Abstract
Ten isolates of the recently delineated genospecies Borrelia spielmanii were tested against antimicrobial agents used to treat Lyme disease and compared to eight isolates of the other three human-pathogenic borrelial genospecies. Despite some small but significant differences in four out of eight antibiotic agents, the susceptibility pattern of B. spielmanii mainly parallels that of the other known human-pathogenic members of the B. burgdorferi sensu lato complex.
Lyme disease is a multisystem tick-borne disorder with dermatologic, neurologic, and rheumatologic manifestations (3, 26, 29). The disease represents the most common vector-borne illness in the Northern Hemisphere and is caused by human-pathogenic members of the Borrelia burgdorferi sensu lato complex, including B. burgdorferi sensu stricto, B. garinii, B. afzelii, and the very recently established species B. spielmanii (22, 28). Isolates belonging to the newly delineated genospecies B. spielmanii have hitherto been isolated from patients in The Netherlands, Hungary, Slovenia, and Germany as well as from ticks in France, Germany, Ukraine, and the Czech Republic (6-8, 18, 19, 23, 25, 28). The heterogeneity of borrelial strains is known to impact the variability of Lyme disease manifestations and clearly is a challenge for the development of diagnostic tests and vaccines (7). Moreover, minor differences in the antimicrobial susceptibility patterns of the classical borrelial genospecies known to be pathogenic for humans have been observed (12, 15, 17, 24). For the newly recognized species B. spielmanii, our current knowledge of clinical disease manifestations, susceptibility to antimicrobials, and optimum treatment regimens is limited due to the low number of clinical cases and few isolates available. As such, a better understanding of the antimicrobial susceptibility of this newly recognized borrelial genospecies is integral for proposing treatment (7, 11).
We investigated under standardized conditions the antibiotic susceptibility patterns of 10 B. spielmanii isolates to eight antimicrobial agents known to be relevant for the treatment of Lyme disease. For methodological and control purposes, eight isolates belonging to the other three human-pathogenic Borrelia species served as a comparison group. The clinical and geographic origins of all isolates used in this study are listed in a footnote to Table 1. For genospecies identification, all isolates were subjected to sequencing of the rrfA-rrlB spacer region in combination with plasmid profile analysis, as previously described (1, 20, 30). Except for B. burgdorferi sensu stricto reference strain B31 (ATCC 35210), low-passage isolates (10 to 20 passages) were tested using microtiter trays carrying lyophilized antimicrobial agents (Merlin-Diagnostika GmbH, Bornheim-Hersel, Germany) (12, 17). The substances tested included β-lactams, tetracyclines, and macrolides, all agents frequently used in the treatment of Lyme disease (29). Moreover, the class I and II fluoroquinolones ciprofloxacin and levofloxacin were also analyzed and served as control substances with known low activities against B. burgdorferi sensu lato (17). MICs were determined after 72 h by use of a colorimetric assay, as recently described in more detail (12, 17). Minimal borreliacidal concentrations (MBCs) were determined under stringent conditions (100% killing in liquid medium) after 72 h. Aliquots (18 μl) from all vials without detectable growth were diluted (1:1,000) below the MIC in Barbour-Stoenner-Kelly medium (BSK) and inspected for regrowth after 3 weeks of subculture (12, 13). For each isolate and substance, independent experiments were performed on different days, with MICs and MBCs reported as the medians from three experiments. For additional quality control and to investigate possible antibiotic-medium interactions, MICs for Staphylococcus aureus reference strain ATCC 29213 were determined following CLSI guidelines, except for a 48-h preincubation of the antibiotic-BSK preparation (5). In addition, exemplary time-kill studies were performed with B. spielmanii strain PC-Eq17 exposed to ceftriaxone for 120 h, as described elsewhere (15, 17, 21). To identify possible differences in MIC and MBC data between B. spielmanii and the other human-pathogenic genospecies, the Kruskal-Wallis test was applied using BIAS, version 8.3.8 (Epsilon Verlag, Hochheim, Germany) (15).
TABLE 1.
Antibiotic susceptibilities of 18 B. burgdorferi sensu lato isolates to β-lactams, macrolides, and doxycycline, as determined in BSKa
| Isolated or parameter | Concn (μg/ml) of antimicrobial agentb
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Doxycycline
|
Erythromycin
|
Clarithromycin
|
Amoxicillin
|
Cefuroxime
|
Ceftriaxone
|
|||||||
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| B. spielmanii | ||||||||||||
| PMew | 0.5 | 16 | 0.0312 | 2 | 0.0079 | 1 | 1 | >16 | 0.125 | >8 | 0.125 | 4 |
| PSigII | 0.125 | 8 | 0.0079 | 2 | 0.0019 | 1 | 0.5 | 16 | 0.125 | 8 | 0.0312 | 1 |
| PC-Eq17 | 0.125 | 16 | 0.0156 | 4 | 0.0019 | 1 | 0.5 | >16 | 0.125 | >8 | 0.0312 | 2 |
| PHap | 0.0625 | 16 | 0.0079 | 2 | 0.0019 | 0.5 | 2 | >16 | 0.25 | >8 | 0.0625 | 2 |
| PJes | 0.125 | 8 | 0.0156 | 1 | 0.0039 | 0.5 | 0.25 | 16 | 0.125 | 8 | 0.0312 | 2 |
| PAnz | 0.0625 | 8 | 0.0079 | 2 | 0.0019 | 1 | 0.25 | 16 | 0.125 | >8 | 0.0156 | 1 |
| PMai | 0.125 | 8 | 0.0079 | 1 | 0.0019 | 0.5 | 2 | 8 | 0.125 | 8 | 0.0625 | 4 |
| A14S | 0.125 | 16 | 0.0156 | 2 | 0.0039 | 1 | 0.25 | 16 | 0.125 | 8 | 0.0312 | 0.5 |
| TIsar2 | 0.25 | 16 | 0.0312 | 1 | 0.0079 | 0.5 | ≤0.125 | 16 | 0.125 | 2 | 0.0156 | 0.5 |
| TIsar3 | 0.125 | 8 | 0.0312 | 2 | 0.0079 | 1 | 2 | 4 | 0.5 | 4 | 0.0625 | 0.5 |
| B. burgdorferi sensu stricto | ||||||||||||
| B31 | 0.25 | 16 | 0.0312 | 4 | 0.0079 | 2 | 0.5 | 16 | 0.125 | >8 | 0.0312 | 2 |
| LW2 | 0.125 | 32 | 0.0312 | 4 | 0.0039 | 4 | 1 | 4 | 0.125 | 8 | 0.0312 | 4 |
| B. afzelii | ||||||||||||
| FEM1 | 0.125 | 4 | 0.0312 | 2 | 0.0039 | 1 | 4 | 4 | 0.5 | >8 | 0.0625 | 2 |
| G600 | 0.25 | 2 | 0.0312 | 2 | 0.0079 | 0.5 | 1 | 4 | 0.25 | 4 | 0.0625 | 0.5 |
| G1039 | 0.125 | 4 | 0.0156 | 2 | 0.0039 | 1 | 0.5 | 8 | 0.125 | 8 | 0.0312 | 0.5 |
| B. garinii | ||||||||||||
| PSth | 0.25 | 32 | 0.0312 | 4 | 0.0079 | 2 | 0.125 | 8 | 0.125 | >8 | 0.0312 | 2 |
| M2094 | 0.25 | 16 | 0.0312 | 4 | 0.0039 | 1 | 0.25 | 16 | 0.125 | >8 | 0.0312 | 2 |
| G1 | 0.125 | 16 | 0.0156 | 4 | 0.0019 | 1 | ≤0.125 | 16 | 0.125 | >8 | 0.0312 | 2 |
| All Borrelia isolates | ||||||||||||
| MIC or MBC range | 0.0625-0.5 | 2-32 | 0.0079-0.0625 | 1->4 | 0.001-0.0156 | 0.25-4 | ≤0.125-4 | 2->16 | ≤0.063-0.25 | 1->8 | 0.0156-0.125 | 0.25-4 |
| MIC90 or MBC90c | 0.25 | 16 | 0.0312 | 4 | 0.0079 | 1 | 2 | >16 | 0.25 | >8 | 0.0625 | 4 |
| S. aureus ATCC 29213e | ||||||||||||
| Median MIC | 0.25 | 0.25 | 0.063 | 2 | 2 | 4 | ||||||
| CLSI MIC range | 0.12-0.5 | 0.25-1 | 0.12-0.5 | 0.12-0.5 | 0.5-2 | 1-8 | ||||||
Antimicrobial susceptibility was determined on three different days, and MICs and MBCs for each isolate are reported as the medians from three experiments.
The test ranges (in μg/ml) were as follows: for doxycycline, 0.016 to 32; for erythromycin and clarithromycin, 0.0002 to 4; for amoxicillin, 0.125 to 16; for ceftriaxone, 0.004 to 8; and for cefuroxime, 0.063 to 8.
MBC90, MBC required to kill 90% of the isolates.
Geographic and clinical characteristics of the strains are as follows: isolates PMew, PSigII, PHap, PMai, PSth, LW2, and FEM1 were recovered from skin samples in Germany; isolate PC-Eq17 was recovered from a tick in France; isolates PAnz, PJes, G600, G1039, and M2094 were recovered from skin samples in Slovenia; isolate A14S was recovered from a skin sample in The Netherlands; isolates TIsar2 and TIsar3 were recovered from ticks in Germany; isolate G1 was recovered from cerebrospinal fluid in Germany; and isolate B31 was recovered from a tick in the United States.
To investigate significant antibiotic-medium interaction, MICs for S. aureus (ATCC 29213) were determined on three different days, referring to the CLSI method (5), except for the use of BSK and preincubation of the antibiotic-medium test preparation for 48 h before testing. Results are reported as the medians from all three experiments.
MICs and MBCs of each antimicrobial agent for the same isolate spanned a maximum range of ±1 log2 unit dilution around the median. Test results for the borrelial reference strains corresponded well to the MICs and MBCs obtained in previous studies under comparable experimental conditions (9, 12-15, 17, 24). As expected, the fluoroquinolones ciprofloxacin (MIC90, >4 μg/ml) and levofloxacin (MIC90, >4 μg/ml) were largely ineffective against all 18 borrelial strains tested. The in vitro activities of the other antimicrobial agents are summarized in Table 1. On a microgram-per-milliliter basis, the rank order of substances with substantial in vitro activity against the borrelial isolates tested was clarithromycin (MIC90, 0.0079 μg/ml) > erythromycin (MIC90, 0.0312 μg/ml) > ceftriaxone (MIC90, 0.0625 μg/ml) > doxycycline and cefuroxime (MIC90, 0.25 μg/ml) > amoxicillin (MIC90, 2 μg/ml).
Quality control experiments with S. aureus ATCC 29213 indicated a loss of activity for amoxicillin and a slightly better performance of clarithromycin due to incubation in BSK. MICs for all other substances were in the ranges published by CLSI (Table 1). Observations of similar side effects of BSK on penicillin and macrolides became obvious also in previous studies of this topic (11, 15).
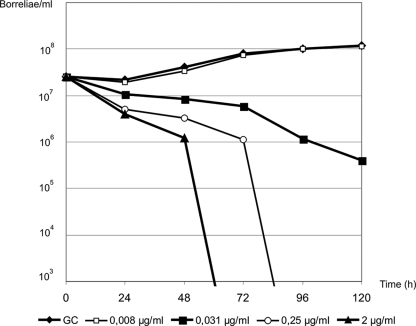
Exemplary time-kill experiments further substantiated the in vitro effectiveness of ceftriaxone against B. spielmanii and the consistency of MICs and MBCs obtained with our standardized colorimetric assay followed by conventional subculture (12, 13, 17). As shown in Fig. 1, exposure to ceftriaxone inhibited the growth of B. spielmanii isolate PC-Eq17 at a MIC of 0.0312 μg/ml and led to a 3 log10 unit (99.9%) reduction of morphologically intact motile cells at a concentration of 2 μg/ml in less than 72 h. Upon statistical analysis of all measured MICs and MBCs (n = 864) obtained throughout our experiments, some small but significant differences between B. spielmanii and the reference strains became obvious in regard to in vitro susceptibilities to amoxicillin, doxycycline, erythromycin, and clarithromycin. Compared to activities against the B. burgdorferi sensu stricto, B. afzelii, and B. garinii strains, the macrolides showed high in vitro activity against the B. spielmanii isolates tested, as demonstrated by significantly lower MICs and MBCs (P < 0.05). Similarly, the MICs of doxycycline were significantly lower (P < 0.05) for B. spielmanii strains whereas the MBCs of amoxicillin were higher than those for the other genospecies tested (P < 0.05). Our study presents the first investigation detailing the activities of antimicrobial agents against B. spielmanii. Here, we demonstrate that the antibiotic susceptibility pattern of this new genospecies is in principal comparable to those of the other known borrelial genospecies with pathogenic potential for humans when tested under similar experimental conditions (9, 12-15, 17, 24). The notion of minor interstrain variability within the species B. spielmanii as well as intergenospecies-specific variations for several antibiotic substances parallels observations of minor differences in the antimicrobial susceptibility patterns within the B. burgdorferi sensu lato complex as described in previous studies (11, 12, 24). So far, B. spielmanii has been isolated only from patients with skin manifestation of Lyme disease (7, 8, 22, 23, 28). However, based upon our findings, the detected differences in the in vitro susceptibility patterns, although significant, appear too small to be of general medical relevance in the treatment of Lyme disease. Instead, antimicrobial agents commonly used for the treatment of Lyme disease are expected to be clinically effective in patients infected with B. spielmanii. It should be considered, however, that although an acquired resistance to antimicrobial agents in borreliae can be detected by use of susceptibility assays (4, 16), in vitro testing alone cannot reliably exclude phenotypic mechanisms of persistence displayed in vivo, as revealed in recent experimental investigations with laboratory animals (2, 10) and clinical studies of patients with Lyme disease (14, 27).
FIG. 1.
Time-kill curves for B. spielmanii isolate PC-Eq17 with ceftriaxone. Lines in boldface indicate borrelial growth of the growth control (GC), inoculum reduction at the MIC (0.031 μg/ml), and killing of the inoculum at the MBC (2 μg/ml) over 120 h of incubation. For reasons of comparison, lines not in boldface show borrelial growth at a ceftriaxone concentration of the MIC (0.008 μg/ml) and decelerated killing of the inoculum at a concentration of 3 log10 units below the MBC (0.25 μg/ml). Experiments were performed on different days by investigation of growth using conventional cell counts, and data are reported as the means from two independent experiments.
Acknowledgments
We thank V. Fingerle, A. van Dam, and E. Ružić-Sabljić for kindly providing some of the tested isolates.
Footnotes
Published ahead of print on 15 December 2008.
REFERENCES
- 1.Barbour, A. G. 1988. Plasmid analysis of Borrelia burgdorferi, the Lyme disease agent. J. Clin. Microbiol. 26:475-478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bockenstedt, L. K., J. Mao, E. Hodzic, S. W. Barthold, and D. Fish. 2002. Detection of attenuated, noninfectious spirochetes in Borrelia burgdorferi-infected mice after antibiotic treatment. J. Infect. Dis. 186:1430-1437. [DOI] [PubMed] [Google Scholar]
- 3.Brouqui, P., F. Bacellar, G. Baranton, R. J. Birtles, A. Bjoersdorff, J. R. Blanco, G. Caruso, M. Cinco, P. E. Fournier, E. Francavilla, M. Jensenius, J. Kazar, H. Laferl, A. Lakos, S. Lotric Furlan, M. Maurin, J. A. Oteo, P. Parola, C. Perez-Eid, O. Peter, D. Postic, D. Raoult, A. Tellez, Y. Tselentis, and B. Wilske. 2004. Guidelines for the diagnosis of tick-borne bacterial diseases in Europe. Clin. Microbiol. Infect. 10:1108-1132. [DOI] [PubMed] [Google Scholar]
- 4.Bunikis, I., K. Denker, Y. Ostberg, C. Andersen, R. Benz, and S. Bergstrom. 2008. An RND-type efflux system in Borrelia burgdorferi is involved in virulence and resistance to antimicrobial compounds. PLoS Pathog. 4:e1000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CLSI. 2006. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A7, 7th ed. CLSI, Wayne, PA.
- 6.Derdáková, M., L. Beati, B. Pet'ko, M. Stanko, and D. Fish. 2003. Genetic variability within Borrelia burgdorferi sensu lato genospecies established by PCR-single-strand conformation polymorphism analysis of the rrfA-rrlB intergenic spacer in Ixodes ricinus ticks from the Czech Republic. Appl. Environ. Microbiol. 69:509-516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fingerle, V., U. C. Schulte-Spechtel, E. Ruzic-Sabljic, S. Leonhard, H. Hofmann, K. Weber, K. Pfister, F. Strle, and B. Wilske. 2008. Epidemiological aspects and molecular characterization of Borrelia burgdorferi s.l. from southern Germany with special respect to the new species Borrelia spielmanii sp. nov. Int. J. Med. Microbiol. 298:279-290. [DOI] [PubMed] [Google Scholar]
- 8.Földvári, G., R. Farkas, and A. Lakos. 2005. Borrelia spielmanii erythema migrans, Hungary. Emerg. Infect. Dis. 11:1794-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henneberg, J. P., and U. Neubert. 2002. Borrelia burgdorferi group: in-vitro antibiotic sensitivity. Orv. Hetil. 143:1195-1198. (In Hungarian.) [PubMed] [Google Scholar]
- 10.Hodzic, E., S. Feng, K. Holden, K. J. Freet, and S. W. Barthold. 2008. Persistence of Borrelia burgdorferi following antibiotic treatment in mice. Antimicrob. Agents Chemother. 52:1728-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hunfeld, K. P., and V. Brade. 2006. Antimicrobial susceptibility of Borrelia burgdorferi sensu lato: what we know, what we don't know, and what we need to know. Wien. Klin. Wochenschr. 118:659-668. [DOI] [PubMed] [Google Scholar]
- 12.Hunfeld, K. P., P. Kraiczy, T. A. Wichelhaus, V. Schafer, and V. Brade. 2000. Colorimetric in vitro susceptibility testing of penicillins, cephalosporins, macrolides, streptogramins, tetracyclines, and aminoglycosides against Borrelia burgdorferi isolates. Int. J. Antimicrob. Agents 15:11-17. [DOI] [PubMed] [Google Scholar]
- 13.Hunfeld, K. P., R. Rodel, and T. A. Wichelhaus. 2003. In vitro activity of eight oral cephalosporins against Borrelia burgdorferi. Int. J. Antimicrob. Agents 21:313-318. [DOI] [PubMed] [Google Scholar]
- 14.Hunfeld, K. P., E. Ruzic-Sabljic, D. E. Norris, P. Kraiczy, and F. Strle. 2005. In vitro susceptibility testing of Borrelia burgdorferi sensu lato isolates cultured from patients with erythema migrans before and after antimicrobial chemotherapy. Antimicrob. Agents Chemother. 49:1294-1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunfeld, K. P., T. A. Wichelhaus, R. Rodel, G. Acker, V. Brade, and P. Kraiczy. 2004. Comparison of in vitro activities of ketolides, macrolides, and an azalide against the spirochete Borrelia burgdorferi. Antimicrob. Agents Chemother. 48:344-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson, C. R., J. A. Boylan, J. G. Frye, and F. C. Gherardini. 2007. Evidence of a conjugal erythromycin resistance element in the Lyme disease spirochete Borrelia burgdorferi. Int. J. Antimicrob. Agents 30:496-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kraiczy, P., J. Weigand, T. A. Wichelhaus, P. Heisig, H. Backes, V. Schafer, G. Acker, V. Brade, and K. P. Hunfeld. 2001. In vitro activities of fluoroquinolones against the spirochete Borrelia burgdorferi. Antimicrob. Agents Chemother. 45:2486-2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maraspin, V., E. Ruzic-Sabljic, and F. Strle. 2006. Lyme borreliosis and Borrelia spielmanii. Emerg. Infect. Dis. 12:1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nefedova, V. V., E. I. Korenberg, V. I. Andreichuk, N. B. Gorelova, A. V. Markov, I. A. Fadeeva, and I. L. Evstaf'ev. 2005. Genetic characterization of pathogenic Borrelia, group A14S, isolated in Ukraine. Zh. Mikrobiol. Epidemiol. Immunobiol. 4:23-27. (In Russian.) [PubMed] [Google Scholar]
- 20.Postic, D., M. V. Assous, P. A. Grimont, and G. Baranton. 1994. Diversity of Borrelia burgdorferi sensu lato evidenced by restriction fragment length polymorphism of rrf (5S)-rrl (23S) intergenic spacer amplicons. Int. J. Syst. Bacteriol. 44:743-752. [DOI] [PubMed] [Google Scholar]
- 21.Preac Mursic, V., W. Marget, U. Busch, D. Pleterski Rigler, and S. Hagl. 1996. Kill kinetics of Borrelia burgdorferi and bacterial findings in relation to the treatment of Lyme borreliosis. Infection 24:9-16. [DOI] [PubMed] [Google Scholar]
- 22.Richter, D., D. Postic, N. Sertour, I. Livey, F. R. Matuschka, and G. Baranton. 2006. Delineation of Borrelia burgdorferi sensu lato species by multilocus sequence analysis and confirmation of the delineation of Borrelia spielmanii sp. nov. Int. J. Syst. Evol. Microbiol. 56:873-881. [DOI] [PubMed] [Google Scholar]
- 23.Richter, D., D. B. Schlee, R. Allgower, and F. R. Matuschka. 2004. Relationships of a novel Lyme disease spirochete, Borrelia spielmani sp. nov., with its hosts in central Europe. Appl. Environ. Microbiol. 70:6414-6419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sicklinger, M., R. Wienecke, and U. Neubert. 2003. In vitro susceptibility testing of four antibiotics against Borrelia burgdorferi: a comparison of results for the three genospecies Borrelia afzelii, Borrelia garinii, and Borrelia burgdorferi sensu stricto. J. Clin. Microbiol. 41:1791-1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skuballa, J., R. Oehme, K. Hartelt, T. Petney, T. Bucher, P. Kimmig, and H. Taraschewski. 2007. European hedgehogs as hosts for Borrelia spp., Germany. Emerg. Infect. Dis. 13:952-953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steere, A. C., and L. Glickstein. 2004. Elucidation of Lyme arthritis. Nat. Rev. Immunol. 4:143-152. [DOI] [PubMed] [Google Scholar]
- 27.Strle, F., Y. Cheng, J. Cimperman, V. Maraspin, S. Lotric-Furlan, J. A. Nelson, M. M. Picken, E. Ruzic-Sabljic, and R. N. Picken. 1995. Persistence of Borrelia burgdorferi sensu lato in resolved erythema migrans lesions. Clin. Infect. Dis. 21:380-389. [DOI] [PubMed] [Google Scholar]
- 28.Wang, G., A. P. van Dam, and J. Dankert. 1999. Phenotypic and genetic characterization of a novel Borrelia burgdorferi sensu lato isolate from a patient with Lyme borreliosis. J. Clin. Microbiol. 37:3025-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wormser, G. P., R. J. Dattwyler, E. D. Shapiro, J. J. Halperin, A. C. Steere, M. S. Klempner, P. J. Krause, J. S. Bakken, F. Strle, G. Stanek, L. Bockenstedt, D. Fish, J. S. Dumler, and R. B. Nadelman. 2006. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 43:1089-1134. [DOI] [PubMed] [Google Scholar]
- 30.Xu, Y., and R. C. Johnson. 1995. Analysis and comparison of plasmid profiles of Borrelia burgdorferi sensu lato strains. J. Clin. Microbiol. 33:2679-2685. [DOI] [PMC free article] [PubMed] [Google Scholar]