Abstract
The gastrointestinal (GI) tract is the system of organs within multi-cellular animals that takes in food, digests it to extract energy and nutrients, and expels the remaining waste. The various patterns of GI tract function are generated by the integrated behaviour of multiple tissues and cell types. A thorough study of the GI tract requires understanding of the interactions between cells, tissues and gastrointestinal organs in health and disease. This depends on knowledge, not only of numerous cellular ionic current mechanisms and signal transduction pathways, but also of large scale GI tissue structures and the special distribution of the nervous network. A unique way of coping with this explosion in complexity is mathematical and computational modelling; providing a computational framework for the multilevel modelling and simulation of the human gastrointestinal anatomy and physiology. The aim of this review is to describe the current status of biomechanical modelling work of the GI tract in humans and animals, which can be further used to integrate the physiological, anatomical and medical knowledge of the GI system. Such modelling will aid research and ensure that medical professionals benefit, through the provision of relevant and precise information about the patient’s condition and GI remodelling in animal disease models. It will also improve the accuracy and efficiency of medical procedures, which could result in reduced cost for diagnosis and treatment.
Keywords: Gastrointestinal tract, Computational modelling, Biomechanics, Remodelling, Disease
INTRODUCTION
The gastrointestinal (GI) tract, also called the digestive tract or the alimentary canal, is the system of organs within multicellular animals that takes in food, digests it to extract energy and nutrients, and expels the remaining waste. The major functions of the GI tract are digestion facilitated by motility, secretion and absorption. The various patterns of GI tract function are generated by the integrated behaviour of multiple tissues and cell types. Medical imaging methods such as ultrasonography[1,2], magnetic resonance imaging (MRI)[3,4], and endoscopic ultrasound (EUS)[5,6] are well known stand-alone clinical methods that can disclose structural and functional abnormalities of the GI tract. However, a thorough study of the GI tract requires understanding of the interactions between cells, tissues and gastrointestinal organs in health and disease. This depends on knowledge, not only of numerous cellular ionic current mechanisms and signal transduction pathways, but also of large-scale GI tissue structures and the special distribution of the nervous network. A unique way of coping with this explosion in complexity is mathematical and computational modelling; providing a computational framework and Information Communication Technology (ICT) based tools for multilevel modelling and simulation of the human gastrointestinal anatomy and physiology[7–9]. Computer-based analysis, visualisation, modelling and simulation are used routinely in fields such as engineering, meteorology or traffic control to understand the behaviour and outcomes of new designs and impact of external phenomena well in advance of their realisation, thereby avoiding costly failures. In GI tract studies, this approach is not common, mainly because we still lack those models that can emulate the behaviour of the human body. Nevertheless, exploration of the GI tract has dramatically improved by the introduction of cross sectional imaging modalities such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI), which have revolutionised the way in which many conditions are diagnosed and treated. The ability to examine, in detail, structures inside the GI tract without resorting to surgery, has allowed clinicians to diagnose problems and plan corrective procedures with a minimum of risk to the patient[10,11]. In order to continue this exploration, it will be necessary to complement the traditional approach with an integrative approach that combines observation, theory and prediction across the temporal and dimensional scales, across scientific disciplines, and across the anatomical subsystems, all of which reflect the rather artificial divisions described.
The aim of this review is to describe the currently status of biomechanical modelling work on the GI tract in humans and animals that can be further used to integrate the physiological, anatomical and medical knowledge of the GI system.
ANATOMY AND FUNCTION OF THE GI TRACT
The GI tract is a continuous channel through the body with the biliary and pancreatic ducts as major side-branches. The GI tract consists of a series of organs, which resemble one another in constitution, being variously arranged as cylinders, spheroids, or intermediate forms. The main functions of the GI tract are transport and digestion of food. The different segments show a large variation in morphology and muscle mechanical properties, i.e. the oesophagus mainly serves to quickly transport the food bolus from the mouth to the stomach where the food in the stomach is stored for some time whilst simultaneously being broken down into smaller components. The GI sphincters serve to separate the GI tract into compartments. However, the gut is also important for immune functions[12]. The wall of the GI tract is typically composed of four layers, i.e., the mucosa, submucosa, muscle and serosa (some parts are called the adventitia where there is no epithelium) (Figure 1). The muscle layer consists of an outer longitudinal and an inner circular muscle layer. The collagen-rich submucosa and mucosa layers are inside the muscle layer. Another thin layer of muscle, the muscularis mucosae, exists almost throughout the entire tract. The motions of the GI tract accomplish a net antegrade flow in order to mix the contents and move them across the surface where absorption occurs. The contractile patterns and transit vary greatly from one part of the tract to another. The GI wall movements during digestion and absorption are the consequence of contractions of the two layers of smooth musculature. Contractions of the longitudinal muscle layer shorten the gut wall, whereas the peristaltic contractions of the circular muscle layer, in contrast, mainly produce forward transit with relatively little mixing. The contractions of circumferential and longitudinal muscles occur together, most of the time. The enteric nervous system (ENS), composed of both the myenteric (inter-muscular) plexus and the submucosal plexus, is distributed in the GI tract from the oesophagus to the internal anal sphincter[13]. A network of nerves of the myenteric plexus is embedded in the loose collagen matrix between the longitudinal and circular muscle layers (Figure 1). This set of nerves is essential for the regulation of the contractions of the adjacent musculature. Between the nerve endings and smooth muscle are the interstitial cells of Cajal (ICCs), which have been shown to be critical for the generation and propagation of the electrical slow waves that regulate the phasic contractile activity of GI smooth muscle, and for mediating neurotransmission from enteric motor neurons to smooth muscle cells[14,15]. The ENS ensures that the GI tract can fulfil essential tasks even when isolated from the rest of the body. The GI tract is - on the other hand - unable to work normally without the integrative functions of the ENS. Malfunctions of the ENS are increasingly recognized as underlying factors in many GI diseases. The exogenous nerves running together with the sympathetic and parasympathetic nervous systems are also important in regulating blood flow and secretion etc[16]. They also encode the conscious sensations from the gut such as fullness, urge to defecate and pain[17]. Medical imaging methods such as ultrasonography, MRI, and endoscopic ultrasound (EUS) are well known stand-alone clinical methods that can disclose structural and functional abnormalities of the GI tract[6,18]. Therefore, modelling analysis based on the anatomy and structure of the GI tract and different imaging methods can be applied to the problems related to function and pathophysiology.
Figure 1.
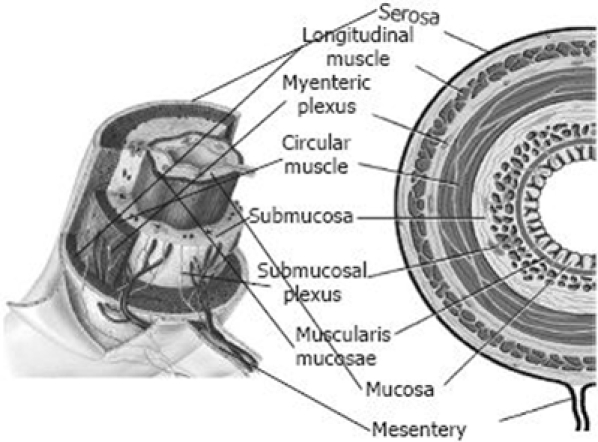
Schematic diagram of the GI tract.
DISEASE CAUSING TISSUE AND STRUCTURE REMODELLING OF THE GI TRACT
The GI tract, like other hollow organs such as the heart, blood vessels, urinary bladder and the urethra, is functionally subjected to dimensional changes. Hence, biomechanical properties are of particular functional importance. Data on the biomechanical properties are crucial for the understanding of the normal function of the GI tract and dysfunction due to disease because, (1) peristaltic motion that propels the food through the GI tract is a result of interaction of the passive and active tissue forces and the hydrodynamic forces in the food bolus and (2) remodelling of the mechanical properties reflects the changes in the tissue structure that determine a specific sensory-motor dysfunction.
Human studies have documented that diabetes melitus[19] and systemic sclerosis[20] induce biomechanical GI remodelling. Using different animal models (Figure 2), we have demonstrated that biomechanical and histomorphological remodelling occur in the GI tract due to normal physiological growth[21,22], malnutrition[23,24], inflammation, obstruction[25–27], bowel resection[28], diabetes[29–33], radiation injury[34], collagen changes[35,36] and EGF treatment. The morphometric properties are best described at the zero-stress state where no internal or external forces deform the tissue. Furthermore, knowing the zero-stress configuration is essential in any mechanical analysis since it serves as the reference state for computing stress and strain under physiological or pathophysiological conditions. With reference to the zero-stress state, combining the morphometry data and pressure data, we can compute the stress-strain relationship of the GI wall. The stress-strain distribution mainly reflects the elastic properties of the GI tract. Changes in the elastic properties reflect structural remodelling of the GI wall in different diseases. Therefore, we consider the opening angle of the zero-stress state, residual strain and stress-strain relationship as the most relevant biomechanical parameters to describe diseases causing GI remodelling. Generally, diseases and factors inducing tissue overgrowth, such as diabetes[37–40], obstruction and EGF[41–45] treatment, increase GI wall stiffness; whereas factors reducing tissue growth, such as fasting and low protein diet decrease GI wall stiffness. The more collagen in the GI wall, the stiffer the wall is[20], and vice versa. However, the effect of different factors on the opening angle and residual strain of GI tract depend on the changes of layered structure. Fung’s hypothesis of non-uniform remodelling states that if the inner wall grows more than the outer wall, the opening angle will increase[46] whereas if the outer wall grows more than the inner wall, the opening angle will decrease. Table 1 summarizes the histomorphological and biomechanical remodelling of the GI tract caused by different diseases.
Figure 2.
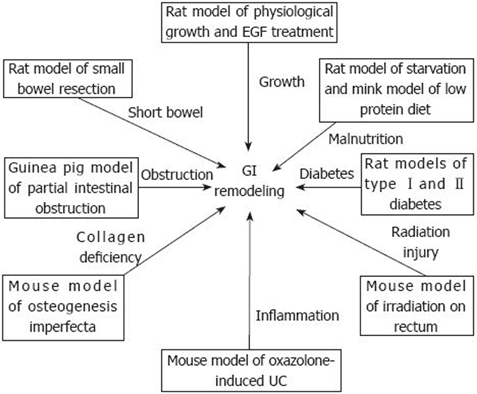
Disease-induced GI remodeling in animal models.
Table 1.
| Diseases | Species | Test organs |
Histomorphometric remodeling |
Biomechanical remodeling |
||||
| WT | WA | LT | OA | RES | Stiffness | |||
| Type Idiabetes | Human | Esophagus | ↑ | ND | ND | ND | ND | Circ NC Long↑ |
| Duodenum | ND | ND | ND | ND | Circ NC Long↑ | |||
| Rat | Esophagus | ↑ | ↑ | Mu↑Su↑Ms↑ | ↓ | ↓ | Circ↑Long ND | |
| Duodenum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↓ | ↓ | Circ↑Long↑ | ||
| Jejunum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↑Long↑ | ||
| Ileum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↑Long↑ | ||
| Colon | ↑ | ↑ | Mu↑Su↑Ms↑ | Circ↑Long↑ | ||||
| Type II diabetes | Rat | Esophagus | ↑ | ↑ | Mu↑Su↑Ms↑ | ↓ | ↓ | Circ↑Long ND |
| Stomach | ND | ND | ND | ND | ND | Circ↑ | ||
| Systemic sclerosis | Human | Duodenum | ND | ND | ND | ND | ND | Circ↑ |
| Ulcerative colitis | Mice | Colon | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↑Long↑↑ |
| Fasting | Rat | Duodenum | ↓ | ↓ | Mu↓ Su↓ | ↑ | ↑ | Circ↓ Long↓ |
| Jejunum | ↓ | ↓ | Mu↓ Su↓ | ↑ | ↑ | Circ↓ Long↓ | ||
| Ileum | ↓ | ↓ | Mu↓ Su↓ | ↑ | ↑ | Circ↓ Long↓ | ||
| Low protein diet | Mink | Duodenum | ↓ | ↓ | NC | NC | NC | Circ↓ Long NC |
| Jejunum | ↓ | ↓ | Mu↓ Su↓ | ↓ | ↓ | Circ↓ Long NC | ||
| Ileum | ↓ | ↓ | Mu↓ Su↓ Ms↓ | ↓ | Circ↓ Long NC | |||
| Partial obstruction | Opossum | esophagus | ND | ND | ND | ND | ND | Circ↑Long ND |
| Guinea pig | Jejunum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↓ | ↓ | Circ↑Long ND | |
| Osteogenesis imperfecta | Mice | Esophagus | ↓ | ↓ | Mu↓ Su↓ Ms↓ | ↑ | ↑ | ND |
| Irradiation | Mice | Rectum | ↑ | ↑ | ND | ↑ | ↑ | ND |
| Small bowel resection | Rat | Jejunum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | NC |
| Ileum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | NC | ||
| EGF treatment | Rat | Esophagus | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↑Long ND |
| Duodenum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↑Long NC | ||
| Jejunum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↓ Long↑ | ||
| Ileum | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | Circ↓ Long↑ | ||
| Colon | ↑ | ↑ | Mu↑Su↑Ms↑ | ↑ | ↑ | ND | ||
WT: Wall thickness; WA: Wall cross-sectional area; OA: Opening angle; RES: Residual strain; LT: Layered wall thickness; Mu: Mucosa; Su: Submucosa; Ms: Muscle; Circ: Circumferential direction; Long: Longitudinal direction; ND: Not done; NC: No change.
It is well known that mechanosensation is important for GI function. Mechanosensitive nerve endings exist extensively in the GI tract where they serve a critical role in homeostasis. The mechanosensitive afferents in the intrinsic and extrinsic pathways have been described as low-, wide-dynamic- or high-threshold tension-receptors[12]. Therefore, the GI tract structure, as well as the stress and strain distribution in the wall, is important for the GI sensory and motor function. The GI wall structure or deformation changes caused by a disease will alter the relative positions of the mechanosensitive afferents (zero setting of the mechanosensitive afferents). The biomechanical remodelling by the disease, such as alterations of residual strain, stress distribution and wall stiffness, will alter the tension and stress distribution of the mechanosensitive afferents. As a result, the perception and motility of the GI tract will also change. Therefore, the morphological changes and biomechanical remodelling of the GI tract are likely to affect the function of mechanosensitive afferents in the GI wall and further affect the motor and sensory functions.
BIOMECHANICAL MODELLING OF THE GI TRACT
The use of numerical models and, in particular, of finite element models has been extensively studied in the field of soft tissue mechanics because of the potential they offer in the analysis of the mechanical behaviour of morphologically complex structures, with high structural hierarchy and constituents with non-linear behaviour[47,48]. The effectiveness of numerical models depends on reliable reconstructions of the morphometry of the anatomical site under investigation, the specific loading and boundary conditions, as well as the definition of constitutive models capable of describing the mechanical response of the single tissues. Gastroenterology research has traditionally been based on experimental approaches rather than on mathematical modelling. Most of the previous modelling efforts in the biological area were in the cardiac and lung field; but, other areas are in now being developed. However, in the past five to ten years several groups have independently started to model the GI tract.
The large morphological complexity of the GI tract and the variability in the different parts of the tract are well known. The complexity increases in the characteristic folds of the connection regions[49–51]. With regard to the structural conformation of GI tract tissues, the inner mucosa and submucosa layers are surrounded by the outer muscular and serosa layers. Collagen fibres of submucosa form a complex network and are oriented in different directions. The muscular layers have muscle fibres oriented in the circumferential direction (circumferential muscle layer) or the longitudinal direction (longitudinal muscle layer). As a consequence, the GI tract tissue must be considered as a multi-layered composite material, made up of tissues with different mechanical characteristics[12,52–54]. Some of the components show a specific spatial disposition of the sub-structures, such as collagen and muscle fibres, and are studied by means of a constitutive formulation already adopted in other fields for the mechanics of biological tissues, based on the theory of fibre-reinforced materials[55–57]. The most current investigations of the GI tissue properties are mainly focused on seeking the constitutive equation and the associated constitutive parameters of the physiological or pathological status. To date, most GI structure and tissue property studies have been based on animal experiments. Medical device development has made it possible to study the mechanical behaviour of the GI tract in vivo[58–62].
The methods and current developments in studies of the biomechanical properties of normal and disease remodelled GI tissues have been described in the above sections. Hereafter, the establishment of morphometric-related modelling of the GI tract will be briefly introduced. According to the reconstruction methods on GI modelling, the establishment of the GI models can be divided into in vivo medical images-based models, the anatomical-based models and the theoretical analysis-based models.
In vivo medical images-based GI models
Advances in imaging are introduced initially as research tools and subsequently as clinical diagnostic tests. Medical image-based 3-D models of in vivo GI organs have characterized the oesophagus, stomach, small intestine, sigmoid colon, oesophageal gastric junction and the rectum, based on cross-sectional imaging using ultrasonography, computed tomography (CT), Functional Luminal Imaging Probe (FLIP) or magnetic resonance imaging (MRI)[3,4,63–68]. With the development of the medical devices such as impedance planimetry, it is now possible to record the mechanical parameters such as the luminal pressure simultaneously with the cross-sectional medical images. Therefore, the in vivo mechanical behaviour of the organs can be computed on the basis of the reconstructed GI morphometric models and the recorded mechanical parameter. A reconstructed sigmoid-colon model and the corresponding tension and stress distribution on the model are illustrated as an example in Figure 3. Detailed descriptions of in vivo GI modelling analysis can be found in studies of Liao et al[66] and Frokjaer et al[3,4].
Figure 3.
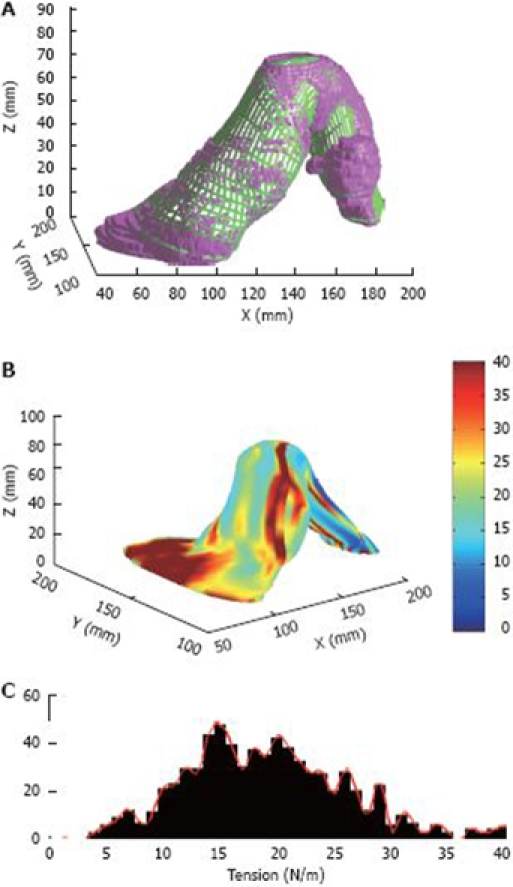
A reconstructed sigmoid-colon model and the corresponding tension distribution. A: A representative sigmoid colon model with the distension volume of 200 mL. The model with purple colour is the solid model generated directly from the MR images, and the green mesh is the smoothened surface, the comparison between the solid model and smoothened surface indicates that the smoothened model fits well with the original solid model; B: The circumferential curvature distribution on the surface models; C: Tension distribution of the sigmoid colon surface model.
Anatomy-based GI modelling
For modelling analysis using the in vivo image based models, only the tension or stress was computed on the basis of three-dimensional surface geometry using the Laplace’s equation, and the wall thickness. The tissue structure was, therefore, not taken into account. To aid in understanding of the relationship between the structure and function of the GI tract in healthy and diseased states, an anatomically-based finite element model is needed. The anatomically based visualization GI model is now commercially available, however the GI anatomy based numerical modelling analyses are mainly been done by Andrew Pullan’s group so far, and all models were built from the Visible Human Project[69–71]. The Visible Human project provided a set of cross sectional images of a human cadaver. On each image, data points around the organ boundary of interest were created and then the geometry models were constructed on the basis of the distinguished data clouds[71–75]. The anatomically-based models have now been used to investigate normal and pathological electrical activity of the stomach and small intestine[71–74], the muscle functions on the gastro-oesophageal junction during swallowing[75] and the blood flow in the mesenteric arterial system of the human intestine[69,70]. An example of the anatomically-based in vitro rat stomach model generated from ultrasonic scanning is illustrated in Figure 4.
Figure 4.
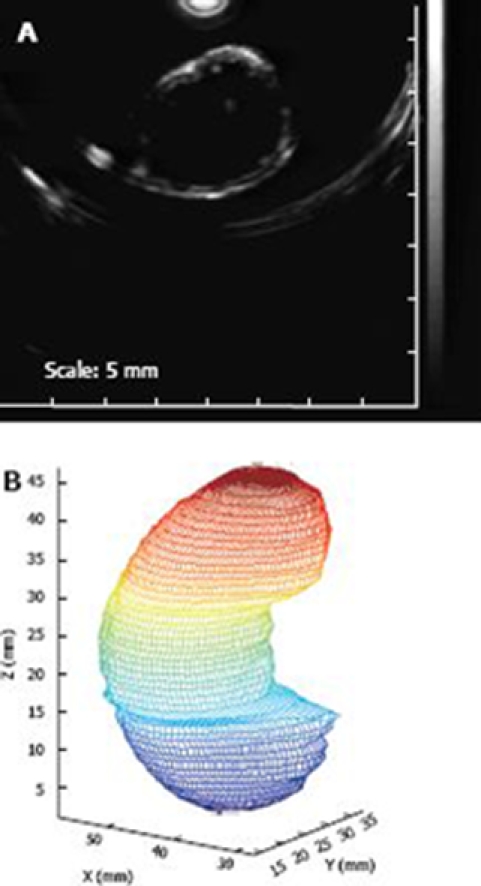
An example of the anatomically based in vitro rat stomach model generated from ultrasonic scanning. A: A representative CT scanning of a cross sectional slice of an in vitro rat stomach; B: The reconstructed gastric model on the basis of the CT scanning on the in vitro rat stomach. The distance between cross sectional slices was 1 mm, the colour change from blue to red means the increase of the stomach length in z direction.
Theoretical analysis-based GI modelling
The morphological complexity of the GI organs makes it difficult to build the anatomically-based finite element models. Hence, some numerical models of the GI organs were built on the basis of theoretical analysis by simplifying the complex GI morphometry as a regular geometry such as a circular cylinder for the oesophagus[52,57,64,68,76] and a sphere for the stomach pouch[77] and some regular tubes for describing the antrodudenal junction[78] and the oesophago-gastric junction[79]. In the morphometrically-simplified model, most of the biomechanical features such as the tissue structure, tissue properties and bolus flow can be expressed mathematically and, thus, the mechanical function of the GI tract can be simulated. The simplified GI tract models have existed for describing the muscle function[53,68,76], food transportation[77,78,80,81] and blood flow[65] in the GI tract in healthy and diseased situations. A simplified pouch model for describing the gastric emptying of a patient treated for obesity is illustrated in Figure 5 as an example. As can be seen, the emptying curves for the pouch based on the simplified model agree well with the clinical results.
Figure 5.
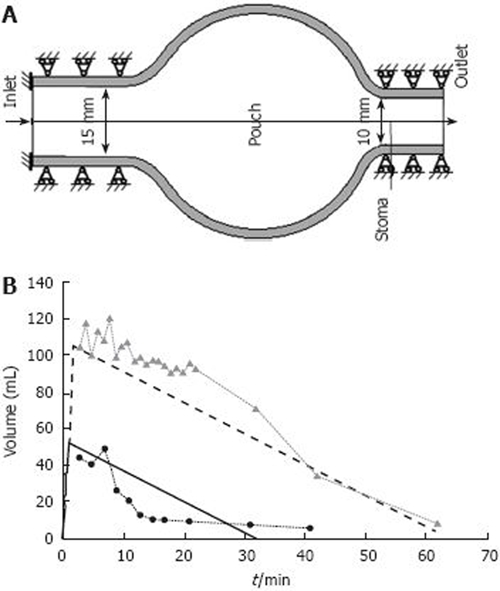
A simplified pouch model for describing the gastric emptying of a patient treated for obesity. A: A representative pouch model of midsized pouch with stoma diameter of 10 mm, B: Volume history in the filling and emptying phases in the mid-sized and large pouch models with stoma diameter of 10 mm. The solid line represents the mid-sized pouch, and the dotted line the large pouch. Circles and triangles represent volume data of the recorded clinical emptying curve for the mid-sized and large pouch. Pouch and stoma are a small fundic cavity and a corresponding narrow outlet between pouch and the rest of the stomach in gastroplasty and gastric bypass procedures for obesity.
PERSPECTIVE
GI modelling studies are focused on patient-specific computational modelling and simulation for prediction of disease or early diagnosis by integrating patient specific knowledge and predispositions obtained in biomedical imaging. Modelling studies of the GI tract will advance our understanding of the mechanisms of GI function and diseases, such as dyspepsia and visceral pain. Furthermore, an integrated GI tract simulation model will be beneficial for medical education, and for evaluation of the efficacy and safety of new drugs. The challenge of GI modelling is to develop mathematical and computational models of structure-function relations appropriate to each (limited) spatial and temporal domain, and then to link the parameters of a model at one scale to a more detailed description of structure and function on the adjacent levels. The present analytical tools can thus be integrated in order to analyze complex structures for understanding biomechanical behaviour in other visceral organs and be further integrated as a global GI model. The mechanical behaviour-related aspects of diseases of the sigmoid colon (diverticular disease, irritable bowel syndrome, etc), small bowel (motility disorders), stomach (motility disorders, non-ulcer dyspepsia, etc) and oesophagus (oesophagitis, gastro-oesophageal reflux disease, non-cardiac chest pain, etc) can be further developed by applying modified versions of the present models.
Footnotes
Supported by A grant from US National Institute of Health with No. 1RO1DK072616-01A2, and Karen Elise Jensen Fond
Peer reviewer:Jennifer Siggers, Department of Bioengineering, Imperial College London, South Kensington Campus, London, SW7 2AZ, United Kingdom
S- Editor Li LF L- Editor Stewart GJ E- Editor Yin DH
References
- 1.Berstad A, Hausken T, Gilja OH, Hveem K, Nesje LB, Odegaard S. Ultrasonography of the human stomach. Scand J Gastroenterol Suppl. 1996;220:75–82. doi: 10.3109/00365529609094755. [DOI] [PubMed] [Google Scholar]
- 2.Berstad A, Hausken T, Gilja OH, Nesland A, Odegaard S. Imaging studies in dyspepsia. Eur J Surg Suppl. 1998;220:42–49. doi: 10.1080/11024159850191436. [DOI] [PubMed] [Google Scholar]
- 3.Frokjaer JB, Liao D, Bergmann A, McMahon BP, Steffensen E, Drewes AM, Gregersen H. Three-dimensional biomechanical properties of the human rectum evaluated with magnetic resonance imaging. Neurogastroenterol Motil. 2005;17:531–540. doi: 10.1111/j.1365-2982.2005.00647.x. [DOI] [PubMed] [Google Scholar]
- 4.Frokjaer JB, Liao D, Steffensen E, Dimcevski G, Bergmann A, Drewes AM, Gregersen H. Geometric and mechanosensory properties of the sigmoid colon evaluated with magnetic resonance imaging. Neurogastroenterol Motil. 2007;19:253–262. doi: 10.1111/j.1365-2982.2006.00884.x. [DOI] [PubMed] [Google Scholar]
- 5.Gilja OH, Lunding J, Hausken T, Gregersen H. Gastric accommodation assessed by ultrasonography. World J Gastroenterol. 2006;12:2825–2829. doi: 10.3748/wjg.v12.i18.2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilja OH, Hatlebakk JG, Odegaard S, Berstad A, Viola I, Giertsen C, Hausken T, Gregersen H. Advanced imaging and visualization in gastrointestinal disorders. World J Gastroenterol. 2007;13:1408–1421. doi: 10.3748/wjg.v13.i9.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clapworthy GJ, Viceconti M. Seeing the EuroPhysiome: A roadmap to the Virtual Physiological Human. (Coordination Action #027642, STEP: A strategy for the EuroPhysiome) Vol. 13. Luton: University of Bedfordshire; 2007. [Google Scholar]
- 8.Hunter PJ, Nielsen PM, Bullivant D. The IUPS Physiome Project. International Union of Physiological Sciences. Novartis Found Symp. 2002;247:207–217; discussion 217-221, 244-252. [PubMed] [Google Scholar]
- 9.Hunter P, Nielsen P. A strategy for integrative computational physiology. Physiology (Bethesda) 2005;20:316–325. doi: 10.1152/physiol.00022.2005. [DOI] [PubMed] [Google Scholar]
- 10.Liao D, Lelic D, Gao F, Drewes AM, Gregersen H. Biomechanical functional and sensory modelling of the gastrointestinal tract. Philos Transact A Math Phys Eng Sci. 2008;366:3281–3299. doi: 10.1098/rsta.2008.0091. [DOI] [PubMed] [Google Scholar]
- 11.Gregersen H. The Giome project. Neurogastroenterol Motil. 2006;18:401–402. doi: 10.1111/j.1365-2982.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- 12.Gregersen H, Kassab G. Biomechanics of the gastrointestinal tract. Neurogastroenterol Motil. 1996;8:277–297. doi: 10.1111/j.1365-2982.1996.tb00267.x. [DOI] [PubMed] [Google Scholar]
- 13.Takaki M. Gut pacemaker cells: the interstitial cells of Cajal (ICC) J Smooth Muscle Res. 2003;39:137–161. doi: 10.1540/jsmr.39.137. [DOI] [PubMed] [Google Scholar]
- 14.Burns AJ. Disorders of interstitial cells of Cajal. J Pediatr Gastroenterol Nutr. 2007;45 Suppl 2:S103–S106. doi: 10.1097/MPG.0b013e31812e65e0. [DOI] [PubMed] [Google Scholar]
- 15.Sanders KM, Ordog T, Ward SM. Physiology and pathophysiology of the interstitial cells of Cajal: from bench to bedside. IV. Genetic and animal models of GI motility disorders caused by loss of interstitial cells of Cajal. Am J Physiol Gastrointest Liver Physiol. 2002;282:G747–G756. doi: 10.1152/ajpgi.00362.2001. [DOI] [PubMed] [Google Scholar]
- 16.Guyton AC, Hall JE. Medical Physiology. 10th ed. Vol. 282. Philadelphia: WB Saunders Company; 2000. [Google Scholar]
- 17.Drewes AM, Gregersen H, Arendt-Nielsen L. Experimental pain in gastroenterology: a reappraisal of human studies. Scand J Gastroenterol. 2003;38:1115–1130. doi: 10.1080/00365520310004399. [DOI] [PubMed] [Google Scholar]
- 18.Camilleri M. New imaging in neurogastroenterology: an overview. Neurogastroenterol Motil. 2006;18:805–812. doi: 10.1111/j.1365-2982.2006.00786.x. [DOI] [PubMed] [Google Scholar]
- 19.Frokjaer JB, Andersen SD, Ejskjaer N, Funch-Jensen P, Drewes AM, Gregersen H. Impaired contractility and remodeling of the upper gastrointestinal tract in diabetes mellitus type-1. World J Gastroenterol. 2007;13:4881–4890. doi: 10.3748/wjg.v13.i36.4881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pedersen J, Gao C, Egekvist H, Bjerring P, Arendt-Nielsen L, Gregersen H, Drewes AM. Pain and biomechanical responses to distention of the duodenum in patients with systemic sclerosis. Gastroenterology. 2003;124:1230–1239. doi: 10.1016/s0016-5085(03)00265-8. [DOI] [PubMed] [Google Scholar]
- 21.Gregersen H, Lu X, Zhao J. Physiological growth is associated with esophageal morphometric and biomechanical changes in rats. Neurogastroenterol Motil. 2004;16:403–412. doi: 10.1111/j.1365-2982.2004.00536.x. [DOI] [PubMed] [Google Scholar]
- 22.Lu X, Zhao J, Gregersen H. Small intestinal morphometric and biomechanical changes during physiological growth in rats. J Biomech. 2005;38:417–426. doi: 10.1016/j.jbiomech.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 23.Dou Y, Gregersen S, Zhao J, Zhuang F, Gregersen H. Effect of re-feeding after starvation on biomechanical properties in rat small intestine. Med Eng Phys. 2001;23:557–566. doi: 10.1016/s1350-4533(01)00091-1. [DOI] [PubMed] [Google Scholar]
- 24.Dou Y, Gregersen S, Zhao J, Zhuang F, Gregersen H. Morphometric and biomechanical intestinal remodeling induced by fasting in rats. Dig Dis Sci. 2002;47:1158–1168. doi: 10.1023/a:1015019030514. [DOI] [PubMed] [Google Scholar]
- 25.Gregersen H, Giversen IM, Rasmussen LM, Tottrup A. Biomechanical wall properties and collagen content in the partially obstructed opossum esophagus. Gastroenterology. 1992;103:1547–1551. doi: 10.1016/0016-5085(92)91176-5. [DOI] [PubMed] [Google Scholar]
- 26.Storkholm JH, Zhao J, Villadsen GE, Hager H, Jensen SL, Gregersen H. Biomechanical remodeling of the chronically obstructed Guinea pig small intestine. Dig Dis Sci. 2007;52:336–346. doi: 10.1007/s10620-006-9431-7. [DOI] [PubMed] [Google Scholar]
- 27.Storkholm JH, Zhao J, Villadsen GE, Gregersen H. Spontaneous and bolus-induced motility in the chronically obstructed guinea-pig small intestine in vitro. Dig Dis Sci. 2008;53:413–420. doi: 10.1007/s10620-007-9865-6. [DOI] [PubMed] [Google Scholar]
- 28.Dou Y, Lu X, Zhao J, Gregersen H. Morphometric and biomechanical remodelling in the intestine after small bowel resection in the rat. Neurogastroenterol Motil. 2002;14:43–53. doi: 10.1046/j.1365-2982.2002.00301.x. [DOI] [PubMed] [Google Scholar]
- 29.Jorgensen CS, Ahrensberg JM, Gregersen H, Flyvberg A. Tension-strain relations and morphometry of rat small intestine in experimental diabetes. Dig Dis Sci. 2001;46:960–967. doi: 10.1023/a:1010737323153. [DOI] [PubMed] [Google Scholar]
- 30.Liao D, Zhao J, Gregersen H. Three-dimensional geometry analysis of the stomach in type II diabetic GK rats. Diabetes Res Clin Pract. 2006;71:1–13. doi: 10.1016/j.diabres.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 31.Yang J, Zhao J, Zeng Y, Gregersen H. Biomechanical properties of the rat oesophagus in experimental type-1 diabetes. Neurogastroenterol Motil. 2004;16:195–203. doi: 10.1111/j.1365-2982.2004.00495.x. [DOI] [PubMed] [Google Scholar]
- 32.Yang J, Zhao J, Liao D, Gregersen H. Biomechanical properties of the layered oesophagus and its remodelling in experimental type-1 diabetes. J Biomech. 2006;39:894–904. doi: 10.1016/j.jbiomech.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 33.Zhao J, Frokjaer JB, Drewes AM, Ejskjaer N. Upper gastrointestinal sensory-motor dysfunction in diabetes mellitus. World J Gastroenterol. 2006;12:2846–2857. doi: 10.3748/wjg.v12.i18.2846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gregersen H, Lundby L, Overgaard J. Early and late effects of irradiation on morphometry and residual strain of mouse rectum. Dig Dis Sci. 2002;47:1472–1479. doi: 10.1023/a:1015894430400. [DOI] [PubMed] [Google Scholar]
- 35.Gregersen H, Weis SM, McCulloch AD. Oesophageal morphometry and residual strain in a mouse model of osteogenesis imperfecta. Neurogastroenterol Motil. 2001;13:457–464. doi: 10.1046/j.1365-2982.2001.00279.x. [DOI] [PubMed] [Google Scholar]
- 36.Fan Y, Zhao J, Liao D, Gregersen H. The effect of digestion of collagen and elastin on histomorphometry and the zero-stress state in rat esophagus. Dig Dis Sci. 2005;50:1497–1505. doi: 10.1007/s10620-005-2868-2. [DOI] [PubMed] [Google Scholar]
- 37.Zhao J, Sha H, Zhou S, Tong X, Zhuang FY, Gregersen H. Remodelling of zero-stress state of small intestine in streptozotocin-induced diabetic rats. Effect of gliclazide. Dig Liver Dis. 2002;34:707–716. doi: 10.1016/s1590-8658(02)80022-6. [DOI] [PubMed] [Google Scholar]
- 38.Zhao J, Liao D, Yang J, Gregersen H. Viscoelastic behavior of small intestine in streptozotocin-induced diabetic rats. Dig Dis Sci. 2003;48:2271–2277. doi: 10.1023/b:ddas.0000007862.50690.85. [DOI] [PubMed] [Google Scholar]
- 39.Zhao J, Yang J, Gregersen H. Biomechanical and morphometric intestinal remodelling during experimental diabetes in rats. Diabetologia. 2003;46:1688–1697. doi: 10.1007/s00125-003-1233-2. [DOI] [PubMed] [Google Scholar]
- 40.Zhao J, Liao D, Gregersen H. Biomechanical and histomorphometric esophageal remodeling in type 2 diabetic GK rats. J Diabetes Complications. 2007;21:34–40. doi: 10.1016/j.jdiacomp.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 41.Liao D, Yang J, Zhao J, Zeng Y, Vinter-Jensen L, Gregersen H. The effect of epidermal growth factor on the incremental Young’s moduli in the rat small intestine. Med Eng Phys. 2003;25:413–418. doi: 10.1016/s1350-4533(03)00020-1. [DOI] [PubMed] [Google Scholar]
- 42.Yang J, Zhao JB, Zeng YJ, Gregersen H. Biomechanical properties of ileum after systemic treatment with epithelial growth factor. World J Gastroenterol. 2003;9:2278–2283. doi: 10.3748/wjg.v9.i10.2278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang J, Zhao J, Zeng Y, Vinter-Jensen L, Gregersen H. Morphological properties of zero-stress state in rat large intestine during systemic EGF treatment. Dig Dis Sci. 2003;48:442–448. doi: 10.1023/a:1022516111538. [DOI] [PubMed] [Google Scholar]
- 44.Zhao J, Yang J, Vinter-Jensen L, Zhuang F, Gregersen H. Biomechanical properties of esophagus during systemic treatment with epidermal growth factor in rats. Ann Biomed Eng. 2003;31:700–709. doi: 10.1114/1.1575758. [DOI] [PubMed] [Google Scholar]
- 45.Zhao J, Yang J, Vinter-Jensen L, Zhuang F, Gregersen H. The morphometry and biomechanical properties of the rat small intestine after systemic treatment with epidermal growth factor. Biorheology. 2002;39:719–733. [PubMed] [Google Scholar]
- 46.Fung YC. Biomechanics mechanical properties of living tissues. Vol. 39. Berlin: Springer-Verlag; 1993. [Google Scholar]
- 47.Natali AN, Carniel EL, Pavan PG, Dario P, Izzo I, Menciassi A. VII Symposium of Computer Method in Biomechanics and Biomedical Engineering. Antibes: [publisher unknown]; 2006. Evaluation of the constitutive parameters for the numerical analysis of non linear mechanical response of soft tissues. [Google Scholar]
- 48.Natali AN, Carniel EL, Pavan PG, Dario P, Izzo I, Menciassi A, editors. 2006 IEEE/RAS-EMBS International Conference on Biomedical Robotics and Biomechatronics. Pisa: 2006. Hyperelastic models for the analysis of soft tissue mechanics: definition of constitutive parameters; pp. 1–8. [Google Scholar]
- 49.Liao D, Zhao J, Yang J, Gregersen H. The oesophageal zero-stress state and mucosal folding from a GIOME perspective. World J Gastroenterol. 2007;13:1347–1351. doi: 10.3748/wjg.v13.i9.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liao D, Cassin J, Zhao J, Gregersen H. The geometric configuration and morphometry of the rabbit oesophagus during luminal pressure loading. Physiol Meas. 2006;27:703–711. doi: 10.1088/0967-3334/27/8/005. [DOI] [PubMed] [Google Scholar]
- 51.Yang W, Fung TC, Chian KS, Chong CK. Three-dimensional finite element model of the two-layered oesophagus, including the effects of residual strains and buckling of mucosa. Proc Inst Mech Eng [H] 2007;221:417–426. doi: 10.1243/09544119JEIM47. [DOI] [PubMed] [Google Scholar]
- 52.Liao D, Fan Y, Zeng Y, Gregersen H. Stress distribution in the layered wall of the rat oesophagus. Med Eng Phys. 2003;25:731–738. doi: 10.1016/s1350-4533(03)00122-x. [DOI] [PubMed] [Google Scholar]
- 53.Liao D, Zhao J, Fan Y, Gregersen H. Two-layered quasi-3D finite element model of the oesophagus. Med Eng Phys. 2004;26:535–543. doi: 10.1016/j.medengphy.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 54.Yang W, Fung TC, Chian KS, Chong CK. Instability of the two-layered thick-walled esophageal model under the external pressure and circular outer boundary condition. J Biomech. 2007;40:481–490. doi: 10.1016/j.jbiomech.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 55.Gasser TC, Ogden RW, Holzapfel GA. Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J R Soc Interface. 2006;3:15–35. doi: 10.1098/rsif.2005.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holzapfel GA, Gasser TC, Ogden RW. Comparison of a multi-layer structural model for arterial walls with a fung-type model, and issues of material stability. J Biomech Eng. 2004;126:264–275. doi: 10.1115/1.1695572. [DOI] [PubMed] [Google Scholar]
- 57.Yang W, Fung TC, Chian KS, Chong CK. Directional, regional, and layer variations of mechanical properties of esophageal tissue and its interpretation using a structure-based constitutive model. J Biomech Eng. 2006;128:409–418. doi: 10.1115/1.2187033. [DOI] [PubMed] [Google Scholar]
- 58.Drewes AM, Arendt-Nielsen L, Funch-Jensen P, Gregersen H. Experimental human pain models in gastro-esophageal reflux disease and unexplained chest pain. World J Gastroenterol. 2006;12:2806–2817. doi: 10.3748/wjg.v12.i18.2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Drewes AM, Gregersen H. Multimodal pain stimulation of the gastrointestinal tract. World J Gastroenterol. 2006;12:2477–2486. doi: 10.3748/wjg.v12.i16.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gregersen H, Drewes AM, McMahon BP, Liao D. Balloon-distension studies in the gastrointestinal tract: current role. Dig Dis. 2006;24:286–296. doi: 10.1159/000092882. [DOI] [PubMed] [Google Scholar]
- 61.Gregersen H, Liao D, Pedersen J, Drewes AM. A new method for evaluation of intestinal muscle contraction properties: studies in normal subjects and in patients with systemic sclerosis. Neurogastroenterol Motil. 2007;19:11–19. doi: 10.1111/j.1365-2982.2006.00837.x. [DOI] [PubMed] [Google Scholar]
- 62.Pedersen J, Drewes AM, Gregersen H. New analysis for the study of the muscle function in the human oesophagus. Neurogastroenterol Motil. 2005;17:767–772. doi: 10.1111/j.1365-2982.2005.00652.x. [DOI] [PubMed] [Google Scholar]
- 63.Frokjaer JB, Andersen SD, Drewes AM, Gregersen H. Ultrasound-determined geometric and biomechanical properties of the human duodenum. Dig Dis Sci. 2006;51:1662–1669. doi: 10.1007/s10620-005-9015-y. [DOI] [PubMed] [Google Scholar]
- 64.Li M, Brasseur JG, Dodds WJ. Analyses of normal and abnormal esophageal transport using computer simulations. Am J Physiol. 1994;266:G525–G543. doi: 10.1152/ajpgi.1994.266.4.G525. [DOI] [PubMed] [Google Scholar]
- 65.Jeays AD, Lawford PV, Gillott R, Spencer P, Barber DC, Bardhan KD, Hose DR. Characterisation of the haemodynamics of the superior mesenteric artery. J Biomech. 2007;40:1916–1926. doi: 10.1016/j.jbiomech.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 66.Liao D, Gregersen H, Hausken T, Gilja OH, Mundt M, Kassab G. Analysis of surface geometry of the human stomach using real-time 3-D ultrasonography in vivo. Neurogastroenterol Motil. 2004;16:315–324. doi: 10.1111/j.1365-2982.2004.00522.x. [DOI] [PubMed] [Google Scholar]
- 67.McMahon BP, Frokjaer JB, Kunwald P, Liao D, Funch-Jensen P, Drewes AM, Gregersen H. The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol. 2007;292:G377–G384. doi: 10.1152/ajpgi.00311.2006. [DOI] [PubMed] [Google Scholar]
- 68.Nicosia MA, Brasseur JG, Liu JB, Miller LS. Local longitudinal muscle shortening of the human esophagus from high-frequency ultrasonography. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1022–G1033. doi: 10.1152/ajpgi.2001.281.4.G1022. [DOI] [PubMed] [Google Scholar]
- 69.Buist ML, Cheng LK, Sanders KM, Pullan AJ. Multiscale modelling of human gastric electric activity: can the electrogastrogram detect functional electrical uncoupling? Exp Physiol. 2006;91:383–390. doi: 10.1113/expphysiol.2005.031021. [DOI] [PubMed] [Google Scholar]
- 70.Buist ML, Cheng LK, Yassi R, Bradshaw LA, Richards WO, Pullan AJ. An anatomical model of the gastric system for producing bioelectric and biomagnetic fields. Physiol Meas. 2004;25:849–861. doi: 10.1088/0967-3334/25/4/006. [DOI] [PubMed] [Google Scholar]
- 71.Cheng LK, Komuro R, Austin TM, Buist ML, Pullan AJ. Anatomically realistic multiscale models of normal and abnormal gastrointestinal electrical activity. World J Gastroenterol. 2007;13:1378–1383. doi: 10.3748/wjg.v13.i9.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin AS, Buist ML, Cheng LK, Smith NP, Pullan AJ. Computational simulations of the human magneto- and electroenterogram. Ann Biomed Eng. 2006;34:1322–1331. doi: 10.1007/s10439-006-9142-4. [DOI] [PubMed] [Google Scholar]
- 73.Lin AS, Buist ML, Smith NP, Pullan AJ. Modelling slow wave activity in the small intestine. J Theor Biol. 2006;242:356–362. doi: 10.1016/j.jtbi.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 74.Pullan A, Cheng L, Yassi R, Buist M. Modelling gastrointestinal bioelectric activity. Prog Biophys Mol Biol. 2004;85:523–550. doi: 10.1016/j.pbiomolbio.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 75.Yassi R, Cheng LK, Al-Ali S, Smith NP, Pullan AJ, Windsor JA. An anatomically based mathematical model of the gastroesophageal junction. Conf Proc IEEE Eng Med Biol Soc. 2004;1:635–638. doi: 10.1109/IEMBS.2004.1403238. [DOI] [PubMed] [Google Scholar]
- 76.Brasseur JG, Nicosia MA, Pal A, Miller LS. Function of longitudinal vs circular muscle fibers in esophageal peristalsis, deduced with mathematical modeling. World J Gastroenterol. 2007;13:1335–1346. doi: 10.3748/wjg.v13.i9.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gao F, Liao D, Zhao J, Drewes AM, Gregersen H. Numerical analysis of pouch filling and emptying after laparoscopic gastric banding surgery. Obes Surg. 2008;18:243–250. doi: 10.1007/s11695-007-9314-9. [DOI] [PubMed] [Google Scholar]
- 78.Dillard S, Krishnan S, Udaykumar HS. Mechanics of flow and mixing at antroduodenal junction. World J Gastroenterol. 2007;13:1365–1371. doi: 10.3748/wjg.v13.i9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McMahon BP, Odie KD, Moloney KW, Gregersen H. Computation of flow through the oesophagogastric junction. World J Gastroenterol. 2007;13:1360–1364. doi: 10.3748/wjg.v13.i9.1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pal A, Brasseur JG, Abrahamsson B. A stomach road or "Magenstrasse" for gastric emptying. J Biomech. 2007;40:1202–1210. doi: 10.1016/j.jbiomech.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 81.Yang W, Fung TC, Chian KS, Chong CK. Finite element simulation of food transport through the esophageal body. World J Gastroenterol. 2007;13:1352–1359. doi: 10.3748/wjg.v13.i9.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]


