Summary
Data are reported on a series of 52 endoscopic procedures of dacryocystorhinostomy, performed in the Department of Otorhinolaryngology of the Hospital of Varese, between May 1999 and February 2003. The study population comprised 42 patients (32 female, 10 male, mean age 57 and 51 years, respectively) with naso-lacrimal obstruction. In all cases, pre-operative diagnosis consisted in irrigation of the lacrimal pathways, confirmed on dacryocystography; in selected cases, an additional computed tomography examination was carried out. All procedures were performed under general anaesthesia and surgical times were recorded; mean time for primary dacryocystorhinostomy was 30 minutes. A silicone tube was inserted in all patients for a period of 3 months. The procedure was successful in 81% of primary dacryocystorhinostomy cases and in 75% of revision dacryocystorhinostomy cases. Personal clinical and surgical experience, focusing on surgical techniques used in dacryocystorhinostomy, is described.
Keywords: Naso-lacrimal obstruction, Surgical treatment, Dacryocystorhinostomy, Endoscopic surgery
Riassunto
Vengono riportati i dati relativi a 52 interventi di dacriocistorinostomia (DCR) primaria endoscopica per stenosi delle vie lacrimali, eseguiti presso la Divisione di Otorinolaringoiatria dell’Ospedale di Circolo di Varese, dal Maggio 1999 al Febbraio 2003. La popolazione in studio comprende 42 pazienti, 32 di sesso femminile e 10 di sesso maschile, con età media rispettivamente di 57 e di 51 anni. La diagnosi si è avvalsa in tutti i casi del lavaggio delle vie lacrimali e della dracriocistografia (DCG), affiancata, in casi accuratamente selezionati, dalla tomografia computerizzata (TC). Il tempo operatorio medio delle procedure, eseguite tutte in anestesia generale, è stato di circa 30 minuti, progressivamente diminuito con l’acquisizione di manualità chirurgica. In tutti i pazienti è stato posizionato uno stent in silicone che è stato rimosso dopo 3 mesi. Nell’81% dei casi la stomia è rimasta pervia al controllo in corso di follow-up (8-56 mesi). Dieci pazienti (19%) hanno manifestato ripresa della malattia, 8 casi sono stati sottoposti ad un secondo intervento di DCR per via endoscopica con esito positivo nel 75% dei casi. Proponiamo qui di seguito la nostra esperienza clinico-chirurgica ed alcune puntualizzazioni riguardo la tecnica operatoria.
Introduction
Stenosis of the nasolacrimal drainage system is encountered in clinical practice both by Ophthalmologists and Otorhinolaryngologists 1–4.
Causes are sometimes acute and chronic inflammation, trauma and congenital malformations. Present-ing symptoms include chronic epiphora, swelling of the lacrimal sac (LS) with subsequent dacryocystitis, and recurrent conjunctivitis. Endoscopic dacryocystorhinostomy (DCR) is indicated when medical therapy has failed to achieve resolution of the disease.
Since 1904 5, the surgical management accepted for this disease was the external approach, although Caldwell 6 was the first to propose, in 1893, the endonasal approach, unfortunately limited by the technology, at that time. The introduction of endoscopes with different degrees of angulation for endoscopic sinus surgery, led to widespread use of endoscopic DCR. The procedure is a valid alternative approach for nasolacrimal canal obstruction. The advantages of the endoscopic approach are minor traumatization, preservation of lacrimal pump function, and reduction of surgical time. The success rate of endoscopic DCR is comparable to that of the traditional external procedure, with minimal morbidity and the possibility to treat simultaneous sinonasal diseases 7–16.
Personal clinical and surgical experience are herein described and surgical techniques, results and follow-up of DCR are discussed
Material and methods
Between May 1999 and February 2003, 68 endoscopic DCR procedures have been performed at the Department of Otorhinolaryngology, Hospital of Varese. Four cases, performed during surgery for sinonasal neoplasms, and 12 cases that required re-operation (9 previously treated elsewhere) were excluded from the present study. Data were collected on 52 primary endoscopic DCR in 42 patients of whom 32 female, mean age 57 years (range 29-78), and 10 male, mean age 51 years (range 25-76).
Ten patients underwent a bilateral procedure, 6 of them, at the same time. One patient had been treated some years earlier, by an external approach, at another hospital. Another case presented post-traumatic stenosis due to maxillary bone fractures which had occurred at the age of 3 years. All patients presented epiphora, associated in 21 cases, with at least one episode of acute dacryocystitis. In 4 cases, a mucopurulent secretion from the lacrimal pathways was detected. In all cases, pre-operative diagnosis consisted in irrigation of the lacrimal pathways and dacryocystography; in 8 selected cases computerized tomography (CT) scan examination was performed. In 4 cases, the endoscopic DCR was associated with an osteocartilagineous septoplasty (3 of which endoscopically); in 2 cases, DCR was associated with functional endoscopic sinus surgery (FESS) for inflammatory diseases.
All procedures were performed under general anaes-thesia, by one surgeon (L.M.), and surgical times were recorded. Our surgical techniques have changed over the years. In the first group of 20 patients, after incision of the mucosal flap, we proceeded to drill the maxillary process until identification of the LS, on the hypothetical projection of the LS, identified by the maxillary line. In some cases, a light source was used to identify the LS. In the second group of 22 patients, after harvesting a posteriorly based muco-periosteal flap, we detected the medial aspect of the LB, with partial resection of the uncinate process (portion of the vertical aspect) when necessary, des-truction of the bone layer and exposure of the LS. The osteotomy was then enlarged, if necessary, from the posterior to anterior way. In both techniques, after exposure of the LS, we make an incision on the LS and remove the medial wall; soft gauze is then placed in the nasal cavity after inserting the silicone stent. Silicone tube was inserted, in all patients, for a period of 3 months. Patients were treated in day-hospital regimen and underwent medications on day 7 and irrigation of the lacrimal pathways on post-operative days 1, 7 and 30.
Results
In 42 cases (81%), epiphora is no longer present and irrigation of the lacrimal pathways is free with a follow-up ranging between 8 and 56 months.
Ten patients (19%) reported epiphora within a period of 12 months after the surgical procedure, and one patient, 30 months after surgery.
Eight patients underwent a second endoscopic DCR, with a mean surgery time of 25 minutes. Two patients refused the operation.
In 2 cases the stent was accidentally removed, and in one of them it was reinserted on day VI on account of recurrent symptoms. As far as concerns the 8 patients undergoing a second procedure, 6 (75%) did not present epiphora, with a follow-up ranging from 3 to 12 months from the second procedure.
Two patients had recurrent symptoms and only one was treated with a third endoscopic DCR after 3 months on account of recurrence of stenosis.
Mean time for primary DCR was 30 minutes, range 15-110 minutes; time progressively decreased with increasing surgical expertise. Post-operative complications included eyelid oedema in one case, treated with topical anti-inflammatory therapy.
Discussion
To establish correct diagnosis and consequently proper management, it is necessary to localize the obstruction in order to rule out a pre-saccal stenosis and detect the LS and eyelid diseases 17.
In this study, we employed a simplified diagnostic protocol without routine use of CT scan imaging 18–25.
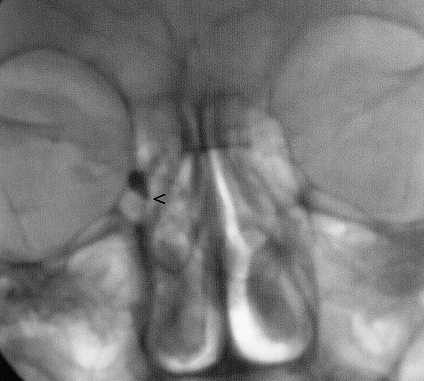
Irrigation of the lacrimal system establishes correct diagnosis, being an easy, safe, and low cost examination. DCG (Fig. 1) visualizes the exact location of the obstruction and the size of the LS, and detects subtotal stenosis of the lacrimal pathway. This examination allowed us to detect two cases of subtotal stenosis, treated with dilatation and stent insertion, avoiding surgery. Mannor et al. 26 reported a success rate of 82% in patients with normal or expanded LS, versus 29% in the case of LS fibrosis.
Fig. 1.
Dacryocystography. Arrow indicates obstruction in lacrimal pathway.
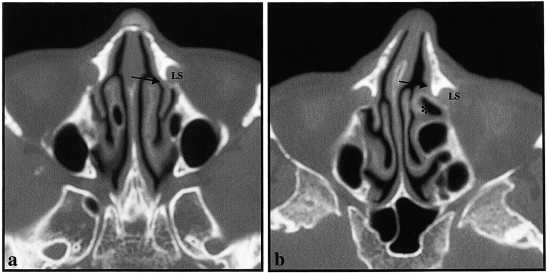
CT scan allows visualization of the anatomy of the bone frame and consequently to detect the position of the uncinate process (UP), and relationship with lacrimal bone (LB) and LS, the presence of a Haller cell, and pneumatization of agger nasi (Fig. 2). In our opinion, most of this anatomical information can be obtained with endonasal endoscopic examinations and any anatomical variants can be managed during the surgical procedure. CT scan imaging is reserved for post-traumatic and malformative cases.
Fig. 2.
Computed tomography scans: a. favourable anatomical conditions for surgical approach; b. difficult case due to particular anatomical findings of anterior ethmoidal cells (asterisk). Arrows indicate surgical approach to identify lacrimal sac.
During identification of LS, transillumination may be misleading due to the variable thickness of the maxillary and lacrimal bones: in fact, the light is projected intensely through the different bone thickness without correct surgical anatomical landmarks. The maxillary process is a solid structure and prolonged drilling is necessary; this determines overheatings around the bone, with an increased risk of scar tissue formation, damaging the adjacent structures. The “retrograde approach” represents a more intuitive surgical approach that frequently detects the correct anatomical landmarks, thus allowing use of the micro-drill to be reduced to a minimum, with subsequent reduction of scar tissues formation. In our study, endoscopic DCR showed a success rate of 81% (follow-up ranging from 8 to 56 months), with complete resolution of symptoms and open pathway, evaluated by irrigation of the lacrimal system. Success rates reported in the literature range from 79.4% to 96% 1 13 27–31.
The endoscopic approach offers many advantages: less skin traumatization and scar tissue, with preservation of lacrimal pump function, avoiding trauma to the medial side tendon 1 15 27 31. Intra-operative bleeding was reduced, thus allowing better visualization of anatomical structures. It may be performed during acute dacryocystitis, where the external access is not indicated 32.
In expert hands, surgical times are reduced: data reported in the literature refer to a mean time, for endoscopic DCR, of 30 minutes, while with the traditional technique, mean time is about 45-50 minutes 33 34. In the present study, except for associated endoscopic procedures, the time required for primary surgical procedures was approximately 30 minutes (range 20-45 minutes) while for secondary procedures, 25 minutes. According to Terbet et al. 33, surgical times are closely related to the surgical experience of the surgeon, confirmed also in our study. Furthermore, this procedure may be performed under local anaesthesia, thus reducing hospitalisation time.
There are also disadvantages related to the use of this technique: the costs of instrumentation are very high; intra-operative bleeding must be avoided; surgical ability requires many years of experience as stressed by many Authors: success rates of 94% and 58% have been reported in two groups of patients that underwent endoscopic DCR, with expert and non-expert surgeons, respectively 3.
The endoscopic DCR surgical technique is not standardized in the literature 35 36.
In our series, some steps in the surgical procedures have been modified, in accordance with changes in the experience of the surgeon: in the majority of cases, osteotomy is performed at the level of the LB with curette instruments and with minimum drilling of the maxillary bone: in the first group of patients, removal of bone was performed with a non-protected drill, causing a reduction in the success rate of this surgical procedure. We observed a 70% failure rate in the first group of 20 patients where the drill was extensively used. In the second group of patients, to avoid this problem we chose the “retrograde approach” with led to the best success rate.
Stent application, associated with topical antibiotic lavage, maintains the lacrimal system open and prevents infections, resulting in a successful outcome. The stent was implanted for approximately 3 months; removal before this time is often the cause of failure. Granulation tissue may be detected after 3 months of stenting 37–39.
Nevertheless, use of the stent is not well established in the literature: according to some Authors, in fact, this procedure is contraindicated on account of an increase in the occurrence of DCR stenosis 40; others 41 42 have described no differences in the success rate using the stent system.
Some Authors have described the use of topical applications of mitomycin-C, 0.2 mg/mL for 25 minutes or 0.5 mg/mL for 30 minutes: this antimetabolite reduces scar formation, determining an increase in the success rate of endoscopic DCR 28 32 43 44. We have no personal experience in the use of mitomycin-C.
Conclusions
In conclusion, endoscopic DCR is a valid alternative to external procedures in the management of nasolacrimal canal obstruction; it is a less invasive procedure, an efficacious method with a high success rate and good outcome.
Current technology, with the introduction of endoscopes and imaging investigations, dedicated to the nasolacrimal system, allow the site of the obstruction to be detected and to perform micro-invasive surgery, respecting the anatomical structures.
References
- 1.Hartikainen J, Antila J, Varpula M, Puukka P, Seppa H, Grenman R. Prospective randomized comparison of endonasal endoscopic dacryocystorynostomy and external dacryocystorhinostomy. Laryngoscope 1998;108:1861-6. [DOI] [PubMed] [Google Scholar]
- 2.Dietrich C, Mewes T, Kuhnemund M, Hashemi B, Mann WJ, Amedee RG. Long-term follow-up of patients with microscopic endonasal dacryocystorhinostomy. Am J Rhinol 2003;17:57-61. [PubMed] [Google Scholar]
- 3.Onerici M. Dacryocystorhinostomy. Diagnosis and treatment of nasolacrimal canal obstruction. Rhinology 2002;40:49-65. [PubMed] [Google Scholar]
- 4.Berlucchi M, Staurenghi G, Rossi Brunori P, Tomenzoli D, Nicolai P. Transnasal endoscopic dacryocystorhinostomy for the treatment of lacrimal pathway stenoses in pediatric patients. Int J Ped Otorhinolaryngol 2003;67:1069-74. [DOI] [PubMed] [Google Scholar]
- 5.Toti A. Nuovo metodo conservatore di cura radicale delle suporazioni croniche del sacco lacrimale. Clin Med Firenze 1904;10:385-9. [Google Scholar]
- 6.Caldwell GW. Two new operations for obstruction of the nasal duct with preservation of the canaliculi and an incidental description of a new lacrimal probe. NY Med J 1893;57:581-2. [Google Scholar]
- 7.Presutti L. Endonasal dacryocystorhinostomy. Acta Otorhinolaryngol Ital 1995;15:449-53. [PubMed] [Google Scholar]
- 8.Bambule G, Chamero J. Endonasal dacryocystorhinostomy (DCR). Rev Med Suisse Romande 2001;121:747-51. [PubMed] [Google Scholar]
- 9.McMasters M, Messerli J, Wolfensberger M. Endonasal dacryocystorhinostomy: technique and results. Schweiz Med Wochenschr 2000;116:745-65. [PubMed] [Google Scholar]
- 10.Zilelioglu G, Tekeli O, Ugurba SH, Akiner M, Akturk T, Anadolu Y. Results of endoscopic endonasal non-laser dacryocystorhinostomy. Doc Ophthalmol 2002;105:57-62. [DOI] [PubMed] [Google Scholar]
- 11.Weidenbecher M, Hosemann W, Buhr W. Endoscopic endonasal dacryocystorhinostomy: results in 56 patients. Ann Otol Rhinol Laryngol 1994;103:363-7. [DOI] [PubMed] [Google Scholar]
- 12.Piane R, Romano L, Nuti D, Romano F, Passali D. Endonasal dacryocystorhinostomy: a personal experience. Acta Otorhinolaryngol Ital 1990;19:255-9. [PubMed] [Google Scholar]
- 13.Par I, Pliskvova I, Plch J. Endoscopic endonasal dacryocystorhinostomy: indications, technique and results. Cesk Slov Oftalmol 1998;54:387-91. [PubMed] [Google Scholar]
- 14.Sprekelsen MB, Barberan MT. Endoscopic dacryocystorhinostomy: surgical technique and results. Laryngoscope 1996;106:187-9. [DOI] [PubMed] [Google Scholar]
- 15.Woog JJ, Kennedy RH, Custer PL, Kaltreider SA, Meyer DR, Camara JG. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology 2001;108:2369-77. [DOI] [PubMed] [Google Scholar]
- 16.Puxeddu R, Nicolai P, Bielamowicz S, Serra A, Puxeddu P. Endoscopic revision of failed external dacryocystorhinostomy. Acta Otorhinolaryngol Ital 2000;20:1-5. [PubMed] [Google Scholar]
- 17.Yung MW, Hardman-Leas S. Analysis of the results of surgical endoscopic dacryocystorhinostomy: effect of the level of obstruction. Br J Ophthalmol 2002;86:792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira L, Dammann F, Duda SH, Reinbold WD, Claussen CD. Value of dacryocystography in localization diagnosis of lacrimal duct stenosis. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 1997;166:498-501. [DOI] [PubMed] [Google Scholar]
- 19.Hansen MH, Albertsen JL, Nepper-Rasmussen HJ, Hecht PS. Preoperative dacryocystography in patients with epiphora. Ugeskr Laeger 1996;158:5022-5. [PubMed] [Google Scholar]
- 20.Helies P, Cosnard G, Pharaboz C, Maille M, Maurin JF. Dacryocystography using CT and MRI. Comparative study apropos of 13 clinical cases. J Fr Ophtalmol 1995;18:763-70. [PubMed] [Google Scholar]
- 21.Caldemeyer KS, Stockbergens SM, Broderick LS. Topical contrast-enhanced CT and MR dacryocystography: imaging of the lacrimal drainage apparatus of healthy volunteers. Am J Roentgenol 1998;171:1501-4. [DOI] [PubMed] [Google Scholar]
- 22.Kallman JE, Foster JA, Wulc AE, Yousem DM, Kennedy DW. Computed tomography in lacrimal outflow obstruction. Ophthalmology 1997;104:676-82. [DOI] [PubMed] [Google Scholar]
- 23.Massoud TF, Whittet HB, Anslow P. CT-dacryocystography for nasolacrimal duct obstruction following paranasal sinus surgery. Br J Radiol 1993;66:223-7. [DOI] [PubMed] [Google Scholar]
- 24.Weber Al, Rodriguez-De Velasquez A, Lucarelli MJ, Cheng HM. Normal anatomy and lesions of the lacrimal sac and duct: evaluated by dacryocystography, computed tomography, and MR imaging. Neuroimaging Clin N Am 1996;6:199-217. [PubMed] [Google Scholar]
- 25.Mafre L, De Maria M, Todaro E, Mangiameli A, Ponte F, Lagalla R. MR dacryocystography: comparison with dacryocystography and CT dacryocystography. Am J Neuroradiol 2000;21:1145-50. [PMC free article] [PubMed] [Google Scholar]
- 26.Mannor GE, Mulman AL. The prognostic value of preoperative dacryocystography in endoscopic intranasal dacryocystorhinostomy. Am J Ophthalmol 1992;113:134-7. [DOI] [PubMed] [Google Scholar]
- 27.Cokkeser Y, Evereklioglu C, Er H. Comparative external versus endoscopic dacryocystorhinostomy: results in 115 patients (130 eyes). Otolaryngol Head Neck Surg 2000;123:488-91. [DOI] [PubMed] [Google Scholar]
- 28.Liu D, Bosley TM. Silicone nasolacrimal intubation with mitomycin-C: a prospective, randomized, double-masked study. Ophthalmology 2003;110:306-10. [DOI] [PubMed] [Google Scholar]
- 29.Zilelioglu G, Ugurbas SH, Anadolu Y, Akiner M, Akturk T. Adjunctive use of mitomycin C on endoscopic lacrimal surgery. Br J Ophthalmol 1998;82:63-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mantynem J, Yoshitsugu M, Rautiainen M. Results of dacryocystorhinostomy in 96 patients. Acta Otolaryngol 1997;529(Suppl):187-9. [DOI] [PubMed] [Google Scholar]
- 31.Dolman PJ. Comparison of external dacryocystorhinostomy with non laser endonasal dacryocystorhinostomy. Ophthalmology 2003;110:78-84. [DOI] [PubMed] [Google Scholar]
- 32.Lee TS, Woog JJ. Endonasal dacryocystorhinostomy in the primary treatment of acute dacryocystitis with abscess formation. Ophthal Plast Reconstr Surg 2001;17:180-3. [DOI] [PubMed] [Google Scholar]
- 33.Tarbet KJ, Custer PL. External dacryocystorhinostomy: surgical success, patient satisfaction and economic cost. Ophthalmology 1995;102:1065-70. [DOI] [PubMed] [Google Scholar]
- 34.Malhotra R, Wright M, Olver JM. A consideration of the time taken to do dacryocystorhinostomy (DCR) surgery. Eye 2003;17:691-6. [DOI] [PubMed] [Google Scholar]
- 35.Eloy P, Bertrand B, Martinez M, Hoebeke M, Watelet JB, Jamart J. Endonasal dacryocystorhinostomy: indications, technique and results. Rhinology 1995;33:229-33. [PubMed] [Google Scholar]
- 36.Tsirbas A, Wormald PJ. Endonasal dacryocystorhinostomy with mucosal flap. Am J Ophthalmol 2003;135:76-83. [DOI] [PubMed] [Google Scholar]
- 37.Soler Machin J, Castillo Laguarta JM, De Gregorio Ariza MA, Medrano J, Cristobal Bescos JA. Lacrimal duct obstruction treated with lacrimonasal stent. Arch Soc Esp Oftalmol 2003;78:315-8. [PubMed] [Google Scholar]
- 38.Bogdanici C, Lupascu C, Halunga M. Complications after catheterization of nasolacrimal duct. Oftalmologia 2002;55:39-42. [PubMed] [Google Scholar]
- 39.Beloglazov VG, Atokova EL, Malaeva LV, Nikol’skaia GM, Azibekian AB, Saad El’din NM. Intubation granulomas of the lacrimal ducts in patients with silicone implants. Vestn Oftalmol 1998;114:29-32. [PubMed] [Google Scholar]
- 40.Allen K, Berlin AJ. Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthalm Surg 1989;20:486-9. [PubMed] [Google Scholar]
- 41.Walland MJ, Rose GE. The effect of silicone intubation on failure and infection rates after dacryocystorhinostomy. Ophthalmic Surg 1994;25:597-600. [PubMed] [Google Scholar]
- 42.Unlu HH, Ozturk F, Nutlu C, Ilker SS, Tarhan S. Endoscopic dacryocystorhinostomy without stents. Auris Nasus Larynx 2000;27:65-71. [DOI] [PubMed] [Google Scholar]
- 43.Camara JG, Bengzon AU, Henson RD. The safety and efficacy of Mitomycin C in endonasal endoscopic laser-assisted dacryocystorhinostomy. Ophthal Plast Reconstr Surg 2000;16:114-8. [DOI] [PubMed] [Google Scholar]
- 44.Selig YK, Biesman BS, Rebeiz EE. Topical application of Mitomycin C in endoscopic dacryocystorhinostomy. Am J Rhinol 2000;14:205-7. [DOI] [PubMed] [Google Scholar]