Abstract
Purpose
The purpose of this article is to present a Swedish study exploring health care professionals’ cooperation in the chain of care for expectant and new parents between antenatal care (AC), postpartum care (PC) and child health care (CHC). Furthermore, the rationale was to conceptualise barriers and facilitators of cooperation in order to generate a comprehensive theoretical model which may explain variations in the care providers’ experiences.
Methods
Thirty-two midwives and CHC nurses were interviewed in five focus group – and two individual interviews in a suburb of a large Swedish city. Grounded Theory was applied as the research methodology.
Results
One core category was discerned: linkage in the chain of care, including six categories with subcategories. Despite the fact that midwives as well as CHC nurses have common visions about linkage, cooperation is not achieved because of interacting barriers that have different influences on the three links in the chain.
Conclusions
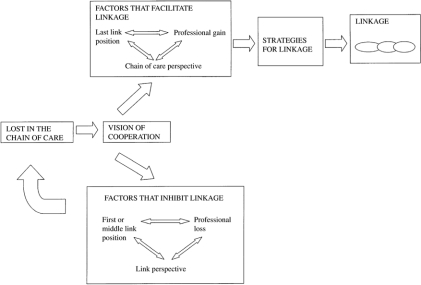
Barriers to linkage are lack of professional gain, link perspective and first or middle position in the chain, while facilitators are chain perspective, professional gain and last position in the chain. As the last link, CHC nurses promote a linkage most strongly and have the greatest gain from such linking.
Keywords: focus group, grounded theory, chain of care, professional cooperation, expectant/new parents
Introduction
Early discharge from hospital wards for mothers with newborn babies has become typical in many Western countries, which means that cooperation between maternity and child health care professionals is essential to ensure safe quality care; however, cooperation between key professional groups is suboptimal [1]. The purpose of this article is to present a Swedish study exploring health care professionals’ cooperation in the chain of care for expectant and new parents between antenatal care (AC), postpartum care (PC) and child health care (CHC). Concepts like chain of care, coordination, cooperation and collaboration have several different meanings in the literature [2]. The two concepts most relevant to this study are ‘chain of care’ and ‘cooperation’. Chain of care is defined as linked coordinated activities including all health care providers serving a specific patient group within a county with the aim of providing good quality care for patients [3]. A common definition of cooperation is “joint interaction with different types of resources for a common pursuit” [2]. Our particular interest is in cooperation between individual professionals or groups of professionals in different facilities but in the same chain of care, specifically (AC-PC-CHC). A general picture of what the organisation of the chain of care is like in Sweden is shown in Table 1. It is notable that nurses with a specialist degree (midwives or paediatric nurses or district nurses) have far reaching responsibilities and are in charge of most of the care in the chain of care.
Table 1.
Organization of the chain of care of antenatal care, labour and delivery, postpartum care and child health care in Sweden
| Type of care | Antenatal care | Labour and delivery | Post partum care | Child health Care |
|---|---|---|---|---|
| Type of clinic | Antenatal clinics | Hospital ward | Hospital ward | Child health service |
| Duration of responsibility | Pregnancy | Birth | One week after delivery | Infant 0–6 years |
| Professionals | Midwives | Midwives | Midwives | Paediatric nurse/district nurse |
| Management | Primary health care | County council | County council | Primary health care |
The average postpartum length of stay in a hospital has declined steadily in many Western countries. In Sweden, Stockholm County, the length of stay is now one to two days [4]. Studies suggest that early discharge is a safe and secure protocol provided there is some form of post-discharge nursing or midwifery support and an effective chain of care [5–7]. However, a lack of structure and other gaps in the chain of care have been reported and early discharge is not always followed by support during the immediate post-discharge period [8–10]. Most Western countries have less well developed systems for home-based postnatal care [5] in contrast to the Netherlands, the only industrialised country with a large proportion of postnatal home-based care [11].
We have only been able to find a few scientific studies on professional or parental perceptions of postpartum support. A couple of these studies show parental discontent with the postpartum care because of too short stays in the hospital and insufficient support, particularly concerning breastfeeding [12–15]. This is particularly remarkable as breastfeeding is also the prime reason for women to contact health care units and hospitals in the post-discharge period [9, 16]. Furthermore, during a ten-year period the number of infants breastfeeding fully after one week has decreased in Stockholm county [17], which could be the result of a lack of support, although other reasons are possible.
Psychosocial issues connected with supporting expectant/new parents have been emphasised during the last few decades in Sweden [18], although professional responsibilities and task duties concerning these issues are neither clearly defined nor well framed [19]. The importance of obtaining a psychosocial history in early pregnancy to identify women at risk for postpartum depression has also been emphasised [20–21], as a depression is a severe risk condition for the mother as well as for the child and it may severely affect breastfeeding and the experience of motherhood [22], leading to inadequate attachment [23] and affecting the child’s cognitive and emotional development [20].
Even though much has been written about the organisation of perinatal care [24] and many researchers stress the importance of cooperation in the chain of care in supporting new parents [25–27], we have only been able to find a few scientific studies on interprofessional cooperation between different facilities in the same chain of care. The mother’s emotional response and relationship to the infant were strengthened in cases where the midwives and district nurses had undergone joint breastfeeding training [28]. There was also a larger increase in breastfeeding frequency in areas where midwives and district nurses actively cooperated compared to areas where individual breastfeeding experts were the norm [29]. A Swedish survey [1] showed that interagency cooperation aimed at providing support to expectant/new parents varied. The most common form of cooperation was coordinated parent training programmes. Cooperation involving joint post-discharge care, such as home visits or breastfeeding clinics, was found in only a few places in Sweden. The main barrier to cooperation was, according to the interviewed coordinators, that AC and CHC clinics were in different locations and under separate management. The establishment of “family centres” staffed by both CHC nurses and midwives [30] is a new form of cooperation, but evaluations show that there are also barriers to cooperation even though they work under the same roof [31].
Research from other areas reveals a range of difficulties related to inter organisational cooperation such as conflicts and territorial struggles [32]. Most of the literature in this area, deals, however, with cooperation between different professional disciplines working together in team settings, not with members of the same discipline working in different fields [33]. Such research may also be relevant for this study if the sub-specialties of nursing (midwives and CHC nurses) identify more strongly with their sub-specialty than with the profession as a whole. Research emphasises a range of difficulties in cooperation between different professionals [34, 35] such as a tendency to professional ethnocentricity [36], ignorance about the other party’s area of competence [37] and a tendency among staff to regard their profession as superior to the others [38].
There are a number of reasons why it is now essential to focus on how staff in the different facilities of the chain of care (AC-PC-CHC) experience cooperation and whether they cooperate to decrease gaps in the chain of care. Cooperation in the chain of care is a new area of research and theoretically based studies are sparse [2, 39]. Earlier Swedish pilot studies have presented the perspectives of the coordinators on cooperation in this specific chain of care [1] and of the parents [12] showing that there is a lack of cooperation and that parents lack postnatal support.
Aim
The purpose of the study was to explore the care providers’ experience of cooperation in the AC, PC, and CHC chain of care. Furthermore, the rationale was to conceptualise barriers and facilitators of cooperation in order to generate a comprehensive theoretical model, which may explain variations in the care providers’ experiences.
How do care givers experience cooperation in the chain of care?
What are the barriers to and facilitators of cooperation in the chain of care?
Method
As our purpose was to create new knowledge, i.e. to conceptualise barriers to and facilitators of cooperation in the chain of care in an area where there has been relatively little research, we chose to apply Grounded Theory Methods (GTM) [40–42], which is a methodology aimed at generating theory. GTM is particularly suited when studying interactive processes within an area that is not widely researched and when the pursuit of the study is to arrive at a conceptualisation of a basic social process. In positioning ourselves in the current discussion of GTM (43), we adhere to a classic GTM concerning technique, theoretical sampling and the pursuit of arriving at a theoretical model [40, 43]. The emphasis on conceptualisation is an important part of our approach [41]. We have partly followed Strauss and Corbin’s suggestion for the procedure but, for example, have not used the coding paradigm [44]. Having said this, we believe, however, that the result of a GTM, i.e. the theoretical model, is constructed by the researchers in interaction with data in the way described by Charmaz [43]. This cannot be regarded as an objective process, but the techniques help the researchers to keep track of undue bias and sharpen the researcher’s awareness of their prior theoretical frameworks. Thus we do believe that our research should be positioned within constructivist research, which is also in accord with the roots of GTM, i.e. the symbolic interactionism [45]. For an example of this approach, see Hylander (2003) [42]. In this study, using GTM means generating hypotheses to arrive at a deeper understanding of cooperative processes among CHC nurses and midwives working in the chain of care of AC, PC, and CHC. The study was limited to staff descriptions of cooperation and perceptions of barriers to/facilitators of cooperation among the professionals in AC, PC and CHC. Data were mainly collected using focus group (FG) interviews, which is a suitable method when the aims are to find out how a particular group views a phenomenon and to lessen the guiding role of the interviewer [46–48]. The first author was the moderator for all FG. The moderator introduced the subject but intervened thereafter only if the participants strayed from the subject. The same information about the background and objectives of the study was given to all participants at the beginning of each session. The sessions lasted 60–90 minutes and were recorded and transcribed verbatim. Two individual interviews were conducted in the same manner and lasted 20–30 minutes. Data collection took place over a period of seven months (2006–2007). The first author also conducted the first open coding. The subsequent analyses were a cooperative process between the two authors who attempted to reach consensus. In cases where there was no agreement, the question was left open, until new analyses and data collections pointed towards a solution where consensus was reached.
Setting
The first two FG interviews were conducted at a residential seminar for midwives and the three remaining interviews at an AC clinic and the individual interviews were held at a hospital department in a suburb of a large Swedish city.
Participants
The sample consisted of 32 midwives and CHC nurses who were interviewed in five focus group (FG) interviews and two individual interviews. All interview subjects were women who had worked in their respective fields between 2 and 30 years (average, 12 years). For a description of the sample, see Table 2.
Table 2.
Participants in the different focus groups and individual interviews
| Midwives in AC | Midwives in PC | CHC nurses | |
|---|---|---|---|
| Focus group 1 | 7 | ||
| Focus group 2 | 5 | ||
| Focus group 3 | 6 | ||
| Focus group 4 | 5 | ||
| Focus group 5 | 3 | 2 | 2 |
| Individual | 2 | ||
| Total | 15 | 4 | 13 |
AC = Antenatal care. PC =Postpartum care. CHC = Child health care.
The sample included 13 CHC nurses from 9 CHC clinics, 15 midwives from 8 AC clinics, and 4 midwives from one hospital with two different postpartum departments. The high workload at the hospital made it difficult to gather a group of postpartum midwives in an FG study and two individual interviews were conducted instead. This is a limitation of the study, which is partly overcome by the fact that most midwives interviewed have experience from working in postpartum wards as well as AC. This issue is further discussed in connection with theoretical sampling.
Procedure and data analysis
A theoretical sample was used in accordance with GTM [40], meaning that the emerging theoretical model was allowed to govern the selection of interview subjects and design of the interview guide. Sampling was refined from open to strategic to variation and, finally, to selective sampling [41–42]. To ensure that each professional group could freely express their thoughts, the first four group interviews were conducted in homogeneous groups [48] two separate groups with AC midwives and two with CHC nurses separately. A semi-structured interview guide was used for the study, with the questions ranging from a broader perspective to a more specific one [49]. The subjects covered in the interview guide were cooperation in the chain of care, parental support, and barriers to/facilitators of cooperation. Open coding of the first two FG transcriptions gave a code list of 28 codes and 9 categories. To fill categories, we decided to conduct two more heterogeneous FGs in homogenous groups for which a new interview guide was subsequently designed based on the categories developed from the first two FGs. Questions about meaningful and meaningless cooperation were added. All transcripts were coded according to the coding list and new codes were added and categories were collapsed or developed into main categories with several subcategories. Patterns began to emerge and we could construct some hypotheses that guided the last interviews. Differences in experiences of the professionals in the different facilities had been obvious, which we now wanted to explore further. One of these hypotheses was that: in spite of a common vision of cooperation in the chain of care, the experiences of and the promotion of cooperation varied between the facilities. It was also clear that even though midwives in AC usually have experience from postpartum wards, in order to get a clear picture, midwives in the postpartum ward should be included. Thus the 5th FG included AC and PC midwives and CHC nurses and focused on barriers and facilitators. In order to increase the variation and saturate the categories, two additional interviews were conducted with postpartum midwives, using a further refined interview guide. Theoretical saturation was determined when the categories were adequately filled and no additional categories had emerged. The different patterns, i.e. how the categories could be linked together, were analysed. Strategy was used as a theoretical code in addition to barriers/facilitators.
Ethical considerations
All participants gave their informed consent and confidentiality was assured before the interviews. The regional ethical vetting board in Stockholm approved the study (2006/816-31).
Results
The result of the study is a grounded theory of professional cooperation or linkage in the three-link AC-PC-CHC chain of care. The core category ‘linkage in the chain of care’, concerns how the professionals (in this case, CHC nurses and midwives) in the different links of the chain cooperate to secure a chain of care. Linkage can be described by its three strategies (three categories with subcategories) and by its barriers/facilitators (three categories with sub-categories), see Table 3. Professional care in AC, PC and CHC may be described as a chain in which each facility constitutes a link; they may function as separate links or be linked to form the AC-PC-CHC chain of care. A chain of care is the case when professionals in the different facilities cooperate in order to help the expectant/new parents to know where to turn and to get a high-quality care. The hypothesis rendered in this study is that experiences of linkage vary among the CHC nurses and midwives from the different facilities, depending on the position in the chain of care, whether the staffs have a chain of care or a link perspective and whether staffs believe linkage will result in a professional gain or can discern a parental gain as a result of the linkage. Linkage may occur in three different ways; through transfer of information or problematic cases; through connection (joint activities); or through adjustment, which is aimed at achieving consensus.
Table 3.
The core category-linkage in the chain of care (AC-PC-CHC)
| Categories | Subcategories | |
|---|---|---|
| Strategies for linkage | Transfer | Information transfer Transfer of women who need special support |
| Connection | Joint meetings Joint home visits Joint parent training Joint breastfeeding support |
|
| Adjustment | Establish joint policy | |
| Factors that facilitate/impede linkage | Position in the chain of care | First link Middle link Last link |
| Perspective on the chain of care | Link perspective Chain of care perspective |
|
| Chain of care gain | Professional gain Perceived parental gain |
The interview subjects believed that parents were lost in the chain of care and that there is a consequent need for a closer linkage. There is, however, a gap between the vision of cooperation expressed by staff in all links and that, which actually seems to be achieved:
“If you can’t see the gains of cooperation, you are not interested in it,” (CHC nurse J).
“Now it is like we don’t cooperate, we are totally different facilities, we have to increase our cooperation,” (CHC nurse B).
“Cooperation is positive, we really have a true motivation, we just have to find the tools for a working cooperation,” (AC midwife I).
Strategies for linkage
Midwives and CHC nurses spoke of three different types of linkage in the chain of care that they were involved in. Transfer refers to information transfer as well as transfer of care, concerning women who need special support. Connection refers to joint activities among themselves and staff from different facilities. Adjustment refers to changing policies and patient information towards consensus.
Transfer
Information transfer
CHC nurses in particular complained of a lack of strategies for information transfer that could link more closely the chain of care. CHC nurses thought that PC midwives call them too infrequently, that documentation on new parents arrives too late, and that charting is inadequate. They wanted more information from PC and AC and quick notice from PC when a baby had been born so they could contact the family and the baby did not ‘pop up’ out of the blue:
“It’s a surprise every day when the phone rings— four new babies, oh boy! It’s too much, you don’t hardly have the energy to say congratulations,” (CHC nurse I).
All agreed that AC and PC midwives were responsible for informing parents that they needed to contact CHC but that this does not always happen.
PC midwives agreed that they rarely called CHC, but when they did call, they wanted immediate contact, but were often met by an answering machine:
“It’s a problem: you never get in touch with CHC”, (PC midwife P).
Transfer of care concerning women who need special support
CHC nurses in particular expressed the desire for information about parents who need early contact. AC midwives also wanted to cooperate, since as they believe that psychological problems have increased among pregnant women, and they do not want to “dump tricky situations on CHC.” With regard to AC, CHC nurses wanted information about families with special requirements who might need an immediate home visit:
“It takes unnecessarily long for us to find out what AC has already discovered about families who need extra support. During the time it takes for us to identify the problem ourselves, things can get a bit out of hand before you figure out what is going on,” (CHC nurse G).
There were suggestions to overcome this, like joint meetings with the mother who needs special support during pregnancy. Again, this was a suggestion, but few had practical experience of it. It was also emphasised that confidentiality must be observed and that it was important to get the mother’s consent before any reports were provided:
“When we need to report something to CHC nurses you have to have the mothers’ agreements” (AC midwife I).
Connection
Joint meetings
Professionals in all links shared a vision of professional meetings in order to put faces on to the voices and facilitate communication and cooperation:
“I participated in a breastfeeding course together with CHC nurses: it was fun and encouraged our relationship,” (AC midwife I).
The meetings could involve, joint training, breastfeeding study groups or simply a working lunch or observation visits. However, some midwives did not feel that joint meetings with CHC nurses would promote cooperation:
“We just meet but I felt I could have been done without it,” (AC midwife L).
Joint home visits
There were favourable experiences of joint home visits by CHC nurses and AC midwives, that were thought to promote mutual learning. At these visits, the midwife typically initially talks to parents about the birth, before the subject moves to the baby, which provides a natural transition to the CHC nurse:
“If you have a good home visit half the job is done, if we could get AC to join in it would be twice as good, ” (CHC nurses E).
“Midwife could help in home visits if the women have a problem,” (AC midwife A).
Joint parent training
A jointly shared vision of CHC nurses and AC midwives was informing new parents about the CHC organisation during the pregnancy and AC midwives participating in post-discharge parent training sessions at the CHC in order to focus more on parenthood:
“We ought to increase collaboration on parent training, it doesn’t have to be like this…, that here is the end of AC and here starts CHC,” (AC midwife M).
Joint breastfeeding support
Midwives and CHC nurses in all links thought that joint breastfeeding support was important like, for example, in one family centre where nurses and midwives actively cooperated to support parents with breastfeeding; they shared responsibility, always had a breastfeeding advice line open during the day, and cooperated well with primary care physicians. Many post-discharge problems were related to breastfeeding and when women had such breastfeeding problems, they needed help the same day or they would seek emergency care. CHC nurses felt they came into contact with the new mothers too late, because breastfeeding complications had already presented themselves:
“The mother stopped breastfeeding. She said she wanted to breastfeed her baby, but she had not been given any support. I thought ‘so much for the chain of care.’ It was such a disappointment, because it would have taken so little,” (CHC nurse D).
The causes of the problems included that PC midwifes were unable to provide adequate breastfeeding support during the brief hospital stay and new mothers found it difficult to assimilate information about breastfeeding so soon after delivery. PC midwifes, who are supposed to provide support during the first week, felt that the breastfeeding clinic had inadequate resources.
Adjustment
Establish joint policy
That opinions diverged as to how parents should be informed about subjects like breastfeeding, the use of pacifiers, and sleeping positions, became obvious in the FG whose members represented all the links in the chain of care:
“Exactly! You can see why parents can’t make up their minds when we are not even sure ourselves,” (AC midwife M).
Since all links are involved in breastfeeding, the midwives and PCH nurses believed a joint policy was necessary for parents to feel secure:
“We have to arrive at a common breastfeeding support policy, we just can’t send them to the hospital as soon as there is a problem,” (AC midwife F).
“We can’t help saying different things and then perhaps mothers continue to call around until they get similar answers,” (CHC nurse A).
In summary, the midwives and CHC nurses agreed that linkage was virtually non-existent in the chain of care, despite the desire for cooperation and the many suggestions for how such cooperation could be achieved. Many suggestions had been tried, but cooperation had nonetheless fallen by the wayside.
Factors that facilitate/impede linkage
We found three significant main factors that were suggested to contribute to the failure or success of linkage:
Position in the chain of care: whether the CHC nurses/midwives work in a facility that is the first, last, or middle link in the chain of care.
Perspective on the chain of care: Whether the CHC nurses and midwives view their own facility from a link perspective or from a chain perspective.
Chain of care gain: the CHC nurses or midwives may see a professional gain in their daily work in their own facility by linkage and/or they may see a patient gain, i.e. that the patients profit by the linkage.
Position in the chain of care
The first link
AC midwives get to know the pregnant women over a long period and are thus responsible for discovering and passing on information about women who need special support from the other links in the chain of care:
“We have to sound alarm from the very beginning if we suspect something,” (Midwife N).
But they have no specific professional need to communicate with the other links, which may explain perceptions of inadequate communication to PC midwives and CHC nurses.
The middle link
Care episodes are short in PC and they are responsible for the new mother and baby only one week post partum. The middle link needs the first link to have prepared care plans for women who need special support; otherwise the stay in PC may be unnecessarily prolonged:
“We have an extremely short postpartum length of stay so we feel the preparation in AC is very important because we don’t have the time to influence. If you have such a short time, much information will not come through to the mothers,” (PC midwife D).
Otherwise, PC midwives see no personal professional gains from a linkage, but they would like to see a joint policy with regard to breastfeeding.
The last link
The shorter length of stay in PC has increased the workload of CHC nurses, who find it difficult to perform their tasks due to inadequate information transfer. CHC nurses in the last link express the greatest disappointment over the lack of outer frameworks and resources for cooperation:
“I see CHC as the last link in the chain of care and that means that it has to work in the other links and that’s why it is so important with cooperation,” (CHC nurse D)
Perspectives on the chain of care
Link perspective
A link perspective means that one’s own facility is prioritised and actions taken are not seen as part of the chain of care. There are many factors that may promote a link perspective. There are tangible and intangible barriers to linkage.
Tangible barriers, such as physical distance, emphasise a link perspective. This is exemplified in the following example: When AC carried out a reorganisation based on its own organisational needs (a link perspective), this had an adverse impact on the linkage between CHC and AC because their districts no longer overlapped, which supposedly inhibits joint activities and risks that commitment to cooperation will wane:
“We are not tied to specific areas or specific patients, but we meet those who come to us as they come. And we do that because it is most convenient right now,” (AC midwife I).
CHC nurses and midwives do believe that shared premises would facilitate linkage, like in family centres where CHC nurses and midwives can communicate immediately when something happens and CHC nurses can see women during pregnancy. Shared premises are, however, no guarantee for linkage, as there are also family centres where there is no active cooperation between CHC and AC:
“When we were door-to-door it was natural to cooperate, but I have also heard about other others who don’t cooperate although they share the same building,” (AC midwife H).
Intangible barriers to cooperation may consist of task-based or time-based territoriality. Task-based territories are, e.g. when breastfeeding counselling is considered the purview of CHC. Time-based territory implies that PC is responsible for care during the first week post partum. CHC nurses believe breastfeeding is their job, but do not feel this is acknowledged by midwives, who “think they know more than we do,” (CHC nurse M).
Both AC and PC midwives expressed dissatisfaction with the inability of CHC nurses to provide adequate breastfeeding support. They felt CHC nurses’ skills were uneven with respect to breastfeeding and that their own expertise was greater:
“It’s very different how CHC nurses handle breastfeeding, so if they can’t do it, they have to send the mother back to the hospital,” (PC midwife P).
Chain of care perspective
In a chain of care perspective, the midwives and CHC nurses base their reasoning on the entire chain of care and are knowledgeable about and invested in the other links in the chain of care. According to the nurses and midwives, a chain of care perspective demands a personal interest:
“We have worked with cooperation ourselves without getting any extra time for it,” (AC midwife C).
Also the midwives and CHC nurses think that it requires a management function in the organisation that assumes responsibility for general decisions and guidelines for cooperation, rather than measures designed independently by each link. The chain of care perspective seems obvious to the last link, which is dependent on the other ones, and it is also mainly CHC that would like to see outer frameworks for cooperation:
“There should be a structure that says, ‘this is how it’s supposed to be done!’ If we are unsure, how are the parents supposed to feel?” (CHC nurse B).
Midwives and CHC nurses also spoke of previous cooperative efforts that had been built up but had now collapsed. At times, they had failed to realise how well cooperation had worked until after reorganization was a fact, which caused feelings of resignation and fatigue:
“And then I think about how many times the people at the top have us start all over again and, Lord, it takes so much energy. It just finally wears you out,” (AC Midwife J).
Chain of care gain
Professional gain
The professional gain from linkage was perceived differently depending on the position in the chain of care. The professional gain is substantial for CHC, but not so for the other links because linkage results in the greatest professional gain for the organization that comes as the last link in the chain of care. CHC expressed a need for information, joint projects, and a joint policy to perform their tasks well. The joint projects mostly mentioned were joint parent training and joint home visits, which supposedly also give both parts a professional gain, i.e. that the daily work is facilitated for CHC nurses as well as for midwives.
Perceived parental gain
In general, midwives and CHC nurses in all links felt that parents were lost in the chain of care, particularly postpartum, and that they also understood why parents are confused and that they searched extensively for health care and occasionally resorted to emergency rooms. Since the midwives and CHC nurses also felt lost, as a result, women with the same problems were referred to different places and ‘bounced around’:
“There are terrible situations when they don’t feel welcome anywhere, but everyone refers to other agencies,” (PC midwife C).
Thus midwives and CHC nurses could agree on the patient gain that would result from more effective linking:
“Cooperation between antenatal care, postpartum care and child health centres helps the mother not to be confused,” (AC midwife B)
“Cooperating prevents complications, I’m sure. We could certainly do more in primary health by cooperating,” (CHC nurse D).
That parent’s gain through linkage contributes to whether the chain of care perspective or the link perspective will predominate. Midwives and CHC nurses in all links believed that parents would profit from greater consensus, achieved by focusing on parenthood and by bridging the gap between PC and CHC, which is where many parents get lost in the chain of care:
“I can feel that there is a greater need for contact today than before because of the short stay in the hospital,” (PC midwife P).
“There seems to be a gap at the breast feeding, the short time at the PC and then there is a gap before they get to CHC,” (CHC nurse C).
“These days when the woman has been home before they come to CHC, lots of things have happened,” (AC midwife C).
The substantive grounded theory of linkage in the three-link AC-PC-CHC chain of care provides an overall picture of the theoretical model which is shown in Figure 1. This study came up with one main hypothesis. Despite the fact that midwives as well as CHC nurses acknowledge that parents are lost in the chain of care and that they have common visions about cooperation, cooperation is not achieved because of interacting barriers that have different influences on the three links in the chain. Little or no professional gain through cooperation is achieved by the first position in the chain, which, in turn, is suggested to enhance a link perspective. The first link doesn’t need information from the other links and is not dependant on their work. Thus, little cooperation is achieved (no joint activities, no transference of information and no adjusted policy) and therefore they are still lost in the chain of care like the parents. But as they acknowledge that the parents are lost, they retain their vision of cooperation. There is also a proposition concerning facilitators in the chain of care, which is: the last link also gains professionally, as their work will run more smoothly, which in turn enhances a chain perspective. However, for linking to be achieved, all links must be involved. The position in the chain cannot be changed, thus common professional gains and chain perspective must be emphasised for a linkage to take place, which is done through the strategies of connection, transfer and adjustment.
Figure 1.
Theoretical model.
Discussion
The proposed theoretical model yields a hypothesis about why linkage in the chain of care is not achieved, in spite of well-known strategies and in spite of a common understanding of the importance of such linkage. Barriers to linkage are a lack of professional gain or even a professional loss (some of the strategies for linkage may be very time consuming), a link perspective and first position in the chain. Facilitators are a chain perspective, professional gains and last position in the chain. In this study the CHC nurses are those who most strongly promote a linkage and also those who are last in the chain of care and have the greatest gain from linking.
It is thus clear that despite a willingness to cooperate between the links in the chain of care, the actual practice of cooperation is substandard with respect to how the links are joined. This study proposes a number of explanations. The development of a chain of care perspective, where the professionals in each link are able to recognise the patients’ way through the whole chain seems to be a potent facilitator, in contrast to a link perspective, which signifies that the view is limited to the one’s own facility and the needs of that facility. The individual links cannot implement linkage if they lack a distinct chain of care perspective. In this study the CHC nurses and midwives believed that this demands an overriding management function that has adopted a chain of care perspective. According to Rodriguez [24], a programme coordinator can enhance the quality of perinatal care when services are provided in more than one organisation. However, even though written specifications exist for cooperation in the chain of care for both midwives and CHC nurses, the study shows that staff perceives a lack of such structure, which was also obvious in an earlier Swedish survey [1]. Cutbacks in postpartum care may have also enhanced the need for structure and guidelines for providing support to new parents [4, 8, 15].
Physical proximity and common districts are additional significant factors for enhancing a chain of care perspective. Midwives and CHC nurses felt that working under the same roof in family centres facilitated cooperation but was not sufficient: personal commitment was also required, which has been emphasised in several earlier studies [50–51]. The significance of organisational affiliation has also been pointed out [50].
Awareness of a parental gain induces staffs, to adopt a chain of care perspective in the discussions and express a vision of cooperation. Studies [50, 52] confirm that the earlier the focus is put on the patient/client, the easier it is to engender staff commitment to cooperative projects in the chain of care. There were particularly two areas, where a patient gain was prominent: breastfeeding and women with a need for special support. Midwives and CHC nurses felt that new mothers were looking for help in the chain of care primarily with regard to breastfeeding issues, which is consistent with earlier studies [7, 9]. A link perspective had, however, developed, despite the fact that the CHC nurses and midwives could recognise an important patient gain. They had inadequate knowledge of each other’s organizations, concerning problems related to breastfeeding. Territoriality and divergent policies emerged, which confirms earlier findings that midwives and CHC nurses have different perspectives on breastfeeding [53]. The Stockholm County Council has adopted a breastfeeding strategy based on a joint declaration from the WHO and UNICEF, as well as a regional care protocol [9] that calls for equal treatment of all breastfeeding complications. That the study results nevertheless still do not show a consensus on breastfeeding issues may be understood on the basis of our model. Midwives and CHC nurses in all links adopt a link perspective, even though they express explicitly that they do not want parents to be given contradictory advice. But since it is mainly CHC nurses in the last link that discover the contradictory advice and they are primarily the ones who would profit by a consensus, the linkage is not implemented, with the result that parents were perceived as ending up in a no-man’s land. Another connected explanation is the vagueness in role because of the mutual and different expectations among the CHC nurses and midwives concerning breastfeeding, as it has been demonstrated how vague roles can lead to inadvertent neglect of tasks [34].
A clear patient gain was also seen within reference to women who require special support. All links expressed a need to cooperate, concerning women who need such support in the entire chain of care. Nevertheless, in the present study, midwives and CHC nurse’s perceived a lack of communication concerning these women. Researchers [20–21] stress the fact that you can identify women who might experience postpartum depression at the antenatal clinics. This highlights the difficulty of information transfer when it comes to long-term professional–patient relations as is the case between the woman and her midwife during pregnancy and when confidence and consent have the highest priority. Without attending to these issues, the link perspective may not be overcome.
A most significant facilitator seems to involve whether midwives and CHC nurses perceive a professional gain through linkage, i.e. feel that the linkage makes their daily work easier. As time is in short supply for all involved, a perceived professional gain promotes linkage in all parts of the chain. The professional gain is proportional to the position in the chain of care, which is consistent with Lindberg [54], who asserts that staff cannot understand the consequences of their own actions unless they understand what occurs in the subsequent care setting. As the last link, CHC, in particular, perceive a professional gain and are accordingly the main advocates of expanded cooperation. The cooperative projects that were suggested and actually existed were also such that gave both or all parties in the chain of care a professional gain, i.e. joint parent training and in joint home visits. The need for joint parent training, which has been shown to be the most common form of cooperation [1], is supported by a study demonstrating that only 40% of first-time mothers believed they had been prepared for parenthood in the antenatal education classes [55]. The participant in this study believed that joint parent training sessions during pregnancy and early parenthood could be beneficial for expectant and new parents, but again there were only few midwives and CHC nurses actually cooperating in this way.
The participants had positive experiences from joint home visits by CHC nurses and AC midwives but, again, only a few examples were given. Despite the strong evidence that early parent–child interaction is important for the development of the child—and one suggestion to promote this is for the home visit programme of the child health services to be strengthened [56]—there is a tendency in Stockholm County for home visits to decrease [17]. This fact, in relation to early discharge from hospital, may be considered particularly conspicuous.
Methodological considerations
Like all GTM, our theory has explanatory value only for the area in which it emerged: in this case, the AC-PC-CHC chain of care in a suburb of a large Swedish city. But the theory is amenable to application and testing in similar areas. Although thoroughly grounded in data, the theory is nevertheless only a set of assumptions. It can be modified and applied in a wider field through continued grounding in new data. Certainly, one can speculate that the findings may be relevant to many other chains of care in explaining why some professional groups (those in the last link) are the ones that get most frustrated and push for improved cooperation, e.g. within the relation between general practitioners and specialists. Work, fit, and applicability [41] have been examined through interviews with six midwives and CHC nurses to whom the model has been presented. They confirmed that the results rang true and that the theory was meaningful, coherent, and applicable in practice. The use of FG produced rich material. One strength of the study is that the interviewees came from many different AC and CHC clinics, which produced a varied material. Another strength is that the moderator for all interviews had a solid understanding of the various links in the chain of care. While this may also be regarded as a weakness, as prior understanding may constitute a bias, this was offset by analysing the material with a co-researcher with extensive experience in GTM research and by discussing the results at several academic seminars.
Conclusions
Early postnatal discharge is here to stay, but support after deliveries varies a lot and we need more research into how to support the expectant and new parents. This study suggests that one way to give better support could be by increasing the linkage in the chain of care for expectant and new parents. Although staffs in all links of the chain of care agree that such a linkage would be beneficial for expectant and new parents, they also agree on the fact that such a linkage has not been achieved. This study is therefore important as it explains why cooperation is not realised even when there are visions of such cooperation and many concrete proposals for cooperation. Several of the individual results of the study verify earlier research. What is new here is a comprehensive theoretical model for the chain of care perspective and linkage in the chain of care:
Cooperation among between AC-PC-CHC is achieved when there is a common professional gain.
CHC nurses in the last link of the chain of care express the greatest need for cooperation and are the most amenable to adopting a chain of care perspective. Accordingly, they must inform the other links about their need for cooperation.
A distinct patient gain promotes a chain of care perspective in all links, but an overriding structure and management that adopts a chain of care perspective is required to achieve cooperation.
Acknowledgments
Our grateful thanks go to the midwives and CHC nurses who participated in the study and shared their thoughts and experiences.
Contributor Information
Mia Barimani, Centre for Family and Community Medicine, Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Alfred Nobels Allé 12, SE-141 83 Huddinge, Stockholm, Sweden.
Ingrid Hylander, Centre for Family and Community Medicine, Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Alfred Nobels Allé 12, SE-141 83 Huddinge, Stockholm, Sweden.
Funding
Financial support was provided through the Regional Agreement on Medical Training and Clinical Research (ALF) between the Stockholm County Council and the Karolinska Institute. We would also like to thank Stiftelsen Allmäna barnbördshusets Minnesfond (the General Maternity Hospital Foundation) and Barnets Lyckopenning for their financial support.
Reviewers
Sue Douglas, Dr., MD CCFP (Canada), Senior Lecturer, Academic Unit of General Practice and Community Health, Australian National University, The Canberra Hospital, Woden, Australia
Karin Forslund Frykedal, PhD, Department of Behaviour Sciences and Learning, Linköping University, Linköping, Sweden
Charo Rodriguez, MD, PhD, Associate Professor, Area of Health Services and Policy Research, Department of Family Medicine, McGill University, Montreal, Quebec, Canada
References
- 1.Barimani M. Samverkan mödrahälsovård och barnhälsovård: hur ser det ut? [Collaboration between Antenatal Care and Child Health Care: how does it look?]. Jordemodern. 2006 Nov;:32–3. [in Swedish] [Google Scholar]
- 2.Danermark B, Kullberg C. Samverkan: välfärdsstatens nya arbetsform. [Collaboration: The new working methods of the welfare state]. Lund: Studentlitteratur; 1999. [in Swedish] [Google Scholar]
- 3.Ahgren B. Chain of care development in Sweden: result of a national study. International Journal of Integrated Care [serial online] 2003 Oct 7;3 Available from: http://www.ijic.org. [PMC free article] [PubMed] [Google Scholar]
- 4.Regional Care Protocol. Normal graviditet, förlossning och eftervård. [Normal pregnancy, delivery and post partum care]. Stockholm: Läns Landsting; 2005. [County Council] [in Swedish] [Google Scholar]
- 5.Brumfield C, Nelson K, Stotser D, Yarbaugh D, Patterson P, Sprayberry N. 24-hour mother-infant discharge with a follow-up home health visit: results in a selected Medicaid population. Obstetrics and Gynaecology. 1996;88:544–8. doi: 10.1016/0029-7844(96)00267-0. [DOI] [PubMed] [Google Scholar]
- 6.Brown S, Small R, Faber B, Krastev A, Davis P. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database of Systematic Reviews. 2002;3 doi: 10.1002/14651858.CD002958. CD002958. [DOI] [PubMed] [Google Scholar]
- 7.Ellberg L, Lundman B, Persson MEK, Hogberg U. Comparison of health care utilization of postnatal programs in Sweden. Journal of Obstetric, Gynaecologic, and Neonatal Nursing. 2005;34:55–62. doi: 10.1177/0884217504273128. [DOI] [PubMed] [Google Scholar]
- 8.State of the Art. Handläggningen av normal förlossning. [Dealing with normal delivery]. Swedish National Board of Health and Welfare; 2001. [in Swedish] [Google Scholar]
- 9.Regional Care Protocol. Bröstkomplikationer i samband med amning. [Breast complications in relation to breastfeeding]. Stockholm County Council; 2008. [in Swedish] [Google Scholar]
- 10.Socialstyrelsen. Socialstyrelsens råd om tidig hemgång efter förlossningen. [The Swedish National Board of Health and Welfare’s recommendations concerning early discharge after delivery]. Swedish National Board of Health and Welfare; 1993. [in Swedish] [Google Scholar]
- 11.De Vries RA. Midwives and maternity care in the Netherlands. London: Temple University Press; 2004. Pleasing birth. [Google Scholar]
- 12.Barimani M. En fokusgruppstudie om kvinnors upplevelse av första tiden efter barnets födelse. [A study using focus group discussions about women’s experience of the first six month post partum]. Degree Project in Reproductive and Perinatal Health Care. 2005 [in Swedish] [Google Scholar]
- 13.Darj E, Stålnacke B. Very early discharge from hospital after normal deliveries. Uppsala Journal of Medical Sciences. 2000;105:57–66. doi: 10.1517/03009734000000047. [DOI] [PubMed] [Google Scholar]
- 14.Hildingsson I, Thomas J. Women’s perspectives on maternity services in Sweden: processes, problems, and solutions. Journal of Midwifery and Women’s Health. 2007;52(2):126–33. doi: 10.1016/j.jmwh.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 15.Waldenström U, Rudman A, Hildingsson I. Intrapartum and postpartum care in Sweden: women’s opinions and risk factors for not being satisfied. Acta Obstetricia et Gynecologica. 2006;85:551–60. doi: 10.1080/00016340500345378. [DOI] [PubMed] [Google Scholar]
- 16.Ellberg L, Lundman B, Persson MEK, Hogberg U. Comparison of health care utilization of postnatal programs in Sweden. Journal of Obstetric, Gynaecologic and Neonatal Nursing. 2005;34:55–62. doi: 10.1177/0884217504273128. [DOI] [PubMed] [Google Scholar]
- 17.Child Health Centers in Stockholm. Barnhälsovård—folkhälsoarbete: Årsrapport. [Child health care—public health care: Annual Report]. Stockholm: County Council; 2007. [in Swedish] [Google Scholar]
- 18.Hallberg AC, Lindbladh E, Peterson K, Råstam L, Håkansson A. Swedish child health care in a changing society. Scandinavian Journal of Caring Sciences. 2005;19:196–203. doi: 10.1111/j.1471-6712.2005.00339.x. [DOI] [PubMed] [Google Scholar]
- 19.Hwang P, Wickberg B. Föräldrastöd och spädbarns psykiska hälsa. [Parent support and the Mental Health of the infant]. Stockholm: Swedish National Institute of Public Health; 2001. [in Swedish] [Google Scholar]
- 20.Josefsson A, Angelsiöö L, Berg G, Ekström CM, Gunnervik C, Nordin C, Sydsjö G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstetrics and Gynaecology. 2002;99(2):223–8. doi: 10.1016/s0029-7844(01)01722-7. [DOI] [PubMed] [Google Scholar]
- 21.Rubertsson C, Wickberg B, Gustavsson P, Rådestad I. Depressive symptoms in early pregnancy, two months and one year postpartum—prevalence and psychosocial risk factors in a national Swedish sample. Archives of Women’s Mental Health. 2005;8(2):97–104. doi: 10.1007/s00737-005-0078-8. [DOI] [PubMed] [Google Scholar]
- 22.Seimyr L, Edhborg M, Lundh W, Sjogren B. In the shadow of maternal depressed mood: experiences of parenthood during the first year after childbirth. Journal Psychosomatic Obstetric Gynecology. 2004;25(1):23–34. doi: 10.1080/01674820410001737414. [DOI] [PubMed] [Google Scholar]
- 23.Edhborg M, Matthiessen AS, Lund W, Widström A-M. Some early indicators for depressive symptoms and bonding 2 months postpartum—a study of new mothers and fathers. Archives of Women’s Mental Health. 2005;8(4):221–31. doi: 10.1007/s00737-005-0097-5. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez C, Rivieres-Pigeon C. A literature review on integrated perinatal care. International Journal of Integrated Care [serial online] 2007 Jul 19;(7) doi: 10.5334/ijic.202. Available from: http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nyqvist KH, Kylberg E. The role of the Swedish child health services in breastfeeding promotion. Acta Paediatrica Supplement. 2002;89:57–64. doi: 10.1111/j.1651-2227.2000.tb03097.x. [DOI] [PubMed] [Google Scholar]
- 26.Nyström K, Ohrling K. Parenthood experiences during the Child’s first year: literature review. Journal of Advanced Nursing. 2004;46:319–30. doi: 10.1111/j.1365-2648.2004.02991.x. [DOI] [PubMed] [Google Scholar]
- 27.Warren P. First-time mothers: social support and confidence in infant care. Journal of Advanced Nursing. 2005;50:479–88. doi: 10.1111/j.1365-2648.2005.03425.x. [DOI] [PubMed] [Google Scholar]
- 28.Ekström A, Nissen E. A mothers feelings for her infant are strengthened by excellent breastfeeding counselling and continuity of care. Pediatrics. 2006;118:309–14. doi: 10.1542/peds.2005-2064. [DOI] [PubMed] [Google Scholar]
- 29.Hoddinott P, Pill R, Chalmers M. Health professionals, implementation and outcomes. Reflections on a complex intervention to improve breastfeeding rates in primary care. Family Practice. 2007;24:84–91. doi: 10.1093/fampra/cml061. [DOI] [PubMed] [Google Scholar]
- 30.Swedish National Institute of Public Health. Att verka tillsammans—en bok om familjecentraler. [Working together—a book about family centers]. Stockholm: FHI; 2000. [in Swedish] [Google Scholar]
- 31.Hylander I. Utvärdering av familjestödjande åtgärder. Delutvärdering av projektet “Barns och ungdomars bästa”. [Evaluation of family support measures. “An evaluation of the project, The Best for Children and Adolescents”]. Linköping: Centrum för kommunstrategiska studier; 2005. [in Swedish] [Google Scholar]
- 32.Granström K. Three models for collaboration. Modes of describing collaboration between pre-school teachers and school teachers. Paper presented at The 12th European Conference on Quality in Early Childhood Education. Nicosia. 2002 Aug;:28–31. [Google Scholar]
- 33.Amir V, Auslander G. Inter-organizational collaboration among social workers: the case of community mental health centers and local social service department in Israel. British Journal of Social Work. 2003;33:557–66. [Google Scholar]
- 34.Blomqvist S. Ju mer vi är tillsammans: Mångprofessionellt teamarbete i vården. [The more we cooperate: multiprofessional teamwork in healthcare]. Linköping: Department of Behavioural Sciences, Linköping University; 2004. (FOG-rapport; 50). [in Swedish] [Google Scholar]
- 35.Herrman H, Trauer T, Warnock J. The roles and relationships of psychiatrists and other service providers in mental health services. Australian and New Zealand Journal of Psychiatry. 2002;36:75–80. doi: 10.1046/j.1440-1614.2002.00982.x. [DOI] [PubMed] [Google Scholar]
- 36.Schofield RF, Amodeo M. Interdisciplinary teams in health care and human services settings: are they effective? Health and Social Work. 1999;24:210–9. doi: 10.1093/hsw/24.3.210. [DOI] [PubMed] [Google Scholar]
- 37.Waskett C. Multidisciplinary teamwork in primary care: The role of the counsellor. Counselling Psychology Quarterly. 1996;9:243–60. [Google Scholar]
- 38.Abramsons JS. Making teams work. Social Work with Groups. 1990;12:45–63. [Google Scholar]
- 39.Ahgren B, Axelsson R. Evaluating integrated health care: a model for measurement. International Journal of Integrated Care [serial online] 2005 Aug 31;5 doi: 10.5334/ijic.134. Available from http://www.ijic.org. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glaser B, Strauss A. New York: Aldine de Gruyter; 1967. The discovery of grounded theory. Strategies for qualitative research. [Google Scholar]
- 41.Glaser B. Advances in the methodology of Grounded Theory. Mill Valley (CA): Sociology Press; 1978. Theoretical Sensitivity. [Google Scholar]
- 42.Hylander I. Toward a grounded theory of the conceptual change process in consulted-centered consultation. Journal of Educational and Psychological Consultation. 2003;14:263–80. [Google Scholar]
- 43.Charmaz K. Grounded theory in the 21 century. In: Denzin NK, Lincoln YS, editors. The Sages handbook of qualitative research. 3th ed. London: Sage Publications; 2005. pp. 507–35. [Google Scholar]
- 44.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks (CA): Sage; 1998. [Google Scholar]
- 45.Blumer H. Symbolic interactionism: Perspective and method. Berkeley (CA): University of California Press; 1969. [Google Scholar]
- 46.Barbour RS, Kitzinger J. Developing focus group research. London: Sage Publications; 2001. [Google Scholar]
- 47.Kreuger RA, Casey MA. Focus Groups, a practical guide for applied research. Thousand Oaks (CA); London: Sage publications; 2000. [Google Scholar]
- 48.Wibeck V. Fokusgrupper- om fokuserade gruppintervjuer som undersökningsmetod. [Focus groups—on focused group interviews as a research method]. Lund: Studentlitteratur; 2000. [in Swedish] [Google Scholar]
- 49.Kreuger RA. Developing questions for focus groups (The Focus Group Kit, no 3) Thousand Oaks (CA): Sage; 1998. [Google Scholar]
- 50.Hjalmarson I, Norman E. Samverkan: enkelt i teorin -svårare att praktisera. [Cooperation: simple in theory but difficult in practice]. Rapporter/stiftelsen Stockholms läns äldrecentrum. 2005 [in Swedish] [Google Scholar]
- 51.Frih C, Steen I. En studie av förebyggande arbete i tre samverkansprojekt kring barn och unga. [A study of preventive work in three projects of cooperative projects involving children and adolescents]. Bräkne-Hoby: Copygraf; 1999. Rapport-fokus. [in Swedish] [Google Scholar]
- 52.Åhgren B. Vårdkedjan—vårdkonsumism och patientfokusering processinriktar sjukvården. [The chain of care—care consumerism for a process-focused health care]. Lund: Studentlitteratur; 1999. [in Swedish] [Google Scholar]
- 53.Ekström A, Matthiesen AS. Widström AM, Nissen E. Breastfeeding attitudes among counselling health professionals. Scandinavian Journal of Public Health. 2005;33:353–9. doi: 10.1080/14034940510005879. [DOI] [PubMed] [Google Scholar]
- 54.Lindberg K. Kopplandets kraft: om organisering mellan organisationer. [The power of connection: on organization between organizations]. Göteborg: BAS; 2002. [in Swedish] [Google Scholar]
- 55.Fabian H, Rådestad I, Waldenström U. Childbirth and parenthood education classes in Sweden. Women’s opinion and possible outcomes. Acta Obstetricia Gynecologica Scandinavia. 2005;84:436–43. doi: 10.1111/j.0001-6349.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- 56.Sundelin C, Håkansson A. The importance of the child health services to the health of children. Acta Paediatrica Supplement. 2000;88:1356–63. doi: 10.1080/080352500750027448. [DOI] [PubMed] [Google Scholar]