Abstract
Objectives. We investigated mental disorders, suicidal ideation, self-perceived need for treatment, and mental health service utilization attributable to exposure to peacekeeping and combat operations among Canadian military personnel.
Methods. With data from the Canadian Community Health Survey Cycle 1.2 Canadian Forces Supplement, a cross-sectional population-based survey of active Canadian military personnel (N = 8441), we estimated population attributable fractions (PAFs) of adverse mental health outcomes.
Results. Exposure to either combat or peacekeeping operations was associated with posttraumatic stress disorder (men: PAF = 46.6%; 95% confidence interval [CI] = 27.3, 62.7; women: PAF = 23.6%; 95% CI = 9.2, 40.1), 1 or more mental disorder assessed in the survey (men: PAF = 9.3%; 95% CI = 0.4, 18.1; women: PAF = 6.1%; 95% CI = 0.0, 13.4), and a perceived need for information (men: PAF = 12.3%; 95% CI = 4.1, 20.6; women: PAF = 7.9%; 95% CI = 1.3, 15.5).
Conclusions. A substantial proportion, but not the majority, of mental health–related outcomes were attributable to combat or peacekeeping deployment. Future studies should assess traumatic events and their association with physical injury during deployment, premilitary factors, and postdeployment psychosocial factors that may influence soldiers’ mental health.
The current military occupations in Iraq and Afghanistan have created a substantial resurgence of international interest in the mental health consequences of combat.1,2–7 Epidemiological studies of soldiers during postdeployment of combat and peacekeeping missions have demonstrated a high prevalence of mental disorders, mental health service use, and somatic complaints.2–4,8–17 However, it is important to note that several studies have not found an association between peacekeeping or combat operations and mental disorders5 or suicide.18,19
To the best of our knowledge, there is only 1 study that has examined the population attributable fractions (PAFs) associated with combat, and it was conducted in a nationally representative civilian sample.20 This study found that 28% of past-year posttraumatic stress disorder (PTSD) and approximately 10% of past-year major depression and substance use problems were attributable to lifetime combat exposure in men.20 Because none of the women in the study20 reported exposure to combat, the study was limited to men.
To date, there has been no empirical evaluation of PAFs for mental disorders in relation to combat in a representative sample of active military personnel. Also, no data are available on the PAFs for mental disorders associated with peacekeeping operations. There are many studies suggesting that soldiers involved in peacekeeping operations experience stressors different from those of soldiers involved in combat.21,22 Finally, there is no empirical evaluation of PAFs among female soldiers.
We studied data from a large population-based survey of active military personnel, the Canadian Community Health Survey Cycle 1.2 Canadian Forces Supplement.14 This survey is unique because it uses a multistage sampling design in active military personnel and includes the use of standardized state-of-the-art variable assessment of mental disorders,23 the self-perceived need for treatment,24,25 and mental health service use.23 Our main objective was to estimate the PAFs for mental disorders, suicidal ideation, and treatment need and use parameters (i.e., self-perceived need for treatment and mental health service utilization) associated with combat or peacekeeping operations.
METHODS
Survey
We used data from a cross-sectional population-based survey of Canadian Forces personnel collected between May and December 2002.14 The survey employed a multistage sampling framework to ensure representation of the sample in relation to the Canadian military (details of the sampling frame of survey are available upon request).14 The sample consisted of 5155 regular force members (response rate 79.5%) and 3286 reserve force members (response rate 83.5%). Reserve members were included in the target population if they had been active in the forces within the 6 months before data collection.
For the sake of anonymity, no information was available on the specific deployment location of the soldiers. However, based on the ages of the sample participants, it is likely that those included were involved in several different missions, including those in the Middle East (i.e., the first Gulf War), Rwanda, Somalia, and the former Yugoslavia.
Measures
Combat and peacekeeping operations.
All respondents were asked about their exposure to a comprehensive list of 28 traumatic events. This measure was abstracted from the PTSD section of the World Mental Health version of the Composite International Diagnostic Interview (CIDI) 28-item lifetime trauma exposure measure. Exposure to combat and peacekeeping operations was assessed with the following 2 questions: “Have you ever participated in combat, either as a member of a military or as a member of an organized nonmilitary group?” and “Have you ever served as a peacekeeper or relief worker in a war zone or in a place where there was ongoing terror of people because of political, ethnic, religious, or other conflicts?” The other 26 items included exposure to sexual trauma, interpersonal trauma, disasters, and accidents. However, systematic information was not available on whether these events occurred during deployment or during civilian life. Thus, a dichotomous variable was created for respondents who reported either combat or peacekeeping exposure.
To examine the unique effects of combat and peacekeeping, a 4-category variable was coded: (1) neither combat nor peacekeeping exposure, (2) combat exposure only, (3) peacekeeping exposure only, and (4) both combat and peacekeeping exposure. We also considered analyzing the data by examining the interaction between combat and peacekeeping operations; however, because of the challenges of estimating PAFs from interaction analyses, we chose the above approach, which is also consistent with recent work.20,26 It is important to note that soldiers who reported deployment to both combat and peacekeeping missions could have been deployed to 1 peacekeeping mission where they were exposed to combat while peacekeeping or to separate combat and peacekeeping missions at different times. No information was available in the data to differentiate these 2 alternatives.
Mental disorders.
The content of the survey was based partly on a selection of mental disorders from the World Mental Health Survey initiative.23,27 The World Health Organization CIDI version 2.1 was used to generate diagnoses according to the definitions and criteria of both the International Classification of Diseases, 10th Revision28 and the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV).29 The CIDI is a fully structured instrument for use by lay interviewers who do not have clinical experience and has been shown to have high levels of reliability and consistency with clinician-based diagnoses of DSM disorders assessed in this survey. The interviewers were trained according to World Mental Health survey standards.23 The methodology of the CCHS has been published elsewhere.30
Past-year prevalence of the following DSM-IV mental disorders was assessed: major depressive disorder, panic disorder, social phobia, generalized anxiety disorder, and PTSD. The diagnosis of PTSD was based on exposure to a list of 28 possible traumatic events (e.g., sexual assault, combat, life-threatening illness). Because the age of onset of social phobia is usually in childhood31 and there is no evidence to suggest that social phobia is precipitated postdeployment, we excluded social phobia from the analysis. (Details of the PTSD module as well as contents of the whole survey are available as an online supplement to the article at http://www.ajph.org) If respondents reported multiple traumatic events, they were asked to identify the event that was most upsetting to them. To assess criteria B and C of PTSD, further questions asked for the most upsetting event. The CIDI Short Form was used to assess alcohol-use disorders based on the criteria of the DSM-IV, in which 3 symptoms or more indicated alcohol dependence.32 DSM-IV alcohol abuse was not measured in the survey.
Suicidality.
Past-year suicidal ideation was measured using the following question: “Did you seriously think about committing suicide or taking your own life?”
Perceived need for mental health care.
The Perceived Need for Care Questionnaire, developed by Meadows et al.,14,25 was included in the Canadian Community Health Survey Cycle 1.2 Canadian Forces Supplement. Data on the reliability and validity of the questionnaire have been published.23 The questionnaire assessed whether a respondent perceived a need for care for problems with emotions, mental health, or use of alcohol or drugs in the past year and whether that need had been met. Five categories were covered: (1) information about mental health problems, its treatments, or available services; (2) medication; (3) therapy or counseling; (4) social interventions (help with financial or housing problems); and (5) skills training (help with employment status, work situation, or personal relationships).
Mental health service use.
All respondents were asked if they had seen or talked to a professional about their emotions, mental health, or use of alcohol or drugs in the past year. Professionals included a psychiatrist, family doctor, general practitioner or medical officer, other medical doctor, psychologist, nurse, nurse practitioner, physician's assistant or medic, social worker, counselor, or psychotherapist, religious or spiritual adviser, or other professional (e.g., acupuncturist, chiropractor, herbalist, or massage therapist). Past-year service use was indicated by reporting any of the aforementioned treatments.
Long-term restriction of activities.
Respondents were asked if a long-term physical health condition, mental health condition, or health problem had reduced the amount or kind of activity “at home,” “at school,” “at work,” or “in other activities, for example transportation or leisure.” For each of the areas of reduced functioning, the respondent had the choice of (1) often, (2) sometimes, or (3) never. Respondents who reported “never” for all areas of functioning were categorized as “not restricted,” and the remaining respondents were categorized as “restricted.”
Analyses
We used 2 estimation procedures. First, we employed the appropriate statistical weights provided by Statistics Canada to ensure that the data were representative of the Canadian Forces target population. All the percentages and regression analyses were based on the weighted sample, which takes into account nonresponse and provides estimates that are generalizable to the Canadian military population. Second, we used the bootstrapping method within the SUDAAN program33 to perform the necessary estimation of design-based standard errors required for data with a complex sampling design.30
We examined the prevalence of all independent and dependent measures stratified by gender. We used the χ2 test to determine the differences between men and women with respect to exposure to the deployment variables and outcome variables. PAFs of outcomes represent the percentage of all cases of each outcome among military personnel exposed to combat or peacekeeping that would not have occurred if exposure had not occurred. Although there are multiple methods for calculating PAFs, we chose the following method, which is based on consultations with various biostatistics and population health researchers.34,35 The formula used in the analysis was
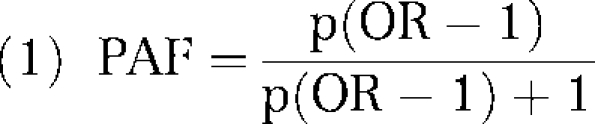 |
where p is the proportion exposed in the entire cohort and OR is equal to the odds ratio of outcomes given combat or peacekeeping exposure. We calculated ORs based on multiple logistic regression analyses in which the presence or absence of either combat or peacekeeping was the independent variable and the mental health, disability, and service use outcomes were the dependent variables. We conducted a separate logistic regression model for each dependent variable. To adjust for confounding variables,34 we adjusted all models for sociodemographic variables that included age, marital status, education, income, military rank (junior, senior, or officer), and type of force (regular vs reserve). We conducted similar regressions with the 4-category deployment variable to examine the individual and combined effects of combat and peacekeeping.
RESULTS
Per standard reporting of population-based surveys, all tables show unweighted n based on the sample and percentages that are weighted for nonresponse and allow for generalizability to the Canadian military population. Table 1 summarizes the sociodemographic characteristics of the sample. The majority of the sample was aged between 25 and 44 years, married, and regular personnel. Table 2 reports the lifetime prevalence of exposure to deployment-related variables. Men were significantly more likely to report exposure to combat or peacekeeping operations than were women. Table 3 shows the past-year prevalence of mental disorders, perceived need, and service use outcome variables. The prevalence of any mental disorder assessed in the survey in men and women was 13.1% and 15.1%, respectively. With the exception of alcohol dependence and generalized anxiety disorder, women had a significantly higher prevalence of mental disorders, mental health service use, and perceived need for treatment than did men.
TABLE 1.
Sample Demographic Characteristics: Canadian Military Personnel, May to December 2002
| Men (n = 5849), No. (%) | Women (n = 2592), No. (%) | |
| Age, y | ||
| 16–24 | 831 (18.6) | 498 (23.0) |
| 25–34 | 1549 (30.1) | 909 (34.1) |
| 35–44 | 2324 (38.0) | 923 (34.7) |
| 45–54 | 1145 (13.3) | 262 (8.2) |
| Marital status | ||
| Married | 3979 (64.6) | 1446 (53.8) |
| Separated/widowed/divorced | 404 (6.9) | 253 (10.4) |
| Never married | 1464 (28.6) | 892 (35.8) |
| Household income, Can $ | ||
| > 80 000 | 2574 (38.1) | 1276 (45.9) |
| 50 000–79 999 | 2167 (39.9) | 651 (25.9) |
| 30 000–49 999 | 747 (16.4) | 430 (19.9) |
| < 29 999 | 263 (5.6) | 178 (8.2) |
| Education | ||
| Undergraduate degree or higher | 1392 (16.9) | 916 (23.3) |
| Any postsecondary school below undergraduate degree | 1716 (29.8) | 730 (32.2) |
| High school diploma or less | 2737 (53.3) | 943 (44.5) |
| Type of service | ||
| Regular | 3664 (73.0) | 1490 (58.9) |
| Reserve | 2185 (27.0) | 1102 (41.1) |
| Rank grouping | ||
| Junior | 2251 (58.7) | 1295 (66.0) |
| Senior | 1852 (21.2) | 293 (14.1) |
| Officer | 1746 (20.2) | 1004 (19.8) |
Note. Sample numbers are unweighted. Percentages are weighted.
TABLE 2.
Lifetime Exposure to Deployment-Related Traumatic Events Among Active Canadian Military Personnel: May to December 2002
| Men (n = 5849), No. (%) | Women (n = 2592), No. (%) | χ2 Difference (df) | |
| No combat or peacekeeping exposure | 3441 (57.4) | 2146 (81.8) | 551.62** (3) |
| Peacekeeping exposure only | 1432 (25.1) | 297 (11.6) | |
| Combat exposure only | 206 (3.3) | 44 (2.0) | |
| Both combat and peacekeeping exposure | 762 (14.2) | 105 (4.6) | |
| Combat or peacekeeping exposure | 2400 (42.6) | 446 (18.2) | 542.50** (1) |
Note. df = degrees of freedom. Sample numbers are unweighted. Percentages are weighted.
**P < .001.
TABLE 3.
Prevalence of Mental Disorders and Perceived Need for Care Among Active Canadian Military Personnel: May to December 2002
| Past 12-Month Variables | Men (n = 5849), No. (%) | Women (n = 2592), No. (%) | χ2 Difference (df) |
| Any mental disorder | 719 (13.1) | 409 (15.1) | 4.49 (1)* |
| Major depression | 326 (6.4) | 237 (9.8) | 20.16 (1)** |
| Panic disorder | 81 (1.6) | 56 (2.6) | 5.74 (1)* |
| Generalized anxiety disorder | 86 (1.6) | 58 (2.1) | NS |
| Posttraumatic stress disorder | 107 (2.2) | 72 (3.3) | 6.11 (1)* |
| Alcohol dependence | 250 (5.2) | 52 (2.3) | 38.32 (1)** |
| Suicidal ideation | 193 (3.7) | 115 (4.8) | 4.14 (1)* |
| Long-term restriction of activity | 1569 (27.5) | 668 (26.1) | NS |
| Any perceived need for treatment | 1216 (22.1) | 748 (29.8) | 42.28 (1)** |
| Information | 595 (11.1) | 313 (13.0) | 4.16 (1)* |
| Medication | 272 (5.3) | 244 (10.4) | 45.27 (1)** |
| Counseling | 615 (11.4) | 490 (19.2) | 64.31 (1)** |
| Social intervention | 202 (4.0) | 103 (4.5) | NS |
| Skills training | 646 (11.8) | 413 (16.0) | 19.93 (1)** |
| Any mental health service use | 628 (11.5) | 516 (20.3) | 79.11 (1)** |
Note. df = degrees of freedom; NS = nonsignificant. Sample numbers are unweighted. Percentages are weighted.
*P < .05; **P < .001.
Tables 4 and 5 illustrate the adjusted odds ratios (ORs) and PAFs for outcomes associated with combat and peacekeeping in men and women, respectively. The majority of mental illness, perceived need, and service use were caused by the combat or peacekeeping operations. Among the mental disorders, PTSD had the greatest PAFs for both men and women. In comparison with those soldiers exposed to combat only or peacekeeping only, those reporting exposure to both peacekeeping and combat had stronger associations with several outcomes. It should be noted that the PAFs for combat alone, peacekeeping alone, and both combat and peacekeeping are not additive; therefore, the sum of these PAFs will not equal the combat or peacekeeping PAF.
TABLE 4.
Population Attributable Fraction Percentages (PAFs) of Mental Health Problems and Mental Health Service Use in Relation to Combat and Peacekeeping Exposure Among Male Active Canadian Military Personnel: May to December 2002
| Peacekeeping Alone |
Combat Alone |
Both Combat and Peacekeeping |
Combat or Peacekeeping |
|||||
| Past 12-Month Variables | AORa (95% CI) | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) |
| Any mental disorderb | 1.05 (0.82, 1.35) | NS | 1.46 (0.94, 2.26) | NS | 1.53** (1.17, 2.01) | 7.0 (2.4, 12.6) | 1.24* (1.01, 1.52) | 9.3 (0.4, 18.1) |
| Major depression | 1.04 (0.75, 1.44) | NS | 0.92 (0.42, 2.04) | NS | 1.64** (1.15, 2.34) | 8.3 (2.1, 16.0) | 1.23 (0.93, 1.62) | NS |
| Panic disorder | 0.94 (0.50, 1.77) | NS | 2.28 (0.77, 6.79) | NS | 1.38 (0.70, 2.74) | NS | 1.19 (0.68, 2.05) | NS |
| Generalized anxiety disorder | 0.64 (0.36, 1.16) | NS | … | … | 0.85 (0.40, 1.81) | NS | 0.68 (0.41, 1.14) | NS |
| Posttraumatic stress disorder | 1.99* (1.13, 3.53) | 19.9 (3.16, 8) | 3.82* (1.25, 11.65) | 8.5* (0.8, 26.6) | 4.77** (2.74, 8.30) | 34.9 (19.8, 50.9) | 3.05** (1.88, 4.95) | 46.6 (27.3, 62.7) |
| Alcohol dependence | 1.00 (0.64, 1.56) | NS | 1.71 (0.85, 3.46) | NS | 0.88 (0.50, 1.52) | NS | 1.05 (0.73, 1.52) | NS |
| Suicidal ideation | 1.02 (0.69, 1.52) | NS | 0.92 (0.33, 2.53) | NS | 1.39 (0.88, 2.20) | NS | 1.13 (0.81, 1.59) | NS |
| Long-term restriction of activity | 1.17 (0.99, 1.38) | NS | 1.45* (1.03, 2.03) | 1.5 (0.1, 15.3) | 1.60** (1.30, 1.96) | 7.9 (4.1, 12.0) | 1.32** (1.14, 1.53) | 12.0 (5.6, 18.4) |
| Any perceived need for treatmentc | 0.94 (0.78, 1.13) | NS | 1.34 (0.92, 1.94) | NS | 1.34** (1.09, 1.66) | 4.6 (1.3, 8.6) | 1.10 (0.95, 1.28) | NS |
| Information | 1.09 (0.87, 1.38) | NS | 1.81** (1.15, 2.85) | 2.6 (0.5, 5.8) | 1.65** (1.27, 2.15) | 8.5 (3.7, 14.0) | 1.33** (1.10, 1.61) | 12.3 (4.1, 20.6) |
| Medication | 0.82 (0.57, 1.16) | NS | 1.13 (0.48, 2.65) | NS | 1.77** (1.24, 2.52) | 9.9 (3.3, 17.8) | 1.15 (0.86, 1.53) | NS |
| Counseling | 0.92 (0.73, 1.16) | NS | 1.59 (0.99, 2.56) | NS | 1.24 (0.94, 1.63) | NS | 1.07 (0.88, 1.32) | NS |
| Social intervention | 0.69 (0.44, 1.06) | NS | 1.45 (0.63, 3.35) | NS | 0.79 (0.49, 1.30) | NS | 0.79 (0.55, 1.12) | NS |
| Skills training | 0.99 (0.79, 1.25) | NS | 1.13 (0.67, 1.90) | NS | 1.43** (1.10, 1.85) | 5.8 (1.4, 10.8) | 1.14 (0.94, 1.38) | NS |
| Any mental health service use | 1.01 (0.81, 1.27) | NS | 1.13 (0.66, 1.92) | NS | 1.35* (1.03, 1.78) | 4.7 (0.4, 10.0) | 1.13 (0.93, 1.38) | NS |
Note. AOR = adjusted odds ratio; CI = confidence interval; NS = not significant. Sample numbers are unweighted. Percentages are weighted. Ellipses indicate that the sample size was too small to calculate.
Adjusted for age, marital status, income, education, military rank (junior, senior, or officer), and type of force (regular vs reserve).
Reference group for these regressions is “No past-year mental disorder.”
Reference group for these regressions is “No past-year perceived need for treatment.”
*P < .05; **P < .01.
TABLE 5.
Population Attributable Fraction Percentages (PAFs) of Mental Health Problems and Mental Health Service Use in Relation to Combat and Peacekeeping Exposure Among Female Active Canadian Military Personnel: May to December 2002
| Peacekeeping Alone |
Combat Alone |
Both Combat and Peacekeeping |
Combat or Peacekeeping |
|||||
| Past 12-Month Variables | AORa (95% CI)c | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) | AORa (95% CI) | PAF (95% CI) |
| Any mental disorderb | 0.87 (0.58, 1.32) | NS | 2.57* (1.28, 5.18) | 3.0* (0.6, 7.7) | 2.23** (1.33, 3.71) | 5.4* (1.5, 11.2) | 1.36* (1.00, 1.85) | 6.1* (0.0, 13.4) |
| Major depression | 0.80 (0.49, 1.31) | NS | 2.74* (1.22, 6.18) | 3.4* (0.4, 9.4) | 2.32** (1.30, 4.16) | 5.8* (1.4, 12.8) | 1.33 (0.92, 1.94) | NS |
| Panic disorder | 2.51* (1.22, 5.16) | 14.9* (2.5, 32.6) | … | … | 3.59* (1.07, 12.03) | 10.7* (0.3, 33.9) | 3.03** (1.60, 5.72) | 27.0* (9.8, 46.2) |
| Generalized anxiety disorder | … | … | … | … | 3.05* (1.21, 7.71) | 8.7* (1.0, 23.8) | 1.08 (0.57, 2.05) | NS |
| Posttraumatic stress disorder | 1.78 (0.84, 3.78) | NS | 6.99** (2.33, 20.98) | 10.7* (2.6, 28.5) | 3.99** (1.69, 9.43) | 12.2* (3.1, 28.1) | 2.70** (1.56, 4.68) | 23.6* (9.2, 40.1) |
| Alcohol dependence | … | … | … | … | … | … | 1.74 (0.77, 3.97) | NS |
| Suicidal ideation | 0.82 (0.41, 1.65) | NS | 2.46 (0.84, 7.24) | NS | 2.08 (0.93, 4.65) | NS | 1.30 (0.80, 2.13) | NS |
| Long-term restriction of activity | 1.06 (0.80, 1.40) | NS | 1.48 (0.78, 2.81) | NS | 1.32 (0.84, 2.05) | NS | 1.16 (0.91, 1.48) | NS |
| Any perceived need for treatmentc | 0.84 (0.63, 1.11) | NS | 1.28 (0.65, 2.52) | NS | 1.72* (1.12, 2.65) | 3.2* (0.6, 7.1) | 1.07 (0.85, 1.34) | NS |
| Information | 0.99 (0.67, 1.56) | NS | 2.53* (1.17, 5.45) | 3.0* (0.3, 8.2) | 2.51** (1.48, 4.26) | 6.6* (2.2, 13.2) | 1.47* (1.07, 2.01) | 7.9* (1.3, 15.5) |
| Medication | 0.78 (0.51, 1.20) | NS | 1.20 (0.38, 3.82) | NS | 1.50 (0.78, 2.90) | NS | 0.96 (0.67, 1.37) | NS |
| Counseling | 0.87 (0.63, 1.21) | NS | 1.33 (0.70, 2.52) | NS | 1.95** (1.23, 3.10) | 4.2* (1.1, 8.9) | 1.14 (0.88, 1.48) | NS |
| Social intervention | 0.60 (0.25, 1.47) | NS | … | … | 2.42* (1.05, 5.55) | 6.2* (0.2, 17.5) | 1.02 (0.58, 1.79) | NS |
| Skills training | 0.84 (0.59, 1.20) | NS | 1.13 (0.53, 2.40) | NS | 1.55 (0.97, 2.47) | NS | 1.02 (0.77, 1.34) | NS |
| Any mental health service use | 0.86 (0.63, 1.18) | NS | 1.06 (0.53, 2.09) | NS | 1.78* (1.10, 2.89) | 3.5* (0.5, 8.1) | 1.08 (0.83, 1.41) | NS |
Note. AOR = adjusted odds ratio; CI = confidence interval; NS = not significant. Sample numbers are unweighted. Percentages are weighted. Ellipses indicate that the sample size was to small to calculate.
Adjusted for age, marital status, income, education, military rank (junior, senior, or officer), and type of force (regular vs reserve).
Reference group for these regressions is “No past-year mental disorder.”
Reference group for these regressions is “No past-year perceived need for treatment.”
*P < .05; **P < .01.
There were some gender differences in the findings. Although long-term restriction of activities was not significantly associated with combat or peacekeeping in women, this association was significant in men (PAF = 12.0%). On the other hand, women had a significant association of panic disorder with combat or peacekeeping (PAF = 27.0%), whereas men did not.
DISCUSSION
To the best of our knowledge, our study is the first to provide PAFs for the association between several mental health outcomes (mental disorders and suicidal ideation, help seeking, and perceived need) and combat and peacekeeping in a representative sample of active military personnel. This investigation adds to a growing body of knowledge showing that soldiers returning from deployment are increasingly likely to have emotional problems,3 to have somatic complaints,6,10 and to use mental health services.4 Like previous findings from a US civilian sample,20 our findings illustrate that the highest PAFs associated with combat or peacekeeping were for PTSD.
Our findings are also consistent with previous work that suggests a minority of mental health problems—even in a sample of active military personnel—is attributable to combat.20 Thus, most mental illness is likely attributable to a wide range of putative risk factors (e.g., genetic, childhood adversity, stressful life events, social supports, and personality) that have been shown in civilian samples and are also likely to be important in military samples.
Our findings suggest that exposure to the combination of combat and peacekeeping operations may have a broader effect on several outcomes than do exposure to peacekeeping only or combat only. These findings are consistent with previous studies. Important nonsignificant findings include the lack of association between peacekeeping or combat and mental health outcomes such as alcohol dependence and suicidal ideation. As noted, the association of mental health problems with suicide in relation to peacekeeping has yielded inconsistent results. Thus, the present findings were consistent with some, but not all, previous work in this area.36,37
Limitations
The following limitations of the study should be considered. First, because of the cross-sectional nature of the survey, we cannot make causal inferences. The age of onset of combat and peacekeeping was not available in the survey; thus, we could not examine when the onset of emotional problems occurred in relation to exposure to combat and peacekeeping. However, like Prigerson et al.,20 we used a lifetime exposure to combat and peacekeeping variable with past-12-month outcomes. Given that most military recruits are young and the natural history of the mental disorders under consideration in this study, it is highly likely that most of the studied disorders have their onset after entry into the military, but it is impossible to ascertain this precisely from the data.
Second, although reliable diagnoses23,38 and need for treatment were based on trained lay interviewer assessment, they may not match the accuracy of clinician-based assessment. However, a recent study found moderate to good concordance between CIDI and structured clinical interview–based diagnoses for most mental disorders.39 Third, detailed information on exposure to traumatic events during deployments was not available. Because there is emerging evidence to suggest that there is a dose–response group relationship between exposure to traumatic events and PTSD,8 future studies should examine PAFs in relation to level of trauma exposure during deployment.
Fourth, alcohol abuse, a prevalent problem among male soldiers, was not assessed in the survey. Thus, we were unable to examine PAFs for alcohol abuse. Finally, it should be noted that the PAFs likely underestimate the associations between combat or peacekeeping operations and outcomes. This is because individuals with the greatest severity of physical or emotional illness following deployment were likely no longer active in the military at the time of the survey.
Conclusions
A substantial proportion, but not the majority, of outcomes were attributable to combat or peacekeeping. With the recent deployment of Canadian soldiers to Afghanistan, where there is substantial exposure to combat, it is possible that a greater number of soldiers are affected with mental health problems than seen in this study. Future studies should consider including a detailed assessment of traumatic events and their association with physical injury40 during deployment, examination of premilitary factors such as childhood adversity,41 and postdeployment psychosocial factors that may influence the mental health of soldiers.
Acknowledgments
Preparation of this article was supported by a New Emerging Team grant (PTS 63186) from the Canadian Institutes of Health Research (CIHR) Institute of Neurosciences, Mental Health, and Addiction; a CIHR operating grant (135861); a CIHR New Investigator grant (152348); a Career Development (K24) award from the National Institutes of Health (MH64122); a CIHR Investigator award; a Canada research chair; a CIHR Canada graduate scholarship–master's award; a Western Regional Training Centre studentship funded by the Canadian Health Services Research Foundation, Alberta Heritage Foundation for Medical Research, and Canadian Institutes of Health Research; and a Social Sciences and Humanities Research Council of Canada Graduate Scholarship-Doctorate award.
The authors thank Natalie Mota, Daniel Rasic, and the anonymous reviewer for their thoughtful comments on the article.
Human Participant Protection
Human participants were involved; however, there was no direct human contact in this research study because this study employed secondary data only. Therefore, all appropriate ethical approvals and informed consent were obtained by the original study coordinators, Statistics Canada. There is also a rigorous approval process through this governmental agency that is implemented before access to the data is approved, which maintains the ethical standards for release of data and confidentiality. The sample has been used extensively in this fashion in other studies.
References
- 1. National Defence. Current Operations. National Defence and the Canadian Forces 2007. Available at: http://www.dnd.ca/site/Operations/current_ops_e.asp. Accessed September 12, 2007.
- 2.Seal KH, Bertenthal D, Miner CR, et al. Bringing the war back home: mental health disorders among 103 788 US veterans returning from Iraq and Afghanistan seen at the Department of Veterans Affairs facilities. Arch Intern Med 2007;167:476–482 [DOI] [PubMed] [Google Scholar]
- 3.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13–22 [DOI] [PubMed] [Google Scholar]
- 4.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295:1023–1032 [DOI] [PubMed] [Google Scholar]
- 5.Horn O, Hull L, Jones M, et al. Is there an Iraq war syndrome? Comparison of the health of UK service personnel after the Gulf and Iraq wars. Lancet 2006;367:1742–1746 [DOI] [PubMed] [Google Scholar]
- 6.Hotopf M, Hull L, Fear NT, et al. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet 2006;367:1731–1741 [DOI] [PubMed] [Google Scholar]
- 7.Stein DJ, Seedat S, Iversen A, et al. Post-traumatic stress disorder: medicine and politics. Lancet 2007;369:139–144 [DOI] [PubMed] [Google Scholar]
- 8.Dohrenwend BP, Turner JB, Turse NA, et al. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science 2006;313:979–982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNally RJ. Psychiatric casualties of war. Science 2006;313:979–982 [DOI] [PubMed] [Google Scholar]
- 10.Hoge CW, Terhakopian A, Castro CA, et al. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry 2007;164:150–153 [DOI] [PubMed] [Google Scholar]
- 11.Buckley TC. PTSD and Vietnam veterans. Science 2007;315:184–187 [PubMed] [Google Scholar]
- 12.Vermetten E, Bremner JD, Skelton L, et al. PTSD and Vietnam veterans. Science 2007;315:184–187 [DOI] [PubMed] [Google Scholar]
- 13.Frueh BC. PTSD and Vietnam veterans. Science 2007;315:184–187 [PubMed] [Google Scholar]
- 14.Sareen J, Cox BJ, Afifi TO, et al. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry 2007;64:843–852 [DOI] [PubMed] [Google Scholar]
- 15.Gray MJ, Bolton EE, Litz BT. A longitudinal analysis of PTSD symptom course: delayed-onset PTSD in Somalia peacekeepers. J Consult Clin Psychol 2004;72:909–913 [DOI] [PubMed] [Google Scholar]
- 16.Litz BT, Orsillo SM, Friedman M, et al. Posttraumatic stress disorder associated with peacekeeping duty in Somalia for US military personnel. Am J Psychiatry 1997;154:178–184 [DOI] [PubMed] [Google Scholar]
- 17.Smith TC, Ryan MA, Wingard DL, et al. and the Millennium Cohort Study Team New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ 2008;336:366–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang HK, Bullman TA. Mortality among US veterans of the Persian Gulf War. N Engl J Med 1996;14:1498–1504 [DOI] [PubMed] [Google Scholar]
- 19.Belik SL, Cox BJ, Stein MB, et al. Traumatic events and suicidal behavior: results from a national mental health survey. J Nerv Ment Dis 2007;195:342–349 [DOI] [PubMed] [Google Scholar]
- 20.Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposure among US men. Am J Public Health 2002;92:59–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bartone PT, Adler AB, Vaitkus MA. Dimensions of psychological stress in peacekeeping operations. Mil Med 1998;163:587–593 [PubMed] [Google Scholar]
- 22.Shigemura J, Nomura S. Mental health issues of peacekeeping workers. Psychiatry Clin Neurosci 2002;56:483–491 [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13:93–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meadows G, Harvey C, Fossey E, et al. Assessing perceived need for mental health care in a community survey: development of the Perceived Need for Care Questionnaire (PNCQ). Soc Psychiatry Psychiatr Epidemiol 2000;35:427–435 [DOI] [PubMed] [Google Scholar]
- 25.Meadows G, Burgess P, Fossey E, et al. Perceived need for mental health care, findings from the Australian National Survey of Mental Health and Well-Being. Psychol Med 2000;(3):645–656 [DOI] [PubMed] [Google Scholar]
- 26.Afifi TO, Cox BJ, Enns MW, et al. Population attributable fractions of psychiatric disorders and suicide ideation and attempts associated with adverse childhood experiences. Am J Public Health 2008;98:946–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593–602 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization International Classification of Diseases, 10th Revision Geneva, Switzerland: World Health Organization; 1992 [Google Scholar]
- 29.American Psychiatric Association Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, Text Revision Washington, DC: American Psychiatric Association; 2000 [Google Scholar]
- 30.Gravel R, Beland Y. The Canadian Community Health Survey: mental health and well-being. Can J Psychiatry 2005;50:573–579 [DOI] [PubMed] [Google Scholar]
- 31.Ruscio AM, Brown TA, Chiu WT, et al. Social fears and social phobia in the United States: results from the National Comorbidity Survey Replication. Psychol Med 38(1):15–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler RC, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Int J Methods Psychiatr Res 1998;7:171–185 [Google Scholar]
- 33.Shah BV, Barnswell BG, Bieler GS. SUDAAN User's Manual: Software for Analysis of Correlated Data. Release 6.40 Research Triangle Park, NC: Research Triangle Institute; 1995 [Google Scholar]
- 34.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health 1998;88:15–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Young TK. Population Health: Concepts and Methods 2nd ed.New York, NY: Oxford University Press; 2005 [Google Scholar]
- 36.Browne T, Hull L, Horn O, et al. Explanations for the increase in mental health problems in UK reserve forces who have served in Iraq. Br J Psychiatry 2007;190:484–489 [DOI] [PubMed] [Google Scholar]
- 37.Wong A, Escobar M, Lesage A, et al. Are UN peacekeepers at risk for suicide. Suicide Life Threat Behav 2001;31:103–112 [DOI] [PubMed] [Google Scholar]
- 38.Kessler RC, Abelson J, Demler O, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI). Int J Methods Psychiatr Res. 2004;13:122–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res 2006;15:167–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoge CW, McGurk D, Thomas JL, et al. Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med 2008;358:453–463 [DOI] [PubMed] [Google Scholar]
- 41.Cabrera OA, Hoge CW, Bliese PD, et al. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. Am J Prev Med 2007;33:77–82 [DOI] [PubMed] [Google Scholar]


