 2003;93:1939–1944. doi: 10.2105/ajph.93.11.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Fuller-Thomson E. The health of grandparents raising grandchildren: Results of a national study. American Journal of Public Health. 1999;89:1384–1389. doi: 10.2105/ajph.89.9.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Roe KM. Grandmothers as caregivers: Raising children of the crack cocaine epidemic. Sage; Newbury Park, CA: 1993. [Google Scholar]
- Mutchler JE, Lee S, Baker LA. Grandparent care in the United States: Comparisons by race and ethnicity. 2006. Retrieved May 4, 2007, from the University of Massachusetts Boston Gerontology Institute Web site: www.geront.umb.edu/inst/pubAndStudies/DiversityinGrandparentCareHouseholds.pdf. [Google Scholar]
- National Cholesterol Education Program . Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III): Executive summary. National Institutes of Health; Washington, DC: 2001. (Publication No. 01-3670). [Google Scholar]
- Patterson JM. Families experiencing stress: The family adjustment and adaptation response model. Family Systems Medicine. 1988;5:202–237. [Google Scholar]
- Patterson JM. Integrating family resilience and family stress theory. Journal of Marriage and Family. 2002;64:349–360. [Google Scholar]
- Roe KM, Minkler M, Saunders F, Thomson GE. Health of grandmothers raising children of the crack cocaine epidemic. Medical Care. 1996;34:1072–1084. doi: 10.1097/00005650-199611000-00002. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Why people use health services. Milbank Memorial Fund Quarterly. 1966;44:94–124. [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Simmons T, Lawler Dye J. Grandparents living with grandchildren: 2000. 2003. (Publication No. C2KBR-31). Retrieved May 4, 2007, from U.S. Census Bureau Web site: www.census.gov/prod/2003pubs/c2kbr-31.pdf. [Google Scholar]
- Smith RA, Cokkinides V, Eyre HJ. Cancer screening in the United States, 2007: A review of current guidelines, practices, and prospects. CA: A Cancer Journal for Clinicians. 2007;57:90–104. doi: 10.3322/canjclin.57.2.90. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Shema SJ, Kaplan GA. New burdens or more of the same? Comparing grandparent, spouse, and adult-child caregivers. The Gerontologist. 1997;37:505–510. doi: 10.1093/geront/37.4.505. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatric Association. 1999;11:139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force . The guide to clinical preventive services. Agency for Healthcare Research and Quality; Washington, DC: 2006. (Publication No. 06-0588). [Google Scholar]
- Wingo PA, Cardinez CJ, Landis SH, Greenlee RT, Ries LAG, Anderson RN, et al. Long-term trends in cancer mortality in the United States, 1930-1998. Cancer. 2003;97:3133–3275. doi: 10.1002/cncr.11380. [DOI] [PubMed] [Google Scholar]