Abstract
Background
Helicopters and light (unpressurised) aircraft are used increasingly for the transport of ventilated patients. Most of these patients are ventilated through endotracheal tubes (ETTs), others through laryngeal mask airways (LMAs). The cuffs of both ETTs and LMAs inflate with increases in altitude as barometric pressure decreases (30 mbar/1000 feet).
Tracheal mucosa perfusion becomes compromised at a pressure of approximately 30 cm H2O; critical perfusion pressure is 50 cm H2O.
Methods
The change in dimensions of the inflated cuffs of a size 8 ETT and a size 5 LMA were measured with digital callipers at 1000 feet intervals in the unpressurised cabin of an Agusta 109 helicopter used by the Warwickshire and Northamptonshire Air Ambulance.
Results
A linear expansion in cuff dimensions as a function of altitude increase was identified. For ETTs, a formula for removal of air from the cuff with increasing altitude was calculated and is recommended for use in aeromedical transfers. This is 1/17×1.1 = 0.06 ml/1000 foot ascent/ml initial cuff inflation.
Conclusion
The data for LMA cuff expansion failed to show significant correlation with altitude change. Further work is required to determine a similar rule of thumb for LMA cuff deflation.
Transport of ventilated critically ill patients by helicopter and light (unpressurised) aircraft has become well established in recent years. Many of these patients are ventilated through a cuffed endotracheal tube (ETT), which is inflated before flight. Some emergency patients might be ventilated through laryngeal mask airways (LMAs) in the event of failure to secure a definitive airway in the field. The cuffs of ETTs and LMAs expand with increasing altitude owing to decreasing barometric pressure at a rate of approximately 30 mbar/1000 feet.
Intubated patients are at risk of tracheal damage owing to the expansion of endotracheal tube cuffs.1,2 Tracheal mucosa has a critical perfusion pressure of 50 cm H2O, but perfusion becomes compromised at pressures of around 30 cm H2O.3 The sequelae of mucosal ischaemia vary in severity as a function of the amount of pressure applied to the mucosa and the duration of ischaemia. These include hoarseness, dysphasia, laryngeal incoordination, oedema, tracheal stenosis and tracheal rupture.1
Both in vivo2 and in vitro4 studies have shown that the tracheal critical perfusion pressure is exceeded between 1820 and 3000 feet altitude in uncompensated endotracheal cuff inflation, making it important to control for cuff‐volume expansion in aeromedical transport. No difference has been found in the cuff pressures of size 8 and size 9 endotracheal tubes at altitude.
In normal clinical situations, avoidance of tracheal ischaemia is achieved by inflating the cuff to the point at which no leakage is heard on positive pressure ventilation; this may be repeated if necessary (eg, if the clinician suspects cuff expansion owing to diffusion of nitrous oxide). However, in helicopters and light aircraft, noise levels are too high to make this possible and correction of high cuff pressures must be achieved by other means.
Current advice for the aeromedical transport of intubated patients includes inflation of the cuff with saline, use of an external balloon into which a valve leaks air at higher pressures or deflation of the ETT cuff at altitude. However, Smith and McArdle4 reported that saline was impractical for clinical use as they were unable to evacuate all air from the cuff and it took considerably longer to inflate and secure the ETT because of the fine bore tubing used in ETTs. Although at least one ETT with a pressure regulation mechanism (Brandt Tracheal tube, Tyco Healthcare, Hampshire, UK) is available in the UK, this device is currently not in widespread use in aeromedical transport.
We sought to determine how much air should be evacuated from an ETT cuff per 1000 feet of altitude to prevent excess pressure on the tracheal mucosa.
LMAs are a useful airway management device in the patient with a difficult airway, and are used at times in the aeromedical transport of critically ill emergency patients.5 LMAs are known to cause ischaemic complications similar to ETTs.6 Excess pressure from LMA cuffs has been implicated in pressure ischaemia of the tongue and oropharynx. LMA cuffs are inflated to the point at which the device begins to advance forwards from the mouth. We sought to determine the change in LMA cuff size with increasing altitude. We have found no previous data in this area.
Method
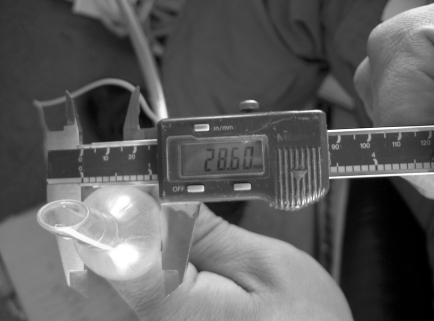
A size 8 ETT was inflated with 17 ml air at ground level to firmly inflate the cuff. Reference points for measurement were marked on the ETT cuff and the diameter was measured using digital callipers. The cuff dimensions were re‐measured using digital callipers every 1000 feet up to a maximum altitude of 10 000 feet inside a non‐pressurised Agusta 109 helicopter, used by the Warwickshire and Northamptonshire Air Ambulance (fig 1).
Figure 1 ETT cuff measurement with digital callipers.
At the end of the flight, all the air was removed to fully deflate the cuff. The volume was measured to ensure that no leaks had occurred. The cuff was then re‐inflated to the dimensions measured at altitude to determine the volume of excess gas in the cuff. Air temperature was recorded at ground level and at 10 000 feet.
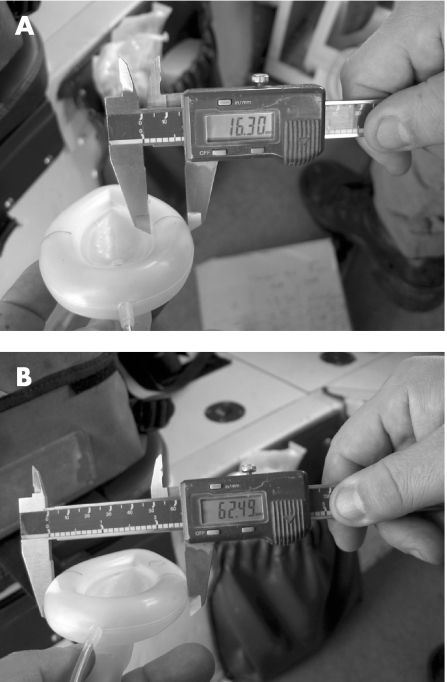
A size 5 LMA was inflated with 40 ml air (as per the manufacturer's instructions). Reference points were marked on the cuff. The cuff diameter and transverse diameter were measured at 1000 feet intervals during the same flight (fig 2).
Figure 2 Cuff diameter and transverse diameter measured using digital callipers.
As air acts as an ideal gas, according to Boyle's law, we can assume that volume and pressure in the cuff are directly proportional (P1V1 = P2V2). Therefore, measuring volumetric expansion of a freely suspended ETT/LMA is directly related to the increase in pressure in the cuff at altitude when inside the trachea.
Results
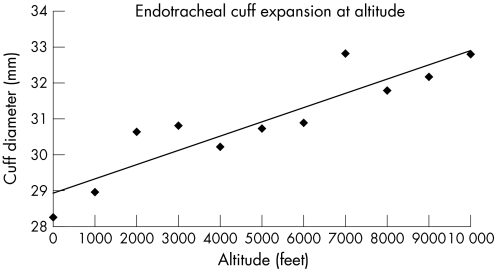
Figure 3 presents the changes in ETT cuff volume with increasing altitude. The diameter of the ETT cuff increased by 4.54 mm at 10 000 feet. At the end of the flight, 11 ml of additional air was required to re‐inflate the cuff to its maximum diameter that was measured at 10 000 feet. There was a strongly correlated linear expansion of the cuff at altitude (Pearson's r = 0.908, p<0.005).
Figure 3 Endotracheal cuff expansion with increasing altitude.
The LMA cuff diameter also expanded at altitude, although this was less significant than that demonstrated with the ETT (Pearson's r = 0.666, p<0.05). There was no significant relationship between the LMA cuff width and altitude (Pearson's r = 0.441, p>0.05).
During the experiment, the outside air temperature was recorded to drop by 12oC between ground level and 10 000 feet. (This is less than the expected 21°C and represents the local weather conditions on the day of the flight.)
Discussion
There was a significant, linear expansion of the ETT cuff with increasing altitude. Although LMA cuff size showed a trend towards expansion with increasing altitude, this was not statistically significant.
We know from previous studies that the critical perfusion pressure of the tracheal mucosa is exceeded above an altitude of 1820 feet.2,4 It is therefore important to control for ETT cuff expansion to prevent tracheal mucosal damage. We have devised a simple rule of thumb for calculating the volume of air to be removed from an ETT cuff, when travelling in noisy aircraft.
The ETT cuff was inflated with 17 ml air at ground level and expanded by 11 ml at 10 000 feet. An ETT cuff would normally be inflated with 5–10 ml air in vivo.
Knowing this, it is possible to calculate the following rule of thumb for deflation of an ETT cuff with rising altitude:
1/17×1.1 = 0.06 ml/1000 foot ascent/ml initial cuff inflation.
For example, a cuff inflated with 5 ml air at ground level should have 0.3 ml removed/1000 foot ascent to control for rising pressure with altitude.
The cuff should be re‐inflated with the same amount of air on descent to avoid air leakage.
As ETT cuffs are never inflated to maximum capacity when used in vivo, this rule of thumb is appropriate for use with all ETTs regardless of size or manufacturer.
Although we found that the LMA also expanded with rising altitude, it was not possible to relate this volumetric expansion to cuff pressure. However, we can conclude that there is a risk of mucosal ischaemia when using LMAs during aeromedical transport and this warrants further study.
During this study, ETT and LMA cuffs were measured in free suspension.
However, in vivo, the air in the cuff would be warmed to some extent by the surrounding tissues. Therefore, our measurements may have slightly underestimated the degree of cuff expansion in vivo owing to the temperature–volume relationship (Charles' law: V1/T1 = V2/T2). This would theoretically introduce an error <0.01 ml/1000 foot ascent/ml inflation (air temperature drops by approximately 2.1°C/1000 feet ascent).
During this experiment, the temperature drop with altitude was less than predicted for standard atmospheric conditions (12°C rather than 21°C). This would further reduce any in vitro error introduced by changes in cabin temperature with changes in altitude.
Abbreviations
ETT - endotracheal tube
LMA - laryngeal mask airway
Footnotes
Competing interests: None declared.
References
- 1.Crawley B E, Cross B D. Tracheal cuffs: a review and dynamic pressure study. Anaesthesia 198658111–116. [DOI] [PubMed] [Google Scholar]
- 2.Henning J, Sharley P, Young R. Pressures within air‐filled tracheal cuffs at altitude—an in vivo study. Anaesthesia 200459252–254. [DOI] [PubMed] [Google Scholar]
- 3.Seeglobin R D, Van Hasselt G L. Endotracheal cuff pressure and mucosal blood flow: endoscopic study of four large volume cuffs. BMJ 1984288965–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith R P R, McArdle B H. Pressure in the cuffs of tracheal tubes at altitude. Anaesthesia 200257374–378. [DOI] [PubMed] [Google Scholar]
- 5.Martin S E, Ochsner M G, Jarman R H.et al Use of the laryngeal mask airway in air transport when intubation fails. J Trauma‐Inj Infect Crit Care 199947352–357. [DOI] [PubMed] [Google Scholar]
- 6.Asai T, Brimacombe J. Cuff volume and size selection with the laryngeal mask. Anaesthesia 2000551179–1184. [DOI] [PubMed] [Google Scholar]