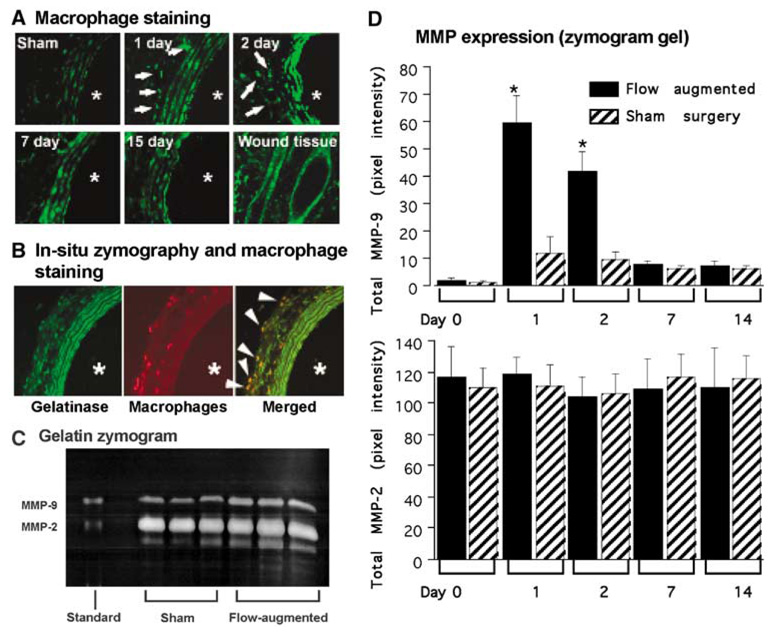
Figure 3.
MMP expression in the remodeling common carotid artery. (A) In situ zymography (gelatin) in flow-augmented right common carotid artery (× 20). The remodeling carotid artery showed abundant gelatinase activity between elastic laminae and scattered gelatinase activity in the adventitia (white arrows). Among the time points we studied, gelatinase activity was most prominent at day 2. Sham surgery group showed gelatinase activity only between elastic laminae, probably reflecting constitutive expression of MMP-2 by smooth muscle cells as previously described. (B) In situ zymography and immunofluorescence staining for macrophages in flow-augmented right common carotid artery at day 3 (× 20). Wound tissue was used as a positive control. *Indicates the lumen. Gelatinase activity was between elastic laminae and in the adventitia (left panel, green). Macrophages were seen mostly in the adventitia (middle panel, red). Macrophages were colocalized with gelatinase activity in the adventitia (right panel, yellow). White arrows indicate colocalization of gelatinase activity with macrophages. (C) Gelatin zymogram gel using flow-augmented right common carotid artery at day 2. Flow-augmented right common carotid arteries had higher levels of MMP-2 and MMP-9 at day 2 than those from sham surgery. Although pro-MMP-9, pro-MMP-2, and active MMP-2 bands were prominent, active MMP-9 bands were very faint. (D) Time course of MMP-9 and MMP-2 expression in flow-augmented right common carotid artery. In the flow-augmented right common carotid artery, upregulation of total MMP-9 was detected as early as day 1, after which MMP-9 levels gradually returned to baseline. In sham surgery group, there was a slight increase in MMP-9 at day 1, probably reflecting systemic inflammation caused by the sham surgery. The time course of MMP-9 expression coincided with infiltration of macrophages. MMP-2 was expressed in both sham and flow-augmented right common carotid artery at all time points that we studied. There was no difference in MMP-2 levels between sham and flow-augmented right common carotid arteries at any time point. Moreover, there was no significant temporal change of MMP-2 levels in flow-augmented common carotid artery. (Mean±s.d.; *P<0.05, compared with the baseline.)