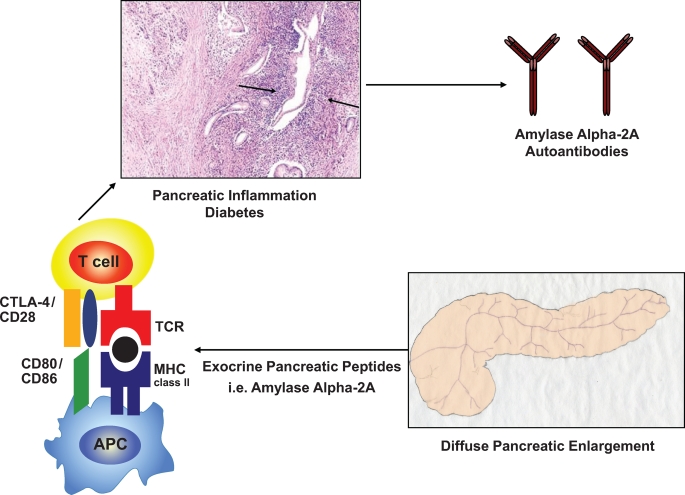
FIG. 1.
Hypothetical mechanisms causing autoimmune pancreatitis. Although the pathogenesis of AIP and fulminant type 1 diabetes remains to be elucidated, AIP, similar to other autoimmune diseases, is associated with polymorphisms within the HLA complex. In the Japanese population, the highest risk for autoimmune pancreatitis is conferred by the HLA DRB1*0405-DQB1*0401 haplotype (ref. 11). Each allele is simply given a number that represents a unique amino acid sequence, and each sequence binds only certain peptides, which could be amylase α-2A peptides. Antigen-presenting cells (APC) present these peptides to lymphocytes and provide signals that stimulate the proliferation and differentiation of lymphocytes, generally T-lymphocytes. Interestingly, regulatory T-cell–deficient NOD CD28KO mice develop spontaneous AIP, which in this model is not a consequence of preexisting β-cell autoimmunity (ref. 13). This mechanism could also play a role in the pathogenesis of AIP in humans. The histologic pattern of AIP in humans includes a periductal collar of lymphoplasmacytic inflammation (arrows, hematoxylin and eosin image reprinted with permission from Finkelbert et al. [ref. 16]). MHC, major histocompatibility complex; TCR, T-cell receptor. (Please see http://dx.doi.org/10.2337/db08-1655 for a high-quality digital representation of this figure.)