Abstract
“Truth is the daughter of Time,” said mystery writer Josephine Tey. This point, illustrated in her rehabilitation of the “villainous” King Richard III, is equally apt for a reconsideration of the 1991 Barer–Stoddart report on medical personnel. Canadian physicians have reviled these authors for “creating” a physician shortage by encouraging provincial cuts to medical school enrolment. Yet, data pre- and post-1991 are quite clear: their report did not and could not have had this effect. The physician-to-population ratio has been stable since 1989. Average physician hours of work have fallen, but per capita expenditures on physicians' services (inflation-adjusted) are rising rapidly. A flood of physicians from the major expansion of enrolments now in place threatens serious fiscal trouble over the next two decades, and is likely to pre-empt any significant system reform.
Abstract
《 La vérité est la fille du temps 》, soutient l'auteure de romans-mystère Josephine Tey. Cet argument, illustré par sa réhabilitation du 《 méchant 》 roi Richard III, vaut tout autant pour un réexamen du rapport de 1991 de Barer–Stoddart sur le personnel médical. Les médecins canadiens ont reproché aux auteurs du rapport d'avoir 《 créé 》 une pénurie de médecins en encourageant les gouvernements provinciaux à réduire le budget consacré aux inscriptions dans les écoles de médecine. Pourtant, les données recueillies avant et après 1991 sont très claires : leur rapport n'a pas eu et n'aurait pas pu avoir un tel effet. Le nombre de médecins par rapport à la population est stable depuis 1989. Le nombre moyen d'heures de travail des médecins a diminué, mais les dépenses par habitant en services médicaux (ajustées en fonction de l'inflation) augmentent rapidement. L'arrivée massive de médecins à la suite d'importantes initiatives mises de l'avant pour accroître le nombre d'inscriptions dans les écoles de médecine pourrait créer de graves problèmes fiscaux au cours des 20 prochaines années et risque d'entraver toute réforme significative du système.
King Richard III has acquired rather a bad reputation. Coming to the throne by murdering everyone in his way, and in particular the two sons of his brother Edward IV (“the little princes in the Tower,” Edward V and the Duke of York), was bound to excite some unfavourable comment. After all, Edward Sr. had appointed Richard their guardian. By the time Shakespeare was through with him, Richard was a monster of evil incarnate.
Shakespeare was a dramatist, not a historian. He was also writing during the reign of Elizabeth I. She was not only extremely popular – she is still great box office – but was also the granddaughter of Henry Tudor, who became King Henry VII after his supporters defeated and killed Richard. So Shakespeare knew how his bread was buttered when he had Richard declare his intention:
“… since I cannot prove a lover [because of his physical deformity] … I am determined to prove a villain … .”
(Richard III, act I, scene 1)
He does, in spades.
There is in fact no evidence that Richard was deformed, and Shakespeare has him strategically seducing and marrying Anne Neville, whose father and brother he had murdered. So the motivation for his bottomless evil is obscure. Poetic licence.
Over the centuries, however, historical revisionism has poked serious holes in the Shakespearian account, and there is today an entire society dedicated to the rehabilitation of Richard III, as at least innocent of the murder of the little princes. Certainly, his successor was a master of political propaganda, and a large number of key documents seem to have disappeared during Henry's reign. Nor, strangely, did Henry ever produce the bodies. The mystery of the little princes has never been satisfactorily solved. The dissenting argument is put, very readably, as a detective novel by Josephine Tey in The Daughter of Time.
It is in this spirit that we revisit the work of two more recent villains, Morris Barer and Greg Stoddart, who in the notorious Barer–Stoddart report nearly 20 years ago recommended cuts to the enrolment in Canadian medical schools. They are accordingly held responsible, at least by prominent voices in Canada's medical community, for a severe shortage of physicians that persists to this day:
Having your names associated with a report that has been universally blamed for leading health ministers to cut medical school enrolment by 10% is no way to make friends in the medical profession … [I]n terms of health economists who are reviled by Canadian physicians, Barer and Stoddart probably place second to the great Satan1 himself, Robert Evans.”
But Time has moved on, and his daughter now has more to say about the shortage of physicians, and the role of the villainous Barer and Stoddart. In retrospect, the conventional dramatization is a combination of myth and muddle. The myth is that Barer and Stoddart simply recommended enrolment cuts; the muddle is a confusion between medical school enrolment and the stock of physicians, and between the physician stock and the supply of physicians' services. (The relationship between any of these, and population health, never entered the debate.)
Barer and Stoddart summarized their 355-page report in a series of 12 papers in the Canadian Medical Association Journal during 1992 and 1993. Had they done no more than recommend a reduction in enrolments, they might have been more succinct. They may have hoped that a comprehensive and accessible presentation would prevent the generation of myths and misinformation. It didn't.
Their report was, as requested by the Federal/Provincial/Territorial Conference of Deputy Ministers of Health, a review of issues and policy options for assuring an adequate and appropriate supply of medical services for Canadians. These go far beyond counting physicians. The authors made 53 recommendations, in an integrated package, and emphasized that “cherry-picking” from this package could easily do more harm that good. Provincial governments promptly (and predictably) cherry-picked the easiest, in hopes of saving money.
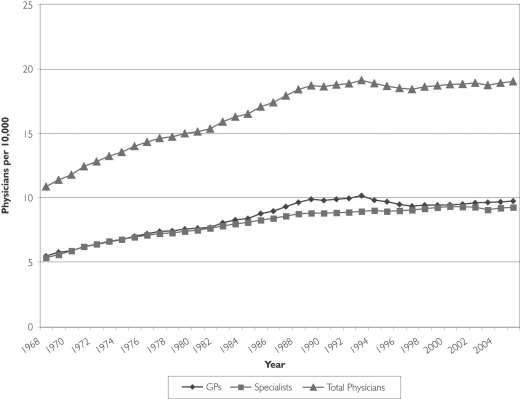
The result? Figure 1 plots the Canadian physician-to-population ratios – generalists, specialists and total – from 1968 to 2005 (CIHI 2007b). The main messages of Figure 1 are twofold. First, there was a major change in the dynamics of physician supply at the end of the 1980s, wholly unrelated to Barer–Stoddart or to subsequent enrolment cuts. And second, despite that shift, the supply of physicians has not been falling. The number of physicians per 10,000 population has been remarkably stable, with minor fluctuations, over the last two decades. The 2005 level of 19.0 was 1.6% above the 1991 level of 18.7.
FIGURE 1.
Canada, physicians per 10,000 population, 1968–2005
Yet, reports that people cannot find a family physician, and face unacceptable waits for specialist care, persist despite what is in fact a growing supply. As Chan (2002) put it, “Why does it feel like we have a physician shortage?” If it is true that an increasingly severe shortage has been developing since the mid-1990s, it must be a shortage of physicians' services, not of physicians per se, perhaps reflecting declining average clinical workload per physician.2 We address this issue below, noting here only that medical school enrolments have no direct effect on average physician workloads.
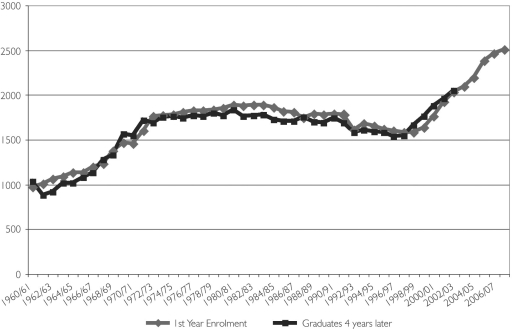
Enrolments certainly fell after 1991 – and before. Figure 2 plots first-year enrolments by academic year along with calendar-year graduations four years later (ACMC 2007). First-year enrolments fell by 5.9% from their 1983/84 peak of 1,887 to 1,775 in 1991/92, and by a further 11.1% to 1,577 by 1997/98. Numbers of graduates correspondingly began to fall in 1987/88 and troughed in 2000/01 and 2001/02.
FIGURE 2.
Canadian medical schools, 1960/61–2007/08
Graduation, however, does not mean entry to practice. There is a further residency period of two years for family practitioners (one year, prior to 1993) and significantly longer for specialists. Changes in first-year enrolment only begin to show up in the practitioner stock six years later, and may take eight to 10 years to have their full effect on practice entry. And since the currently practising stock is so much larger than the annual increment, changes in the annual numbers entering practice might not be noticeable for at least another decade.
Changes in training requirements that affect an entire cohort of students do show up in Figures 1 and 2. Eliminating the rotating internship in 1993, thus lengthening the family practice residency to two years, in effect delayed the entry to practice of an entire cohort by one year, and the effect shows up in Figure 1. Likewise, the shortening of undergraduate training at the University of Montreal eliminated an entire entering class and produced the drop in Figure 2 in 1992.
Media reports of physician shortages in the mid- and late 1990s are thus far too early to reflect the effects on the ground of recommendations made or actions taken in the early 1990s. The cuts made in the 1980s could conceivably be affecting the supply of physicians by now – but as Figure 1 shows, the doctor-to-population ratio still resolutely refuses to fall. So where's the shortage?
One obvious possibility is that physicians are, on average, providing less care than formerly. Medicine has become increasingly feminized, and females put in, on average, less time in practice over the year or the career. Moreover, and perhaps more significantly, the young physicians of today have different career expectations than their predecessors did. Physicians still work more hours than the average member of the labour force, but the younger generation do not, on average, match their elders.
Watson et al. (2006) and Crossley et al. (2006) both report declines in self-reported average weekly hours of direct patient care by GPs/FPs from national CMA surveys. Watson et al. find a decline of 8.5% between 1993 and 2003; Crossley et al. find a decline of 15.6% between 1982 and 2003. Preliminary data for British Columbia show declining annual (full-time) days worked for both GPs and specialists between 1994 and 2004. These results are consistent with a shortage emerging, not from a declining physician supply, but from declining labour input by physicians.
The findings also suggest a possible explanation for the emergence of “shortage” concerns in the 1990s. GPs/FPs per capita rose 22.5% between 1982 and 1989, considerably more than the decline in average hours of work found by Crossley et al. for the whole period 1982 to 2003. When the doctor-to-population ratio stabilized, the continuing decline in hours of work led to perceptions of a shortage. But it was, and is, a decline in physician work effort, not in physician numbers – and therefore wholly unrelated to enrolment cuts.
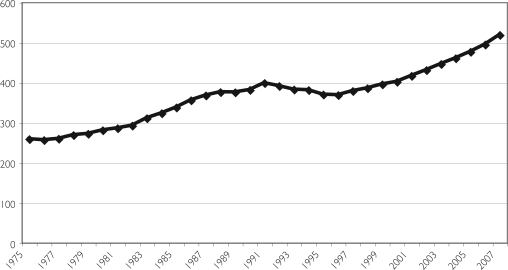
But if physicians are putting in less time, should not their average billings be falling? Figure 3 shows the trend in (inflation-adjusted) per capita expenditures on physicians' services between 1975 and 2007 (forecast, CIHI 2007a). This measure of service volume per capita increased by 30% between 1991 and 2007. While markedly less rapid than the 54% increase from 1975 to 1991, this is still a respectable increase for a time when the physician-to-population ratio was stable and physician hours of work were falling. How are these figures reconciled with a general perception of shortage?3
FIGURE 3.
Canada, physician expenditures per capita, inflation-adjusted, 1975–2007
Watson et al. (2004) suggest a possible explanation. Studying GPs in Winnipeg, they found declines between 1993 and 2003 in average service volumes provided by successive cohorts of younger physicians, but increases among older physicians. As physicians and their patients age together, the servicing per patient increases. But older physicians may be less willing to take on new patients, and younger physicians are carrying smaller patient loads. Thus new patients cannot find a practice to accept them, even though average billing (expenditure) rates are not falling. This bifurcation in workloads would suggest that, when the older physician cohorts retire, average workloads may drop significantly.
The hours-of-work studies focus only on GPs/FPs; Figure 3 reports total expenditures on both GPs/FPs and specialists' services. The ratio of generalists to specialists has remained surprisingly constant over time; the data underlying Figure 1 show a ratio of 49.4% specialists in 1968 and 48.7% in 2005. But billings per specialist are both greater and increasing more rapidly. Barer et al. (2004) found that in British Columbia, expenditures per capita on GP/FP services (age-adjusted) rose only 3.3% between 1985/86 and 1996/97, while those for all specialists rose 15.7%. Expenditures for medical specialists rose 31.8%. “GP/FPs appeared to focus increasingly on less time-consuming (younger) patients, referring more complex (older) patients for specialty attention after initial contact” (Barer et al. (2004). Insofar as workload is being shifted from generalists to specialists, a focus on GPs/FPs alone may significantly underestimate trends in available primary care capacity.
Like the fate of the little princes, there remains an air of mystery surrounding the Canadian physician shortage. The stabilization of the doctor-to-population ratio at the end of the 1980s suggests that population growth had finally caught up with the dramatic increase in first-year enrolments (81.8%) between 1960/61 and 1972/73. The previously rapid climb in (inflation-adjusted) expenditures per capita correspondingly slowed, and even fell back slightly, before beginning a new, rapid acceleration after 1996.
This recent surge implies an extraordinary growth in billings (and alternative payments) per physician – Figure 3 divided by Figure 1. Apparent “output” per physician grew by 22% between 1990 and 2005, twice the 11% rate from 1975 to 1990. Yet, physicians report putting in fewer hours, and there is a widespread perception of shortage. Obviously, specialists must be factored into the mix, but if all physicians are working less and billing so much more, how do we interpret this discrepancy? What are they doing, why and with what consequences?
To call this trend increased “productivity” is to assume that increased billings correspond to increased provision of needed, effective services.4 But if this “real output” per doctor – effective care – has been increasing by over 2.5% per year since 1996, why are there complaints of shortages, and why do we need more doctors? Conversely, if the surge in expenditures is a result of average fee increases outrunning inflation (see note 4), or more creative billing practices, then Canadians are simply paying more for less.
This point is critical in light of the right-hand side of Figure 2. The physician shortage, real or rhetorical, has had its political effect. In the decade from 1997/98 to 2007/08, first-year medical school enrolment has risen by 58.9%, from 1,577 to 2,506. This growth is remarkably similar to that from 1962/63 to 1972/73. Graduations are following with a four-year lag, and if there is no further expansion, should top out at about 2,500 in 2011.
The impact on practitioner numbers, starting in 2004/05, is almost imperceptible now but will build steadily for the next 20 years, placing steadily increasing pressure on medicare budgets. If per capita billings per physician also continue to grow at the rates observed after 1996, that pressure will be doubled.
There is serious fiscal trouble on the horizon if these new practitioners expect earnings similar to their predecessors'. Will we be willing to continue paying physicians more to work less, as their numbers swell? If they also each expect similar levels of practice support – hospitals, medical equipment and drugs – the cost pressures will be multiplied further. But if not?
One thing is crystal clear. Neither the alleged shortage nor the dramatic overreaction can be laid at the feet of Barer and Stoddart. This leaves one more little mystery. We may understand why Shakespeare demonized Richard – good politics and great theatre. But why, given the obvious disconnect between their report and the subsequently alleged physician shortage, did Barer and Stoddart become the whipping boys for that shortage? Force of habit, perhaps. But when otherwise-intelligent people say or do silly things, there is usually a deeper reason.
The hostility of the professional leadership based in medical schools is not hard to understand – reduced enrolments, reduced budgets, more limited research and career opportunities. But why would the rest of the profession support expansion? Consider what happened after the previous great surge.
The early 1970s were a time of great hopes for change in healthcare. Following the implementation of universal coverage, the next step would focus on how medical work was organized and paid for – Tommy Douglas's “second phase.” John Hastings's (1970) report on community health centres and Thomas Boudreau's (1972) report on the nurse practitioner as substitute for general practitioners in primary care both drew on extensive and incontrovertible research on better, and more efficient, alternatives to traditional, independent, fee-for-service practice.
All these hopes were washed away in the flood of new doctors. Provincial governments, hip-deep in physicians, had little energy or money left to focus on draining the medical swamp. They were too busy trying to cope with the cost implications of a 71.6% increase in physicians per capita between 1968 and 1989. Over those years, the share of GDP absorbed by physicians rose over 30%.
The stabilization of physician supply at the beginning of the 1990s opened a new opportunity to consider more diverse ways of providing medical care, and a number of these alternatives were considered in the Barer–Stoddart report. But they were kept off the public agenda by the exclusive focus on physician numbers and enrolments, and the report as a whole was discredited by the claim that it had caused a shortage. (“Don't listen to those guys!”) Nothing is wrong with the status quo; we just need more of the same – and more money to pay them. The coming new flood of physicians is likely to wash away Douglas's second phase for another 20 years.
The earlier surge was a pure policy accident. Justice Emmett Hall's recommendations, in 1964, for a major expansion in training places were made on the assumption that the post-war baby boom would continue. The ink on his report was barely dry when the Great Obstetrical Contraction of 1964–1966 cut the birth rate by nearly 20%. Hall's population projections for 1991 were too high by 25%, but the medical school capacity built to meet those projections, like the Sorcerer's Apprentice, kept grinding out more physicians. By the late 1980s, headlines like “Doctor Glut Costs Millions” were becoming commonplace.
But it is striking – and this is a critical point – that service use, or at least billings, kept pace with the growing supply. There was no sign of saturation. This situation might have raised questions as to the appropriateness of the extra services being provided. How were the additional physicians keeping themselves (gainfully) employed? Were they meeting previously unmet needs, or providing unnecessary services? Was anyone's health improved?
Any suggestion that physicians, while fully employed, are in oversupply thus raises potentially embarrassing questions. The view acceptable to the profession is that if services are being provided by well-trained physicians, then they must, by definition, be needed – res ipse loquitur – no matter how large the supply. If more doctors correlate with more servicing – and increased expenditures – so be it. Patients are benefiting. To suggest otherwise would be outrageous.5
Barer and Stoddart provided a convenient lightning rod for discharging this sense of outrage. The fact that, whether or not there was or is a physician shortage, their report did not and could not have had anything to do with it, was irrelevant.
As for Richard, his Tudor successors ruled England from 1485 to 1603, and Richard III is one of Shakespeare's most popular plays.
And we in Canada are now beginning the same physician supply cycle again, 40 years on.
“Great Satan” is the term used by the Iranian ayatollahs to describe the United States, but the editor of the Medical Post surely did not intend to draw a parallel between Canada's physicians and Iran's ayatollahs.
Reports of shortages may also reflect distributional problems, or shortages in particular regions or specialties, misperceived as a general shortage.
A knee-jerk explanation, population aging, is (as always) too feeble an effect. The connection between age and physician use is much weaker than that for hospital or other institutional care. Aging per se would increase use by 0.3% to 0.5% per year, or 5% to 8% over 16 years. A more serious bias in Figure 3 is the deflation of physician expenditures by an index based on general price levels. National fee indexes are, unfortunately, no longer compiled. The measure of service volumes is thus downward- (upward-) biased over any period in which physicians' fees were rising less (more) rapidly than prices generally. A related problem arises from the expansion of alternative payment programs (APPs). Insofar as these, as in British Columbia, primarily cover on-call time or increased rural/isolation allowances rather than payments for increased services, they represent increases in prices, not quantities, but are not included in the deflator used in Figure 3.
Increased output of unnecessary or harmful services is counted as productivity in some of the more severely lobotomized reaches of economic analysis, but serious people do not take such measures seriously.
Dentists, by contrast, seem quite untroubled by reduced training capacity, and thereby hangs a tale.
Contributor Information
Robert G. Evans, Professor of Economics, University of British Columbia, Vancouver, BC
Kimberlyn M. McGrail, Centre for Health Services and Policy Research, University of British Columbia, Vancouver, BC.
References
- Association of Canadian Medical Colleges (ACMC) Canadian Medical Education Statistics, 2007. Volume 29. Ottawa: Author; 2007. [Google Scholar]
- Barer M.L., Evans R.G., McGrail K.M., Green B., Hertzman C., Sheps S.B. Beneath the Calm Surface …: The Changing Face of Physician Service Use in British Columbia, 1985/86–1996/97. Canadian Medical Association Journal. 2004 Mar 2;170(5):803–7. doi: 10.1503/cmaj.1020460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barer M.L., Stoddart G.L. Toward Integrated Medical Resource Policies for Canada: Background Document. Vancouver: Centre for Health Services and Policy Research, University of British Columbia; 1991. HPRU 91:06D. Retrieved January 27, 2008. < http://www.chspr.ubc.ca/files/publications/1991/hpru91-06D.pdf>. [Google Scholar]
- Boudreau T.J. Report of the Committee on Nurse Practitioners. Ottawa: Department of National Health and Welfare; 1972. [Google Scholar]
- Canadian Institute for Health Information (CIHI) National Health Expenditure Trends, 1975–2007. Ottawa: Author; 2007a. [Google Scholar]
- Canadian Institute for Health Information (CIHI) Scott's Medical Database. 2007b Retrieved January 27, 2008. < http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=hhrdata_smdb_e>.
- Chan B. From Perceived Surplus to Perceived Shortage: What Happened to Canada's Physician Workforce in the 1990s? Ottawa: Canadian Institute for Health Information; 2002. [Google Scholar]
- Crossley T.F., Hurley J., Jeon S.-H. Physician Labour Supply in Canada: A Cohort Analysis. Hamilton, ON: McMaster University; 2006. Sep 12, SEDAP Research Paper No. 162. Retrieved January 27, 2008. < http://socserv.mcmaster.ca/sedap/p/sedap162.pdf>. [DOI] [PubMed] [Google Scholar]
- Hall E. Report of the Royal Commission on Health Services. Ottawa: Queen's Printer; 1964. [Google Scholar]
- Hastings J.E.T. The Community Health Centre in Canada: Report of the Community Health Centre Project to the Conference of Health Ministers. Ottawa: Department of National Health and Welfare; 1970. [Google Scholar]
- Politicians can't live up to Barer-Stoddart ideals. The Medical Post. 1999. Sep 28, p. 12. Editorial.
- Watson D.E., Katz A., Reid R.J., Bogdanovic B., Roos N., Heppner P. Family Physician Workloads and Access to Care in Winnipeg: 1991 to 2001. Canadian Medical Association Journal. 2004 Aug 17;171(4):339–42. doi: 10.1503/cmaj.1031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., Slade S., Buske L., Tepper J. Intergenerational Differences in Workloads among Primary Care Physicians: A Ten-Year, Population-Based Study. Health Affairs. 2006;25(6):1620–28. doi: 10.1377/hlthaff.25.6.1620. [DOI] [PubMed] [Google Scholar]