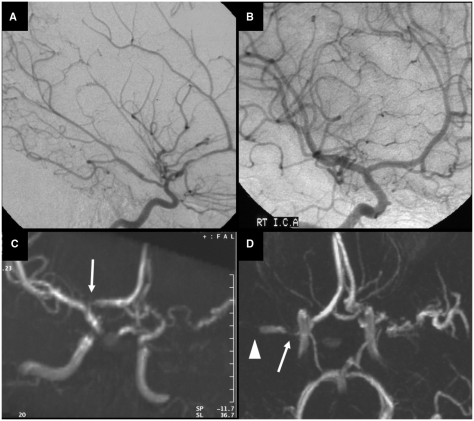
Fig. 6.
Progressive arteriopathy in a girl who initially presented with an ischaemic stroke in the left basal ganglia and loss of flow voids in the left ICA and proximal MCA on MRA, 8 days after stroke. She was treated with aspirin and was left with a moderate right hemiparesis and some comprehension and word-finding difficulties. Conventional angiography at 3 months after stroke showed vasculopathy affecting the left side (A) but the right was normal (B). Further MRA 9 months later (C) suggested abnormality of the right proximal ACA (arrow), but the findings were interpreted cautiously in view of the image quality and it was not considered ethical to repeat the conventional arteriography. Three months later, she had a contralateral infarct on MRI, involving the right basal ganglia and insular region (not shown). MRA (D), confirmed by conventional angiography, then showed bilateral arteriopathy with proximal stenosis of the right MCA (arrow) and a more distal occlusion of the right M1 segment (arrow head), as well as irregular stenosis of the left MCA.