Abstract
We report a case of tension pneumothorax after an endoscopic sphincterotomy. A 78-yr-old woman presented with progressing dyspnea. She had undergone an endoscopic retrograde cholangiopancreatogram three days before due to acute cholecystitis. She underwent endoscopic sphincterotomy for stone extraction, but the procedure failed. On arrival to our hospital, she complained about severe dyspnea and she had subcutaneous emphysema. A computed tomogram scan revealed severe subcutaneous emphysema, right-side tension pneumothorax, and pneumoretroperitoneum. Contrast media injected through a transnasal biliary drainage catheter spilled from the second portion of the duodenum. A second abdominal computed tomogram showed multiple air densities in the retroperitoneum and peritoneal cavity, which were consistent with panperitonitis. We recommended an emergent laparotomic exploration, but the patient's guardians refused. She died eventually due to septic shock. Endoscopic retrograde cholangiopancreatogram is a popular procedure for biliary and pancreatic diseases, but it can cause severe complications such as intestinal perforation. Besides perforations, air can spread through the abdominal cavity, retroperitoneum, mediastinum, and the neck soft tissue, eventually causing pneumothorax. Early recognition and appropriate management is crucial to an optimal output of gastrointestinal perforation and pneumothorax.
Keywords: Pneumothorax, Cholangiopancreatography, Sphincterotomy, Complications
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is one of several popular procedures for biliary or pancreatic duct diseases. Recently, it has been used in lithotripsy, endoprosthesis placement, stone extraction, and sphincterotomy. However, it has also many complications from mild inflammation to severe life-threatening bleeding or perforations. Intestinal perforations after endoscopic procedures can cause pneumothorax, but this is rare especially for tension pneumothorax.
We describe a case of duodenal perforation with tension pneumothorax after an endoscopic sphincterotomy.
CASE REPORT
A 78-yr-old woman came to our hospital complaining of dyspnea. A physical exam revealed normal vital signs except mild tachypnea. She showed mild subcutaneous emphysema at the face and upper extremities. Breathing sounds were decreased at the entire thorax. A transnasal biliary drainage catheter was placed in her nose. Three days before, she had been admitted to another hospital due to acute cholecystitis. An abdominal computed tomography (CT) at that time showed multiple stones in the biliary tract. An ERCP was performed showing dilated biliary tract and multiple bile duct stones. The endoscopic sphincteropapillotomy was done for stone removal, but failed to remove them all. A large stone of about 1.5 cm remained, so they introduced a transnasal biliary drainage catheter. In the evening, she complained of dyspnea and visited emergency center of our hospital.
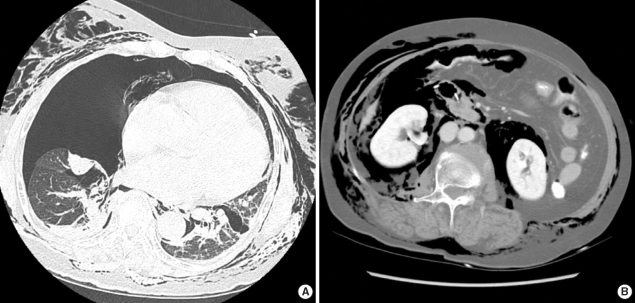
A simple chest roentgenogram showed severe subcutaneous emphysema and pneumomediastinum. Chest CT showed subcutaneous emphysema and pneumomediastinum with right pneumothorax (Fig. 1). A concomitantly abdominal computed tomogram showed retroperitoneal air shadow especially around the left kidney (Fig. 1). Leftward mediastinal shifting was also shown, so we did a tube thoracostomy at the right thorax. After closing the thoracostomy, her dyspnea disappeared. Soon after, the fluid from the chest tube drainage was green colored, and its bilirubin amount was 2.0 dL/mL. There were no clinical findings suggesting mediastinitis or esophageal perforation.
Fig. 1.
The initial chest and abdominal computed tomograms showing severe subcutaneous emphysema, pneumothorax, pneumomediastinum, deviated mediastinum and pneumoperitoneum.
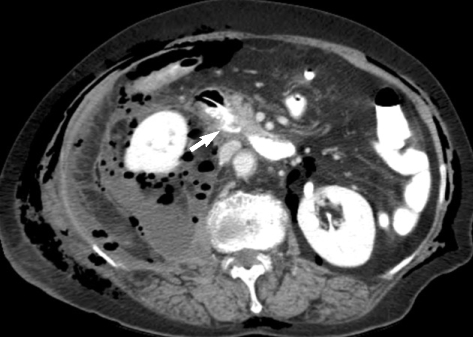
The next morning, the patient suffered from severe abdominal pain with tenderness and rebound tenderness. We suspected that duodenal perforation had developed after the endoscopic sphincterotomy, so we injected contrast media via the biliary drainage catheter that had been introduced before, and we did an abdominal CT scan. The scan showed the contrast media at the retroperitoneum around the second portion of the duodenum and retroperitoneal abscess around the right kidney, and multiple air densities in the retroperitoneum and peritoneal cavity, which were consistent with panperitonitis (Fig. 2). We recommended an emergent laparotomy, but her guardians did not want any surgical procedure. So we did only conservative management, but eventually she died because of septic shock month after admission.
Fig. 2.
An abdominal computed tomogram after injection of contrast media via biliary drainage catheter. The scan shows catheter and retroperitoneal dye spillage (arrow).
DISCUSSION
ERCP is a procedure that is gaining more popularity in the diagnosis and treatment of biliary and pancreatic disease, but it has many complications. As invasiveness of the procedure increases, more serious complications such as perforations or bleedings develop. Common complications of ERCP are pancreatitis, cholangitis, hemorrhage, and duodenal perforations (1). Other unusual complications such as cardiopulmonary and sedation related complications or electrical injuries may occur. Life-threatening complications such as a septic cholangitis or severe bleeding can also develop even though their rates are low (2).
ERCP-related perforations can present as retroperitoneal duodenal perforations, which are most commonly seen, free bowel wall perforations, or perforation of the bile duct. Stapfer et al. classified ERCP-related duodenal injuries in four types: type 1 is an injury of the lateral duodenal wall, type 2 is an injury at the sphincter of Oddi, type 3 is a ductile injury, and type 4 is single retroperitoneal air (3).
The incidence rate of perforation complications due to ERCP is about 1%, and the mortality rate of ERCP-related perforations goes from 16% to 18% (3).
Pneumothorax or pneumomediastinum have been reported second to gastrointestinal perforations, including perforation after endoscopic sphincterotomy. However, diagnostic endoscopy can also cause pneumothorax by esophageal perforation or without gastrointestinal perforation (4). Tension pneumothorax after endoscopic sphincterotomy and colonoscopy have been also reported (4, 5). However, some cases were detected shortly after ERCP procedures, which did not have any evidence of duodenal perforation by radiographic findings. Only one case was similar to our case that pneumothorax developed several hours after procedure and had radiologically confirmed duodenal perforation (6). If duodenal perforation were not proven, one should consider the possibility of pneumatic trauma from high pressure air inflation during procedures. Although pneumothorax after ERCP or colonoscopy is not uncommon, tension pneumothorax is relatively rare. Once perforation occurs, intraluminal air can travel to the thorax through the retroperitoneum or abdominal cavity via various routes. If the perforation occurs during an endoscopic sphincterotomy, pneumoretroperitoneum could develop. The visceral space is a connecting and continuous fascial compartment extending from the retroperitoneum to the mediastinum, and eventually to the neck (7). So pneumomediastinum can develop after pneumoretroperitoneum. Should the mediastinal pleura rupture, pneumothorax develops. Torn pleura can act as a check valve causing accumulation of air in thoracic cavity due to pressure gradient. Large bore is not essential for tension pneumothorax. It can develop even after one or two days later if intestinal air leakage were continued. When pneumothorax develops, it can compromise the patient. In general, pneumothorax complications due to ERCP can be diagnosed using fluoroscopy. So if the patient complains about any chest discomfort, a physician consider to pneumothorax.
Early recognition and appropriate management is essential to optimal output in perforation complications due to ERCP. Surgical indications after duodenal perforation are acute peritoneal irritation signs with or without sepsis, documentation of large contrast extravasation, presence of intra- or retroperitoneal fluid collections, or suspected perforation with retained material. In the absence of these indications and if the perforation is recognized at an early stage, conservative management can be attempted (8). According to Stapfer et al., type 1 perforations were usually managed by surgery, while surgery is less likely in other types (3).
We hereby report a case of tension pneumothorax after ERCP, which is rare but should be taken into consideration in patients who complain of respiratory discomfort during or after endoscopic procedures.
References
- 1.Loperfido S, Angelini G, Benedetti G, Chilovi F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1–10. doi: 10.1016/s0016-5107(98)70121-x. [DOI] [PubMed] [Google Scholar]
- 2.Pohle T, Domschke W, Lerch MM. Needle knife precut-induced bleeding from a "pancreatic cyst". Gastrointest Endosc. 2000;52:564–566. doi: 10.1067/mge.2000.108662. [DOI] [PubMed] [Google Scholar]
- 3.Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191–198. doi: 10.1097/00000658-200008000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeno BR, Sahn SA. Colonoscopy-associated pneumothorax: a case of tension pneumothorax and review of the literature. Am J Med Sci. 2006;332:153–155. doi: 10.1097/00000441-200609000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Morley AP, Lau JY, Young RJ. Tension pneumothorax complicating a perforation of a duodenal ulcer during ERCP with endoscopic sphincterotomy. Endoscopy. 1997;29:332. doi: 10.1055/s-2007-1004205. [DOI] [PubMed] [Google Scholar]
- 6.Gya D, Sali A, Angus D. Subcutaneous emphysema and pneumothorax following endoscopic sphincterotomy. Aust N Z J Surg. 1989;59:900–902. doi: 10.1111/j.1445-2197.1989.tb07038.x. [DOI] [PubMed] [Google Scholar]
- 7.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447–1453. [PubMed] [Google Scholar]
- 8.Margantinis G, Sakorafas GH, Kostopoulos P, Kontou S, Tsiakos S, Arvanitidis D. Post-ERCP/endoscopic sphincterotomy duodenal perforation is not always a surgical emergency. Dig Liver Dis. 2006;38:434–436. doi: 10.1016/j.dld.2005.10.023. [DOI] [PubMed] [Google Scholar]