Abstract
Background
This study sought to investigate the effect of changes in depression status on physical disability in older persons receiving home care, examine whether the effect is due to concomitant changes in cognitive status, and test whether affective state and cognitive ability interact to influence physical disability.
Methods
Multilevel analyses were conducted using longitudinal data collected about every 3 months from older participants in Michigan's community-based long-term care programs (N = 13,129). The data set provided an average of nine repeated measures of depressive symptoms, cognitive functioning, and physical disability. We estimated the lag effects of within-person changes in depression and cognitive status, and their interaction, on physical disability measured by activities of daily living (ADL) and instrumental activities of daily living (IADL), controlling for health-related events that occurred in the interim.
Results
Changes between not having and having depressive symptoms, including subsyndromal symptoms, are critical to physical disability for home care elders. The effects are independent of concomitant changes in cognitive status, which also have significant adverse effects on physical disability. There is some evidence that improvement of depression buffers the adverse effect of cognitive decline on IADL disability.
Conclusions
Providers should monitor changes in depression and cognitive status in home care elders. Early detection and treatment of subthreshold depression, as well as efforts to prevent worsening of cognitive status in home care elders, may have a meaningful impact on their ability to live at home.
Keywords: Frail elderly, Depression, Cognitive impairment, Disability, Aging in place, Multilevel analysis
NUMEROUS population-based aging studies have reported that depression is disabling (1–4). There is suggestion, however, that the effect of depression on disability may be less salient in older adults who are already disabled. For example, Mehta and colleagues (5) found that depressive symptoms have no significant effect on functional decline after controlling for cognitive impairment among older persons with dependence in activities of daily living (ADL) at baseline, although both depressive symptoms and cognitive impairment are risk factors for functional decline among those with no ADL dependence. Research has shown that depressive symptoms and cognitive impairment occur concomitantly (6), that cognitive dysfunction is a common symptomatic manifestation of late-life depression (7), and that poor cognitive functioning is a major risk factor for physical decline (8). Hence, it is possible that the observed effects of depression on disability are due to cognitive deficits, particularly among home care elders who are vulnerable to both depression and cognitive impairment (9,10). There is also evidence that emotional health and cognitive ability interact to influence physical function; for instance, Raji and colleagues (11) found that low depressive symptoms buffer the adverse impact of low cognition on subsequent decline of lower body function among older Mexican Americans.
The purpose of this study is threefold. First, we investigate the effect of changes in depression status on physical disability among elderly persons receiving home care. Second, we examine whether such effect is independent of concomitant changes in cognitive status. Third, we test whether changes in depression and cognitive status interact to influence physical disability.
METHODS
Source of Data
This is a secondary data analysis based on data collected from a large cohort of elderly participants in two publicly funded home- and community-based long-term care programs in Michigan: Medicaid Waiver and Care Management. Participants of both programs must be eligible for nursing home care. An income limit (Medicaid eligible) applies to Waiver and an age limit (60 years or older) to Care Management clients. For care planning purposes, all program participants have to be assessed by case managers (social workers or nurses) at baseline and then every 3 months, using the same instrument (Minimum Data Set for Home Care [MDS-HC]). Assessments are conducted through home visits and based on all sources of information, including the participants, their caregivers and clinicians, and direct observations.
We followed the cohort who enrolled in either Waiver or Care Management between October 1998 and September 2003. They were observed till the end of 2003. We selected those who were 65 years or older, either black or white, and had been assessed at least three times during the observation period as the sample. We excluded those with severe cognitive impairment at baseline, defined as a score of 4 or more on the MDS cognitive performance scale (CPS; range = 0–6) (12). The final sample consisted of 13,129 respondents who had been assessed 8.5 times (range = 3–24) for a period of 23 months (range = 2–60) on average. At the end of the observation period, 19.2% of the sample had died and 10.3% were institutionalized. All sample members were included in multilevel analyses that can accommodate unbalanced designs.
Variables and Measures
Physical disability—indicated by ADL and instrumental activities of daily living (IADL). ADL was assessed by eight items (e.g., transferring, dressing, eating). Each was rated as 0 (independent), 1 (supervision), 2 (limited assistance), 3 (extensive assistance), or 4 (totally dependent). IADL included seven items (eg, preparing meals, managing finances, using the phone). Each was rated as 0 (no difficulty), 1 (some difficulty), or 2 (great difficulty). Scales of ADL (range = 0–32; α = .93) and IADL (range = 0–14; α = .80) were formed by summing their respective items; higher scores indicating more disability. Additionally, we formed dichotomous variables to distinguish “more dependent” from “less dependent” elders. ADL dependence status was coded 1—needs physical help (ratings of 2–4) in one or more ADLs—and 0—needs supervision only or independent (ratings of 0 and 1) in all ADLs. IADL dependence status was coded 1—has difficulty (ratings of 1 and 2) in all IADLs—and 0—independent in one or more IADLs.
Depressive symptoms—measured by six items (eg, recurring crying and tearfulness, a feeling of sadness or being depressed, withdrawal from activities of interest) adapted from the MDS depression rating scale (DRS). Each item was rated from 0 (not exhibited in the past 30 days) to 2 (exhibited daily). The scale score was formed by summing all items (range = 0–12; α = .74). The DRS has been validated against the Hamilton Depression Rating Scale (13) and the Cornell Scale for Depression in Dementia (14). A DRS score of 3 or more indicates probable depression, and has demonstrated excellent sensitivity (.91) and acceptable specificity (.69) compared with psychiatric diagnosis based on the Diagnostic and Statistical Manual of Mental Disorders IV criteria (15). We classified depression status into three categories: no depression (DRS score = 0), subthreshold depression (DRS score = 1 or 2), and probable depression (DRS score ≥3).
Cognitive functioning—measured by the MDS CPS (12), which has been validated against the Mini-Mental State Examination (16) and the Test for Severe Impairment (17). The CPS ranges from 0 to 6 (α = .71), with 0 and 1 representing intact and borderline intact cognition, and 2–6 representing mild to very severe cognitive impairment. A cut point at 2 or greater had a sensitivity between .82 and .93 and specificity between .88 and .95 when compared with nurse assessors’ judgment of residents’ orientation status (12). We classified cognitive status into three categories: cognitively intact (CPS = 0), borderline (CPS = 1), and impaired (CPS ≥ 2).
Falls, acute episodes, and flare-up of chronic conditions that occurred between assessment occasions may influence changes in depression, cognition, and disability. Each of these health-related events was coded dichotomously (yes vs no) and controlled in the analyses. We also adjusted for the effect of time, measured as number of years since baseline.
Data Analysis
We conducted multilevel analyses with repeated measures at level 1 and individuals at level 2 using the HLM software (18). To reduce temporal ambiguity, the depression status and cognitive status at each assessment were used to predict the outcomes (ADL and IADL disability) at the next follow-up. These time-varying predictors were centered at individual's group mean (ie, raw values minus mean values across all measurement occasions), whereas individual's mean depression status and cognitive status were used as time-fixed covariates. In this way, the effects of within-person and between-person variations were decomposed (19); the former was our substantive interest. The interaction effects of change in depression and cognitive status on physical disability were tested by entering their product terms as time-varying predictors. We ran two sets of parallel analyses, with the outcomes (ADL and IADL disability) measured as continuous and dichotomous variables, respectively. Hierarchical linear models were used to estimate continuous outcomes and Bernoulli hierarchical generalized linear models for dichotomous outcomes (19). Significance level was set at p less than .05.
Most study variables had missing data. The percentage of missing was highest at baseline and decreased thereafter. For example, depressive symptoms had 9.7% missing at baseline, the highest of all, but only 0.5% missing at the third assessment. We undertook multiple imputation for study variables missing at baseline, using the NORM program (20). Then, we used the lag values to replace missing variables at the following assessment. Three imputed data sets were analyzed. The final estimates and standard errors (SEs) combined results from the three analyses (21).
RESULTS
Characteristics of the Sample
Baseline sample characteristics are presented in Table 1. Most respondents were middle-old individuals with multiple chronic conditions. About 73% needed physical help in one or more ADLs and 35% had difficulty in all IADLs. About 47% had no depression, 30% had subthreshold depression, and 23% had probable depression. Approximately, 43% were cognitively intact, 23% were borderline intact, and 34% had mild to moderate impairment.
Table 1.
Sample Characteristics at Baseline (N = 13,129)
| % or Mean (SD) | |
| Age (y) | 78.86 (7.52) |
| Race | |
| Black | 18.29 |
| White | 81.71 |
| Gender | |
| Male | 26.29 |
| Female | 73.71 |
| Education | |
| Less than high school | 53.90 |
| High school | 29.22 |
| More than high school | 16.88 |
| Marital status | |
| Married | 29.61 |
| Widowed | 55.66 |
| Separated/divorced | 11.29 |
| Never married | 3.44 |
| Living arrangements | |
| Alone | 44.78 |
| With spouse | 28.04 |
| With others | 27.18 |
| Program type | |
| Waiver | 52.44 |
| Care management | 47.55 |
| No. of chronic conditions | 5.23 (2.39) |
| ADL scale score | 7.34 (6.83) |
| ADL dependence status | |
| Need physical help in 1+ ADLs | 72.65 |
| Independent or need supervision only in all ADLs | 27.35 |
| IADL scale score | 9.86 (2.96) |
| IADL dependence status | |
| Have difficulty in all IADLs | 34.96 |
| Independent in 1+ IADLs | 65.04 |
| Depression status | |
| No depression | 47.06 |
| Subthreshold depression | 29.92 |
| Probable depression | 23.02 |
| Cognitive status | |
| Intact | 43.47 |
| Borderline intact | 22.96 |
| Impaired | 33.57 |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
The sample had substantial changes in physical disability, depression, and cognitive status during the observation period (Table 2). In terms of physical disability, about 62% had changes in ADL score, 19% in ADL dependence status, 43% in IADL score, and 10% in IADL dependence status. Regarding depression and cognitive status, about 48% and 29%, respectively, experienced changes. The changes were in all directions; some respondents had improvement only, some only decline, and some experienced both improvement and decline over time.
Table 2.
Within-Person Changes in Physical Disability, Depression, and Cognitive Status in the Sample During the Observation Period
| N (%) Experienced Positive Changes (improvement) Only | N (%) Experienced Negative Changes (decline) Only | N (%) Experienced Both Positive and Negative Changes | |
| ADL scale score | 1711 (13.03) | 3596 (27.39) | 2792 (21.26) |
| ADL dependence status | 595 (4.53) | 1216 (9.26) | 687 (5.23) |
| IADL scale score | 1342 (10.22) | 2939 (22.38) | 1332 (10.15) |
| IADL dependence status | 392 (2.99) | 810 (6.17) | 134 (1.02) |
| Depression status | 2593 (19.75) | 1205 (9.18) | 2522 (19.22) |
| Cognitive status | 805 (6.13) | 2049 (15.60) | 939 (7.15) |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
Effects of Changes in Depression and Cognitive Status on ADL Disability
The multilevel analysis of ADL disability shows that a change from subthreshold to no depression is associated with a decrease of .104 point (SE = .033, p = .001) in ADL score and a 14% reduction in the likelihood of needing physical help in ADLs (vs needing supervision only or independent) (odds ratio [OR] = .859, 95% confidence interval [CI] = .767–.962, p = .009) at the next assessment (Table 3, model 1). A change from subthreshold to probable depression does not have significant effects on ADL disability measured either continuously or dichotomously. The estimates did not change substantively when adjusting for concomitant changes in cognitive status (beta for ADL score = −.097, SE = .033, p = .003; OR for needing physical help in ADLs = .875, 95% CI = .782–.980, p = .021; Table 3, model 2), suggesting that the effects of depression on ADL disability are independent of cognitive functioning.
Table 3.
Effects of Within-Person Changes in Depression and Cognitive Status on Subsequent ADL Disability
| ADL Scale Score |
Need Physical Help in 1+ ADLs (vs independent or need supervision only in all ADLs) |
|||||||
| Model 1 |
Model 2 |
Model 1 |
Model 2 |
|||||
| b (SE) | p | b (SE) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Fall | .134 (.019) | <.0001 | .134 (.019) | <.0001 | 1.277 (1.194–1.365) | <.0001 | 1.274 (1.191–1.362) | <.0001 |
| Acute episode | .247 (.041) | <.0001 | .245 (.041) | <.0001 | 1.433 (1.048–1.960) | .0241 | 1.432 (1.045–1.963) | .0254 |
| Flare-up of chronic conditions | .209 (.047) | <.0001 | .210 (.047) | <.0001 | 1.272 (1.100–1.471) | .0012 | 1.264 (1.094–1.460) | .0015 |
| Depression status (omitted: subthreshold depression) | ||||||||
| No depression | –.104 (.033) | .0014 | –.097 (.033) | .0031 | .859 (.767–.962) | .0085 | .875 (.782–.980) | .0206 |
| Probable depression | .070 (.041) | .0879 | .062 (.041) | .1285 | .981 (.847–1.136) | .7995 | .961 (.832–1.111) | .5920 |
| Cognitive status (omitted: borderline intact) | ||||||||
| Intact | — | –.059 (.045) | .1919 | — | .745 (.612–.906) | .0032 | ||
| Impaired | — | .251 (.051) | <.0001 | — | 1.281 (1.040–1.577) | .0197 | ||
Note: All models controlled for time (a quadratic term for ADL scale and a linear term for ADL dependence status), and individual's mean depression and cognitive status. ADL = activities of daily living; OR = odds ratio; CI = confidence interval.
Cognitive status significantly predicts ADL disability. A deterioration from borderline intact to impaired cognition is associated with an increment of .251 point (SE = .051, p < .001) in ADL score and a 28% increase in the odds of needing physical help in ADLs (OR = 1.281, 95% CI = 1.040–1.577, p = .020). An improvement from borderline to intact cognition reduces the odds of needing physical help in ADLs by 26% (OR = .745, 95% CI = .612–.906, p = .003) but has no significant effect on ADL score. No significant interaction of depression and cognitive status was detected.
Effects of Within-Person Changes in Depression and Cognitive Status on IADL Disability
Regarding IADL disability (Table 4), an improvement from subthreshold to no depression is significantly associated with a subsequent decrease in IADL score both before (beta = −.040, SE = .011, p < .001) and after (beta = −.036, SE = .011, p = .002) adjusting for cognitive status. It also reduces the likelihood of having difficulty in all IADLs (vs independent in one or more IADLs) by 18% (OR = .821, 95% CI = .725–.930, p = .002) before and 13% (OR = .874, 95% CI = .771-.991, p = .035) after controlling for cognitive status. Changes between subthreshold and probable depression do not have significant effects on subsequent IADL disability.
Table 4.
Effects of Within-Person Changes in Depression and Cognitive Status on Subsequent IADL Disability
| IADL Scale Score |
Difficulty in All IADLs (vs independent in 1+ IADLs) |
|||||||||
| Model 1 |
Model 2 |
Model 3 |
Model 1 |
Model 2 |
||||||
| b (SE) | p | b (SE) | p | b (SE) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Fall | .034 (.007) | <.0001 | .034 (.007) | <.0001 | .034 (.007) | <.0001 | 1.175 (1.096–1.260) | <.0001 | 1.174 (1.095–1.258) | <.0001 |
| Acute episode | .074 (.014) | <.0001 | .073 (.014) | <.0001 | .072 (.014) | <.0001 | 1.267 (1.048–1.532) | .0144 | 1.246 (1.034–1.502) | .0212 |
| Flare-up of chronic conditions | .080 (.017) | <.0001 | .080 (.017) | <.0001 | .080 (.017) | <.0001 | 1.082 (.919–1.275) | .3436 | 1.083 (.921–1.273) | .3330 |
| Depression status (omitted: subthreshold depression) | ||||||||||
| No depression | –.040 (.011) | .0005 | –.036 (.011) | .0015 | –.037 (.011) | .0011 | .821 (.725–.930) | .0019 | .874 (.771–.991) | .0353 |
| Probable depression | .022 (.017) | .1988 | .018 (.017) | .2842 | .016 (.017) | .3457 | 1.064 (.894–1.266) | .4871 | 1.005 (.851–1.187) | .9498 |
| Cognitive status (omitted: borderline intact) | ||||||||||
| Intact | — | –.054 (.019) | .0054 | –.055 (.019) | .0047 | — | .557 (.444–.698) | <.0001 | ||
| Impaired | — | .099 (.020) | <.0001 | .097 (.020) | <.0001 | — | 2.147 (1.740–2.650) | <.0001 | ||
| Depression × Cognitive Status | ||||||||||
| No Depression × Intact | –.079 (.062) | .2002 | ||||||||
| No Depression × Impaired | –.147 (.055) | .0073 | ||||||||
| Probable Depression × Intact | –.150 (.073) | .0401 | ||||||||
| Probable Depression × Impaired | –.011 (.068) | .8705 | ||||||||
Note: All models controlled for time (a quadratic term for IADL scale and a linear term for IADL dependence status), and individual's mean depression and cognitive status. IADL = instrumental activities of daily living; OR = odds ratio; CI = confidence interval.
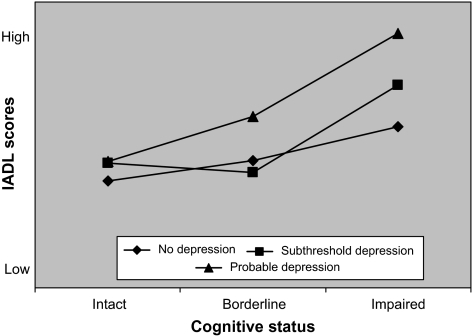
Cognitive status has strong effects on IADL disability. A decline from borderline intact to impairment doubles the odds of having difficulty in all IADLs (OR = 2.147, 95% CI = 1.740–2.650, p < .001) and predicts .099 point (SE = .020, p < .001) increase in IADL score at the following assessment. An improvement from borderline to cognitively intact status, in contrast, is associated with a 54% reduction (OR = .557, 95% CI = .444, .698, p < .001) in the likelihood of having difficulty in all IADLs and a reduction of .054 point (SE =.019, p=.005) in IADL score. The interaction of depression and cognitive status on IADL scale score is statistically significant (Table 4, model 3). Figure 1 depicts the effects, which suggests that a decline of cognitive status is associated with more elevated IADL scores when depression status worsens.
Figure 1.
Interaction effect of depression and cognitive status on instrumental activities of daily living (IADL) scores.
DISCUSSION
This analysis shows that worsening of depression and cognitive status independently predicts a subsequent increase in ADL and IADL score (more disability) and an increased likelihood of dependency in both domains of functioning among home care elders. Transitions between no and subthreshold depression and between borderline intact and impaired cognition are particularly important to their change in physical disability. There is some evidence that improvement of depression buffers the adverse effects of cognitive decline on IADL score. The findings here should be an impetus for more focused inquiry in frail elderly persons using the MDS-HC as well as other measures of depression, cognition, and physical disability.
This study has several methodological strengths that help to provide a rigorous test of the effects of depressive symptoms on physical disability. Repeated assessments enable within-person analysis and the use of lag variables as predictors, resolving temporal ambiguity when examining the association of changes in depression status and changes in physical disability. Also, with this approach each individual acts as his or her own control, reducing potential for selection bias associated with differences between individuals. Health-related events that occurred within individuals between assessments were controlled however. Finally, all data were collected by case managers based on information from multiple sources, reducing potential measurement errors due to self-report (e.g., the influence of depression on assessment of disability) (22).
The mechanisms by which depression has an effect on physical disability are not completely understood. Both behavioral (depressed patients may have poor lifestyle, such as nonadherence to medical and self-care regiments) and biological mechanisms (depression may worsen medical diseases through changes in hypothalamic-pituitary-adrenal axis and the sympathetic nervous and immunological system) have been proposed (23). Each could lead to more disability.
This study has limitations as well. First, the sample's representativeness may be limited. It may overrepresent community-living frail elders with low incomes—a vulnerable, difficult-to-access, and understudied population. Second, the MDS measures of depressive symptoms and cognitive functioning have not been widely used; particularly, their performance over time is unknown. We examined the DRS and CPS across nine waves of assessment and found that their internal consistency reliabilities, and correlations with each other and with ADL and IADL scales, are quite consistent across waves. Both DRS and CPS also show statistically significant change over time. The DRS has been validated against the Cornell Scale for Depression in Dementia (14), which is a measure of depression targeting people with dementia; nonetheless, evaluating depression in patients with dementia is an issue that needs further study.
Our findings suggest that the emergence of any depressive symptoms in nondepressed frail elders, including subsyndromal clinical states, should be evaluated and treatment should be considered. In home care elders, elimination of subthreshold depression reduces the odds of needing physical help in ADLs and the odds of having difficulty in all IADLs by 13%, whereas the onset of subsyndromal symptoms increases their odds by 16% and 15%, respectively. Moreover, it is necessary to monitor frail elderly persons’ cognitive performance. Great efforts should be made to help those who are borderline intact to maintain or improve their cognitive ability. In the case that a downward trajectory toward cognitive impairment is obvious, helping patients to prepare for possible physical deterioration such as modifying the home environment, may be needed. From a public health perspective, early detection and treatment of depression, including subsyndromal symptoms, as well as efforts to prevent cognitive decline in home care elders may have a meaningful impact on their ability to live at home and thus on controlling health care costs.
Acknowledgments
An earlier version of this paper was presented at the 60th annual meeting of the Gerontological Society of America in San Francisco, CA. L.W.L. was supported by the University of Michigan Claude D. Pepper Older Americans Independence Center with a grant from the National Institute of Aging (AG024824). Y.C. received support from the National Institute of Mental Health (P20 MH071897 and R24 MH07164). The authors thank the Michigan Department of Community Health and Mary James, Brant Fries, and Kristina Szafara for their assistance in accessing the data; Deborah Bybee and Brady West for statistical consultations; and Tanya Emley for editorial assistance.
References
- 1.Beekman AT, Penninx BW, Deeg DJ, de Beurs E, Geerlings SW, van Tilburg W. The impact of depression on the well-being, disability and use of services in older adults: a longitudinal perspective. Acta Psychiatr Scand. 2002;105:20–27. doi: 10.1034/j.1600-0447.2002.10078.x. [DOI] [PubMed] [Google Scholar]
- 2.Cronin-Stubbs D, de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Arch Intern Med. 2000;160:3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- 3.Lenze EJ, Schulz R, Martire LM, et al. The course of functional decline in older people with persistently elevated depressive symptoms. J Am Geriatr Soc. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- 4.Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the Established Populations for Epidemiologic Studies of the Elderly. Am J Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta KM, Yaffe K, Covinsky KE. Cognitive impairment, depressive symptoms, and functional decline in older people. J Am Geriatr Soc. 2002;50:1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Han L, McCusker J, Abrahamowicz M, Cole M, Capek R. The temporal relationship between depression symptoms and cognitive functioning in older medical patients—prospective or concurrent? J Gerontol Med Sci. 2006;61A:M1319–M1323. doi: 10.1093/gerona/61.12.1319. [DOI] [PubMed] [Google Scholar]
- 7.Reifler BV. Detection and treatment of mixed cognitive and affective symptoms in the elderly: is it dementia, depression, or both? Clin Geriatr. 1998;6:17–33. [Google Scholar]
- 8.Greiner PA, Snowdon DA, Schmitt FA. The loss of independence in activities of daily living: the role of low cognitive function in elderly nuns. Am J Public Health. 1996;86:62–66. doi: 10.2105/ajph.86.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong-Esther C, Hagen B, Sandilands M, Williams R, Smith C. A longitudinal study of home care clients and their informal carers. Br J Community Nurs. 2005;10:284–291. doi: 10.12968/bjcn.2005.10.6.18169. [DOI] [PubMed] [Google Scholar]
- 11.Raji MA, Ostir GV, Markides KS, Goodwin JS. The interaction of cognitive and emotional status on subsequent physical functioning in older Mexican Americans: findings from the Hispanic Established Population for the Epidemiologic Study of the Elderly. J Gerontol Med Sci. 2002;57A:M678–M682. doi: 10.1093/gerona/57.10.m678. [DOI] [PubMed] [Google Scholar]
- 12.Morris J, Fries B, Mehr D, Hawes C, Phillips C. MDS cognitive performance scale. J Gerontol Med Sci. 1994;49:M174–M182. doi: 10.1093/geronj/49.4.m174. [DOI] [PubMed] [Google Scholar]
- 13.Burrows AB, Morris JN, Simon SE, Hirdes JP, Phillips C. Development of a minimum data set-based depression rating scale for use in nursing homes. Age Aging. 2000;29:165–172. doi: 10.1093/ageing/29.2.165. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 15.Alexopoulos GS, Abrams RC, Young RC, et al. Cornell scale for depression in dementia. Biol Psychiatry. 1988;23:271–284. doi: 10.1016/0006-3223(88)90038-8. [DOI] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 17.Albert M, Cohen C. The test for severe impairment: an instrument for the assessment of patients with severe cognitive dysfunction. J Am Geriatr Soc. 1992;40:449–453. doi: 10.1111/j.1532-5415.1992.tb02009.x. [DOI] [PubMed] [Google Scholar]
- 18.Raudenbush S, Bryk A, Congdon R. HLM6.04 [software] Chicago, IL: Scientific Software International; 2007. [Google Scholar]
- 19.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 20.Schafer J. NORM: Multiple Imputation of Incomplete Multivariate Data Under a Normal Model [computer software] Pennsylvania State University Department of Statistics: University Park; 1999. [Google Scholar]
- 21.Schafer J, Olsen M. Multiple imputation for multivariate missing-data problems: a data analyst's perspective. Multivariate Beh Res. 1998;33:545–571. doi: 10.1207/s15327906mbr3304_5. [DOI] [PubMed] [Google Scholar]
- 22.Bruce M. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry. 2001;9:102–112. [PubMed] [Google Scholar]
- 23.Katon WJ, Lin E, Russo J, Unutzer J. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]