Abstract
The influenza virus genes that confer efficient transmission of epidemic and pandemic strains in humans have not been identified. The rapid spread and severe disease caused by the 1918 influenza pandemic virus makes it an ideal virus to study the transmissibility of potentially pandemic influenza strains. Here, we used a series of human 1918-avian H1N1 influenza reassortant viruses to identify the genetic determinants that govern airborne transmission of avian influenza viruses. We have demonstrated that the 1918 HA gene was necessary for efficient direct contact transmission, but did not allow respiratory droplet transmission between ferrets of an avian influenza virus possessing an avian polymerase subunit PB2. The 1918 PB2 protein was found to be both necessary and sufficient for airborne transmission of a virus expressing the 1918 HA and neuraminidase. Also, it was found that influenza viruses that were able to transmit efficiently in ferrets were able to replicate efficiently at the lower temperature (33 °C) found in the environment of mammalian airway. These findings demonstrate that the adaptation of the HA and PB2 proteins are critical for the development of pandemic influenza strains from avian influenza viruses.
Keywords: ferrets, 1918 pandemic
Influenza pandemics occur after the emergence of a novel influenza A virus subtype that can efficiently replicate and spread among humans, due to lack of preexisting immunity to the novel hemagglutinin (HA). At present, the avian influenza H5N1 subtype virus, responsible for at least 387 human H5N1 infections and 245 deaths (1, 2), is considered a significant threat to global public health (3, 4). However, these viruses have failed to transmit efficiently between humans, a critical property of pandemic influenza strains. The severe disease caused by H5N1 viruses raises the possibility of another pandemic similar to the “Spanish” influenza pandemic of 1918–1919, which resulted in an estimated 50 million deaths worldwide (5). Despite active investigation (6, 7), the exact influenza virus genes that confer efficient transmission of epidemic and pandemic strains in humans have not been identified.
The recent reconstruction and characterization of the highly pathogenic and transmissible 1918 H1N1 pandemic strain provides a useful tool to understand the factors that may lead to the emergence of future pandemic influenza viruses (8). The ability of the 1918 pandemic virus to transmit through the air by means of respiratory droplets is of particular interest, because efficient transmission by means of this route is a critical property of pandemic influenza strains. Studies to investigate the transmissibility of the 1918 pandemic virus have been carried out in ferrets, which, based on accumulated data, are the best available animal model to study transmission of avian and human influenza viruses (7, 9–11). The reconstructed 1918 virus is both transmissible and lethal to ferrets (12). The receptor binding preference of the 1918 HA is critical for this high-transmissibility phenotype in ferrets (12). Influenza viruses use cell surface glycans with terminal sialic acid (SA) moieties as receptors for cell entry. Avian influenza virus HAs preferentially recognize α2,3 linked SA receptors, which are abundant in the gastrointestinal tract of poultry and wild birds (13), whereas those from human viruses preferentially recognize α2,6 linked SA receptors, which are present in the upper respiratory tract of both humans and ferrets (14–17). The current evidence suggests that the 1918 influenza pandemic was caused by viruses with 2 receptor-binding variants: A/South Carolina/1/1918 (SC18) and A/Brevig Mission/1/1918, like A/London/1/1918, possess the human α2,6 SA receptor preference, whereas natural variants A/New York/1/1918 and A/London/1/1919 possess a mixed α2,6/α2,3 SA specificity (18). This receptor binding preference for either α2,3 or α2,6 linked SA can be modulated by mutation of amino acid residues at positions 190 and 225 (H3 numbering) in the H1 subtype HA (19, 20). Human H1 proteins that bind α2,6 SA, including the parental South Carolina HA of 1918, contain an aspartate at both positions (Asp190 and Asp225), whereas α2,3 binding avian viruses contain glutamate at position 190 (Glu190) and glycine at position 225 (Gly225) (19). Generation of a mutant 1918 virus with an α2,3 binding HA (AV18) resulted in loss of transmissibility in the ferret model (12). This finding suggests that a binding preference for α2,6 linked SA receptors was an essential property of the 1918 pandemic strain, and is consistent with the observation that the pandemics of 1957 and 1968 were also caused by viruses with a preference for α2,6 linked SA (16). However, it remains unclear whether this “human” receptor binding preference is sufficient for transmission among mammals. Also, the precise influenza virus genes required of an avian influenza virus to transmit efficiently through the air has remained elusive.
In the present investigation, we used the reconstructed 1918 influenza virus and ferrets as a model to identify the genetic determinants that confer the transmission phenotype observed among human influenza viruses. We report here that H1N1 recombinant influenza viruses possessing the 1918 HA and polymerase subunit PB2 spread efficiently through the air to naive ferrets. These findings demonstrate that the adaptation of the HA and PB2 proteins are critical for the development of pandemic influenza strains from avian influenza viruses, and serve as an important baseline that can now be extended to other subtypes, including H5N1, which pose an immediate pandemic threat.
Results
Transmissibility of Avian and Human H1N1 Influenza Viruses.
Using the ferret model, we examined the airborne transmissibility (referred to as respiratory droplet transmissibility) of modern H1N1 avian and human influenza viruses. In these studies, 3 animals were inoculated intranasally (i.n.) with 106 pfu of virus; ≈24 h later, inoculated-contact animal pairs were established by placing a naive ferret in each of 3 adjacent cages with perforated side walls, allowing exchange of respiratory droplets without direct or indirect contact (7). Virus replication was monitored in both inoculated and contact animals by collection of nasal washes (NWs) and titration of virus by serial dilution in embryonated chicken eggs as previously described (7). Also, transmission to contact animals was assessed by the titration of virus specific antibodies in convalescent serum [collected days 18–21 postinoculation (p.i.)/postcontact (p.c.)] by using a hemagglutination inhibition (HI) assay. Overall, we found that 5 modern avian H1N1 strains possessing “avian” receptor binding amino acids (Glu190 and Gly225) did not transmit to contact animals by means of respiratory droplets, whereas efficient transmission occurred with a human H1N1 virus possessing human receptor binding residues (Asp190 and Asp225) [supporting information (SI) Table S1 and Fig. S1]. All viruses tested replicated to high titers in the ferret upper respiratory tract with similar kinetics in the inoculated animals (Table S1 and Fig. S1).
Two representative avian influenza viruses, A/Duck/Alberta/35/76 (Dk/Alb/76) and A/Duck/New York/15024–21/96 (Dk/NY/96), were examined further for the ability to transmit by direct contact. In these experiments, a naive animal was placed in the same cage as each of 3 inoculated animals, such that paired animals had both direct contact with each other and indirect contact by means of shared food and water sources. Dk/Alb/76 and Dk/NY/96 viruses transmitted inefficiently between ferrets by direct contact, with virus recovered from the NWs of and seroconversion detected in 1 of 3 contact animals (Table 1). Collectively, these findings indicate that, unlike human H1N1 viruses, avian H1N1 viruses do not transmit efficiently by either respiratory droplets or direct contact in the ferret model, consistent with the transmission data obtained with contemporary avian influenza H5N1 viruses (7).
Table 1.
Direct contact transmission of wild-type and mutant avian and human H1N1 viruses
| Virus | Inoculated animals |
Contact Animals |
||||
|---|---|---|---|---|---|---|
| Clinical symptoms |
No. with virus detection(peak titer)‡ | No. with seroconversion(HI titer range)§ | No. with virus detection(peak titer)‡ | No. with seroconversion(HI titer range)§ | ||
| No. with weight loss (%)* | No. sneezing (onset day)† | |||||
| A/Duck/Alberta/35/76 | 2/3 (3.7) | 0/3 | 3/3 (6.9) | 3/3 (80–160) | 1/3 (6.5) | 1/3 (160) |
| A/Duck/NewYork/15024-21/96¶ | 3/3 (9.1) | 0/3 | 3/3 (6.2) | 3/3 (1,280) | 1/3 (8.0) | 1/3 (1,280) |
| Dk/NY/96-DD | 3/3 (8.0) | 0/3 | 3/3 (6.3) | 3/3 (640) | 1/3 (6.5) | 1/3 (640) |
| 1918NA:Dk/NY/96-DD | 3/3 (9.8) | 1/3 (5) | 3/3 (6.2) | 3/3 (320) | 0/3 | 1/3 (40) |
| 1918HANA:Dk/NY/96 | 3/3 (11.3) | 1/3 (4) | 3/3 (6.8) | 3/3 (320–640) | 3/3 (7.4) | 3/3 (320–640) |
*Number of animals in which weight loss was observed. Values in parentheses indicate percentage mean maximum weight loss observed during the first 9 days p.i.
†Number of animals in which sneezing was observed during the first 9 days of the experiment. Values in parentheses indicate day of onset.
‡Number of animals in which virus was detected in nasal washes. Values in parentheses indicate nasal wash titers, which are expressed as mean log10 peak virus titer observed within the first 9 days p.i.
§Number of animals in which seroconversion was observed. Values in parentheses show HI antibody titers in sera collected at least 18 days p.i. HI titers were determined using the homologous virus as test antigen.
¶The transmission of a reverse genetics generated A/Dk/NY/15024/96 virus was also examined and was similar to the wild-type virus.
The 1918 Virus Surface Glycoproteins Confer Direct Contact Transmissibility of an Avian H1N1 Virus.
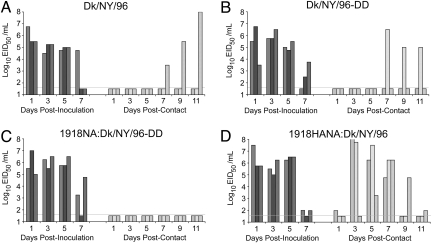
The inability of the Dk/NY/96 virus to transmit efficiently to contact animals provided a framework to identify the viral factors that are required for efficient virus transmission, which can lead to sustained pandemic spread. To test the hypothesis that an α2,6 SA receptor binding preference would allow transmission of an avian H1N1 strain, we constructed a mutant Dk/NY/96 virus containing Asp190 and Asp225 by introduction of point mutations into the HA. Recombinant viruses containing either the mutant (Dk/NY/96-DD) and a wild-type HA (Dk/NY/96) were rescued by using standard reverse genetics techniques, and the receptor binding phenotype of each virus was verified by using a previously described red blood cell (RBC) resialylation assay (20). As expected, the wild-type Dk/NY/96 virus agglutinated α2,3 but not α2,6 resialylated RBCs, whereas the Dk/NY/96-DD mutant virus agglutinated α2,6 but not α2,3 SA containing RBCs (data not shown). Neither Dk/NY/96-DD nor the parental avian virus (Dk/NY/96) transmitted to contact animals in respiratory droplet experiments (Table 2, Fig. S2), and both viruses transmitted to only 1 of 3 contact animals in the direct contact transmission model (Fig. 1 A and B and Table 1). Next, a Dk/NY/96-DD virus containing the 1918 neuraminidase (NA) protein (1918NA:Dk/NY/96-DD) was generated to exclude the possibility that the lack of transmission observed with Dk/NY/96-DD was due to HA-NA incompatibility, and to investigate a possible role for NA in transmission. This virus did not show enhanced transmissibility in contact or respiratory droplet experiments (Fig. 1C, Table 1, and Fig. S2), suggesting that 1918 NA alone is not sufficient for virus transmission. A virus containing the HA and NA from the 1918 pandemic virus with remaining Dk/NY/96 virus genes (1918HANA:Dk/NY/96) also failed to transmit by means of respiratory droplets; virus was not detected in contact ferret NWs, and no seroconversion of contact animals was observed (Fig. 2A, Table 2). However, this virus transmitted to 100% of contact animals in multiple direct contact experiments, supporting a specific role for the 1918 HA in virus transmission among ferrets (Fig. 1D and Table 1). It is important to note that lack of efficient transmission of avian H1N1 viruses or reassortant H1N1 viruses in these experiments cannot be attributed to reduced virus replication in the upper respiratory tract of ferrets. To address the possibility that nontransmitting viruses replicated less efficiently than those that transmitted, we performed a statistical analysis of day 1 virus titers in directly inoculated animals. Day 1 was chosen based on the observation that in efficiently transmitting viruses, virus was present in contact animals by day 3 p.i. ANOVA analysis of the day 1 NW titers of all 4 viruses (Dk/NY/96, Dk/NY96-DD, 1918NA:Dk/NY/96-DD, and 1918HANA:Dk/NY/96-DD) showed no significant differences between transmissible and nontransmissible viruses. Collectively, these experiments demonstrate that the 1918 HA protein, when expressed together with the 1918 NA, confers efficient contact transmission between ferrets, but is not sufficient for transmission by means of respiratory droplets.
Table 2.
Respiratory droplet transmission of 1918-avian reassortant H1N1 viruses
| Virus | Inoculated Animals |
Contact Animals |
||||
|---|---|---|---|---|---|---|
| Clinical Symptoms | No. with virus detection(peak titer)‡ | No. with seroconversion(HI titer range)§ | No. with virus detection(peak titer)‡ | No. with seroconversion(HI titer range)§ | ||
| No. with weight loss (%)* | No. sneezing (onset day)† | |||||
| A/Dk/NY/96 | 2/3 (6) | 1/3 (3) | 3/3 (6.3) | 3/3 (1280) | 0/3 | 0/3 |
| Dk/NY/96-DD | 3/3 (11.1) | 0/3 | 3/3 (6.6) | 3/3 (320–1,280) | 0/3 | 0/3 |
| 1918NA:Dk/NY/96-DD | 3/3 (10.6) | 1/3 (3) | 3/3 (6.3) | 3/3 (160) | 0/3 | 0/3 |
| 1918HANA:Dk/NY/96 | 3/3 (9.1) | 2/3 (4) | 3/3 (6.5) | 3/3 (320–640) | 0/3 | 0/3 |
| Dk/NY/96HANA:1918 | 3/3 (13.2) | 0/3 | 3/3 (7.4) | ND¶ | 0/3 | ND |
| 1918HANAPB1PB2PA:Dk/NY/96 | 2/3 (6.8) | 3/3 | 3/3 (8.2) | 3/3 (80–320) | 2/3 (7.5) | 2/3 (160–320) |
| 1918HANAPB1PB2:Dk/NY/96 | 2/3 (16.2) | 3/3 (2) | 3/3 (7.8) | 3/3 (320–640) | 3/3 (6.4) | 3/3 (320–640) |
| 1918HANAPB1:Dk/NY/96 | 3/3 (12.4) | 3/3 (2) | 3/3 (7.1) | 3/3 (160–640) | 0/3 | 0/3 |
| 1918HANAPB2:Dk/NY/96 | 3/3 (12.9) | 2/3 (4) | 3/3 (8.1) | 3/3 (320) | 3/3 (7.1) | 3/3 (160/320) |
| 1918HANAPA:Dk/NY/96 | 3/3 (17.5) | 0/3 | 3/3 (8.4) | 3/3 (320–640) | 0/3 | 0/3 |
| Dk/NY/96-PB2:1918 | 3/3 (10.4) | 2/3 (2) | 3/3 (7.4) | 3/3 (320–640) | 1/3 (7.5) | 1/3 (320) |
*Number of animals in which weight loss was observed. Values in parentheses indicate percentage mean maximum weight loss observed during the first 9 days p.i.
†Number of animals in which sneezing was observed during the first 9 days of the experiment. Values in parentheses indicate day of onset.
‡Number of animals in which virus was detected in nasal washes. Values in parentheses indicate nasal wash titers, which are expressed as mean log10 peak virus titer observed within the first 9 days p.i.
§Number of animals in which seroconversion was observed. Values in parentheses show HI antibody titers in sera collected at least 18 days p.i. HI titers were determined using the homologous virus as test antigen.
¶ND, not determined.
Fig. 1.
Direct contact transmissibility of wild-type, mutant, and reassortant avian H1N1 viruses. We inoculated 3 ferrets with 106 EID50 of Dk/NY/96 (A), Dk/NY/96-DD (B), 1918NA:Dk/NY/96-DD (C), or 1918HANA:Dk/NY/96 (D). One day p.i., a naive ferret was placed in each cage to establish contact between the animal pairs. Viral replication was monitored by titration of NWs collected every other day in both inoculated (Left) and contact (Right) animals. The limit of detection was 101.5 EID50/mL, and is indicated by a solid line on each representation.
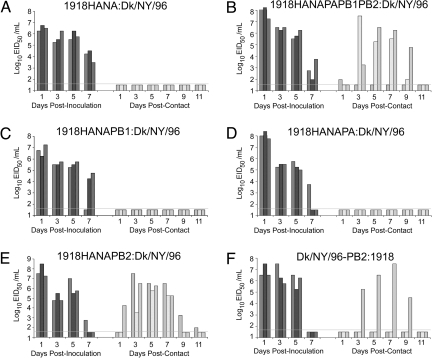
Fig. 2.
Respiratory droplet transmissibility of 1918-Dk/NY/96 reassortant H1N1 viruses. We inoculated 3 ferrets with 106 EID50 of 1918-DK/NY/96 reassortant viruses containing the 1918 HA and NA (A), the 1918 HA, NA, PB1, PB2, and PA (B), the 1918 HA, NA, and PB1 (C), the 1918 HA, NA, and PA (D), and the1918 HA, NA, and PB2 (E). Also, the transmissibility of a 1918 virus containing the Dk/NY/96 PB2 gene was examined (F). All animals were housed individually in specialized cages that permit exchange of respiratory droplets, but prevent direct or indirect contact between inoculated-contact animal pairs. One day p.i., a naive contact animal was placed in each adjacent cage. Viral replication was monitored by titration of NWs collected every other day in both inoculated (Left) and contact (Right) animals. The limit of detection was 101.5 EID50/mL, and is indicated by a solid line on each representation.
Identification of the PB2 Gene As a Critical Determinant for Respiratory Droplet Transmissibility.
The lack of respiratory droplet transmission observed with the 1918HANA:Dk/NY/96 virus suggested that, although the internal proteins of Dk/NY/96 are sufficient for contact transmission, they are inadequate to support respiratory droplet transmission (Fig. 2A, Table 2). To identify internal proteins from the 1918 pandemic virus that confer respiratory droplet transmissibility, we constructed a series of 1918:Dk/NY/96 reassortants containing selected internal genes as well as the HA and NA proteins from the 1918 pandemic strain. Strikingly, a virus containing the 1918 PA, PB1, and PB2 genes, in addition to the HA and NA, transmitted to 2 of 3 naive ferrets by the respiratory droplet route, suggesting that the polymerase complex has a critical role in this mode of transmission of the 1918 pandemic strain (Fig. 2B, Table 2). To identify which genes from the polymerase complex were responsible for this enhanced virus transmissibility, we generated a series of reassortant viruses containing the 1918 HA, NA, and either the 1918 PA, PB1, or PB2 genes. The viruses containing the PA or PB1 genes did not transmit by respiratory droplets, despite efficient replication in the ferret upper respiratory tract of inoculated animals (Fig. 2 C and D and Table 2). In contrast, a virus containing the HA, NA, and PB2 genes from the 1918 virus transmitted efficiently to all naive ferrets, as measured by both virus detection in NWs and seroconversion (Fig. 2E and Table 2). To confirm the role of PB2 in virus transmission, we tested a virus containing the Dk/NY/96 PB2 gene with all remaining genes from the 1918 pandemic virus (Dk/NY/96-PB2:1918). Compared with the fully reconstructed 1918 pandemic strain, which transmitted rapidly and efficiently to contact animals by means of respiratory droplets, the 1918 virus containing the avian PB2 (Dk/NY96-PB2:1918) transmitted inefficiently (Fig. 2F, Table 2). These results demonstrate a requirement for the PB2 gene in this efficiently transmitting pandemic strain.
Role of PB2 Position 627 in Avian H1N1 Virus Transmissibility.
The presence of a lysine residue at position 627 of the 1918 PB2 protein was of particular interest, as this residue has been previously identified as a determinant of pathogenicity for H5N1 viruses, and has been suggested to allow more efficient growth at the lower temperatures encountered in the upper airway of mammals (21, 22). To test the hypothesis that a lysine at position 627 in the 1918 PB2 protein is necessary for transmission, we tested the transmissibility of a mutant 1918 virus containing the avian consensus residue, a glutamic acid, at this position (1918-PB2-K627E). This mutation resulted in greatly reduced transmission (1/5 animals positive) in respiratory droplet studies, but did not affect the ability of the virus to transmit in direct contact experiments (Fig. 3). Sequencing of viruses from inoculated and contact animals demonstrated maintenance of the K627E mutation; no wild-type revertant viruses were observed. This pattern of transmission suggests that a lysine at PB2 position 627 is specifically necessary for transmission of the 1918 virus through the air.
Fig. 3.
Respiratory droplet and contact transmissibility of 1918-PB2-K627E. The 1918-PB2K627E mutant virus was tested in respiratory droplet (A) and direct contact (B) transmission experiments. In both cases, ferrets were inoculated with 106 EID50 of 1918-PB2-K627E. Viral replication was monitored by titration of NWs collected every other day in both inoculated (Left) and contact (Right) animals. The limit of detection was 101.5 EID50/mL, and is indicated by a solid line on each representation.
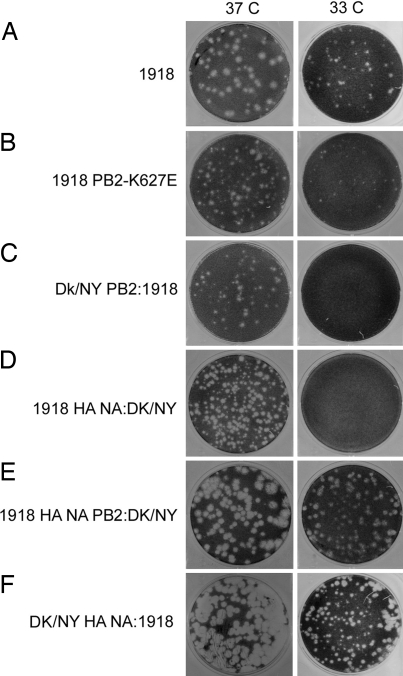
To elucidate how the PB2 gene, and amino acid position 627 in particular, affects the transmissibility of avian H1N1 viruses, we evaluated the plaque phenotypes of the 1918-avian H1N1 influenza reassortant viruses (Fig. 4). The residue 627 was shown to contribute to host range and to the temperature sensitivity of avian viral replication in mammalian cells (23, 24). Plaque assays were performed in triplicate and incubated at either 37 °C or 33 °C. We found that the reconstructed 1918 virus was able to form plaques at both 37 °C and 33 °C (Fig. 4A). In contrast, reassortant viruses possessing a glutamic acid at position 627 (K627E) were unable to form significant plaques, indicating a substantial impairment in plaque formation at the lower temperature. Also, avian H1N1 virus and human 1918 virus containing PB2 from avian virus could not form plaques at the lower temperature. However, the PB2 gene from the human 1918 pandemic strain, not the HA and NA gene, can support an avian H1N1 virus to form clear plaques at the lower temperature (Fig. 4), confirming the importance of a human adapted PB2 gene for efficient virus transmission by supporting virus replication in the lower temperature environment present in the mammalian airway.
Fig. 4.
Plaque morphology of MDCK cells infected with H1N1 reassortant viruses. Confluent monolayers of MDCK cells were inoculated with the indicated H1N1 reassortant viruses, incubated at either 37 °C or 33 °C for 48 h, and visualized for plaque morphology.
Discussion
Collectively, the findings presented in this study demonstrate that the 1918 HA and PB2 contribute to the transmissibility of the 1918 pandemic influenza virus. Transmission did not occur for avian influenza viruses with a α2,3 SA receptor specificity, for avian viruses with mutations in the HA gene conferring a specificity for alpha 2,6 receptors, or for avian viruses with such mutations and the 1918 NA gene. Although the reassortant viruses and the 1918 mutants possessed the 1918 NA, the 1918 NA protein alone was not sufficient for transmission of an avian virus with a receptor specificity for α2,6 SA receptor preference. The receptor binding specificity of virus surface HA is shown here to be critical for transmission by direct contact. However, in the absence of other factors, this receptor specificity is insufficient for respiratory droplet transmission. Avian reassortant or wild-type H1N1 viruses containing an avian PB2 gene failed to spread to naive ferrets by respiratory droplets, whereas viruses containing the PB2 protein from the human 1918 pandemic strain, along with the 1918 HA transmitted efficiently by means of respiratory droplets. Our findings suggest that human adaptation of the PB2 proteins of avian influenza viruses, including potentially pandemic H5N1 viruses, is required to generate viruses readily transmissible through the air.
All 3 of the 20th century influenza pandemics were caused by viruses containing human adapted PB2 genes. Recent work has examined the sequences of human and avian PB2 proteins and, based on amino acid alignments, have identified a set of 6 amino acids hypothesized to be responsible for human-to-human transmission (25). Alignment of Dk/NY/96 virus and 1918 virus PB2 proteins show a total of 10-aa differences, at positions 108, 114, 199, 473, 475, 477, 539, 576, 627, and 702. These changes occur in domains that are suggested by previous research to have various functions including mRNA cap-binding and PB1 binding (26–28). Although testing each mutation was beyond the scope of this work, we did see a clear affect of the K627E PB2 mutation on transmission of the 1918 virus through the air. It is interesting to note that, in general, lysine is present at 627 among the human influenza viruses that do transmit efficiently, whereas a glutamic acid is found in the position among the avian influenza isolates.
Identification of the PB2 protein as a critical determinant of respiratory droplet transmission in the ferret suggests a number of interesting hypotheses concerning the mechanism of transmission among mammals. Several studies demonstrate that the PB2 protein from pathogenic H5N1 isolates can increase virulence by enhancing replicative efficiency both in vitro and in vivo, but does not alter cell tropism (21, 29). Also, it has been shown that the H5N1 PB2 contributes to increased replication at lower temperatures encountered in the nasal passages of mice (22). In the current study, the K627 to E mutation resulted in a substantial impairment in plaque formation at the lower temperature. However, it is interesting to note that despite the reduction in plaque size in vitro, the 627E mutant virus reached similar peak titers as the parental 1918 virus in vivo. The NWs most likely contain a collection of viruses from multiple cell types present in the ferret airway and not solely from cells that are responsible for efficient virus transmission. Thus, it is reasonable to speculate that the 627E mutant virus is not replicating efficiently in the putative airway cells involved in shedding the virus into the air. Also, the 1918 HA protein, which is shown here and previously to be a determinant for direct contact transmission, binds specifically to goblet cells in ferret as well as human respiratory tissue(s) (12, 30). Enhanced cell tropism, provided by the HA, could allow viruses to bind a subset of cells in the upper respiratory tract that are critical for transmission. However, PB2 may be further required to optimize replication after entry into these cells; thus, promoting transmission. Examination of the tissue distribution of the reassortants evaluated here, as well as in vitro studies in primary respiratory cell cultures, may provide clues as to the mechanism of enhanced transmission.
Materials and Methods
Viruses.
Wild-type virus stocks were grown in the allantoic cavity of 10- to 11-day-old embryonated eggs of a hen (10). The EID50 titer for each stock was calculated by the method of Reed and Muench after serial titration in eggs (31). Recombinant virus stocks were grown on Madin–Darby canine kidney (MDCK) cells, by using the previously described reconstructed genes of the 1918 pandemic influenza virus (32) and reverse genetics system (33–35). The PFU titer for each cell-grown stock was determined by plaque assay (8). Recombinant viruses were confirmed by RT-PCR and sequencing. Research with viruses containing 1918 gene segments was conducted under biosafety level 3 containment, including enhancements required by the United States Department of Agriculture/Centers for Disease Control Select Agent Program (36). Staff conducting this research were on antiviral prophylaxis and adhered to stringent biosafety precautions to protect the researchers, the environment, and the public.
Ferret Transmission Studies.
Male Fitch ferrets 6–12 months of age (Triple F Farms) were used in all transmission studies. Ferrets were housed throughout each experiment in cages within a Duo-Flo Bioclean mobile clean room (Lab Products) and were determined to be negative for antibody to circulating influenza A (H1N1, H3N2) and Influenza B viruses. Ferrets were inoculated with 106 pfu or EID50 of virus in a total volume of 1 mL (500 μL per nostril), and NWs were collected every 48 h (10). Respiratory droplet and contact transmission experiments were conducted as previously described (7) (Fig. S3). Convalescent serum from all ferrets was collected days 18–21 p.i./p.c. and tested for H1 HA antibodies by using homologous virus and 0.5% turkey or 1% horse RBCs as described (37).
Determination of Plaque Morphology.
Confluent monolayers of MDCK cells on 6-well plates were inoculated in triplicate with indicated recombinant viruses for 1 h. After incubation, the cells were washed, and an overlay consisting of a mixture of 1.6% agarose and double-strength L-15 medium (Cambrex Bio Science), with N-p-tosyl-l-phenylalanine chloromethyl ketone (TPCK)-treated trypsin (Sigma-Aldrich) was added to the cells. After incubating at either 37 °C or 33 °C for 48 h, cells were fixed, stained with 0.1% crystal violet, and visualized for plaque morphology.
Supplementary Material
Acknowledgments.
We thank Eddie Jackson for exceptional care of animals used in this study. The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the funding agency. This work was partially supported by National Institutes of Health Grant PO1 AI058113 (to A.G.-S.), Northeast Biodefense Center Grant U54 AI057158, and Center for Investigating Viral Immunity and Antagonism Grant U19 AI62623. R.S. was supported by the Singapore–Massachusetts Institute of Technology Alliance for Research and Technology.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0813172106/DCSupplemental.
References
- 1.Chen JM, Chen JW, Dai JJ, Sun YX. A survey of human cases of H5N1 avian influenza reported by the WHO before June 2006 for infection control. Am J Infect Control. 2007;35:467–469. doi: 10.1016/j.ajic.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Subbarao K, et al. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science. 1998;279:393–396. doi: 10.1126/science.279.5349.393. [DOI] [PubMed] [Google Scholar]
- 3.Ungchusak K, et al. Probable person-to-person transmission of avian influenza A (H5N1) N Engl J Med. 2005;352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 4.Kandun IN, et al. Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med. 2006;355:2186–2194. doi: 10.1056/NEJMoa060930. [DOI] [PubMed] [Google Scholar]
- 5.Perrone LA, Tumpey TM. Reconstruction of the 1918 pandemic influenza virus: How revealing the molecular secrets of the virus responsible for the worst pandemic in recorded history can guide our response to future influenza pandemics. Infect Disord Drug Targets. 2007;7:294–303. doi: 10.2174/187152607783018772. [DOI] [PubMed] [Google Scholar]
- 6.Yen HL, et al. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol. 2007;81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maines TR, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci USA. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tumpey TM, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 9.Zitzow LA, et al. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J Virol. 2002;76:4420–4429. doi: 10.1128/JVI.76.9.4420-4429.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maines TR, et al. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lowen AC, Palese P. Influenza virus transmission: Basic science and implications for the use of antiviral drugs during a pandemic. Infect Disord Drug Targets. 2007;7:318–328. doi: 10.2174/187152607783018736. [DOI] [PubMed] [Google Scholar]
- 12.Tumpey TM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 13.Ito T, et al. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J Virol. 1998;72:7367–7373. doi: 10.1128/jvi.72.9.7367-7373.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shinya K, Kawaoka Y. Influenza virus receptors in the human airway. Uirusu. 2006;56:85–89. doi: 10.2222/jsv.56.85. [DOI] [PubMed] [Google Scholar]
- 15.Connor RJ, Kawaoka Y, Webster RG, Paulson JC. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology. 1994;205:17–23. doi: 10.1006/viro.1994.1615. [DOI] [PubMed] [Google Scholar]
- 16.Matrosovich M, et al. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol. 2000;74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leigh MW, Connor RJ, Kelm S, Baum LG, Paulson JC. Receptor specificity of influenza virus influences severity of illness in ferrets. Vaccine. 1995;13:1468–1473. doi: 10.1016/0264-410x(95)00004-k. [DOI] [PubMed] [Google Scholar]
- 18.Reid AH, et al. 1918 influenza pandemic caused by highly conserved viruses with two receptor-binding variants. Emerg Infect Dis. 2003;9:1249–1253. doi: 10.3201/eid0910.020789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevens J, et al. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol. 2006;355:1143–1155. doi: 10.1016/j.jmb.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 20.Glaser L, et al. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol. 2005;79:11533–11536. doi: 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 22.Hatta M, et al. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 2007;3:1374–1379. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subbarao EK, London W, Murphy BR. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J Virol. 1993;67:1761–1764. doi: 10.1128/jvi.67.4.1761-1764.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Massin P, van der Werf S, Naffakh N. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J Virol. 2001;75:5398–5404. doi: 10.1128/JVI.75.11.5398-5404.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miotto O, Heiny A, Tan TW, August JT, Brusic V. Identification of human-to-human transmissibility factors in PB2 proteins of influenza A by large-scale mutual information analysis. BMC Bioinformatics. 2008;9:S18. doi: 10.1186/1471-2105-9-S1-S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hatta M, et al. Mapping of functional domains on the influenza A virus RNA polymerase PB2 molecule using monoclonal antibodies. Arch Virol. 2000;145:1947–1961. doi: 10.1007/s007050070068. [DOI] [PubMed] [Google Scholar]
- 27.Poole E, Elton D, Medcalf L, Digard P. Functional domains of the influenza A virus PB2 protein: Identification of NP- and PB1-binding sites. Virology. 2004;321:120–133. doi: 10.1016/j.virol.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 28.Ohtsu Y, Honda Y, Sakata Y, Kato H, Toyoda T. Fine mapping of the subunit binding sites of influenza virus RNA polymerase. Microbiol Immunol. 2002;46:167–175. doi: 10.1111/j.1348-0421.2002.tb02682.x. [DOI] [PubMed] [Google Scholar]
- 29.Shinya K, et al. PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology. 2004;320:258–266. doi: 10.1016/j.virol.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 30.Srinivasan A, et al. Quantitative biochemical rationale for differences in transmissibility of 1918 pandemic influenza A viruses. Proc Natl Acad Sci USA. 2008;105:2800–2805. doi: 10.1073/pnas.0711963105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reed LJ, Muench HA. A simple method of estimating fifty per cent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 32.Pappas C, et al. Single gene reassortants identify a critical role for PB1, HA, and NA in the high virulence of the 1918 pandemic influenza virus. Proc Natl Acad Sci USA. 2008;105:3064–3069. doi: 10.1073/pnas.0711815105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Basler CF, et al. Sequence of the 1918 pandemic influenza virus nonstructural gene (NS) segment and characterization of recombinant viruses bearing the 1918 NS genes. Proc Natl Acad Sci USA. 2001;98:2746–2751. doi: 10.1073/pnas.031575198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fodor E, et al. Rescue of influenza A virus from recombinant DNA. J Virol. 1999;73:9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tumpey TM, et al. Existing antivirals are effective against influenza viruses with genes from the 1918 pandemic virus. Proc Natl Acad Sci USA. 2002;99:13849–13854. doi: 10.1073/pnas.212519699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richmond JY, McKinney RW. In: Biosafety in Microbiological and Biomedical Laboratories. 5th Ed. Richmond JY, McKinney RW, editors. Atlanta: Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 37.Stephenson I, Wood JM, Nicholson KG, Zambon MC. Sialic acid receptor specificity on erythrocytes affects detection of antibody to avian influenza haemagglutinin. J Med Virol. 2003;70:391–398. doi: 10.1002/jmv.10408. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.