Abstract
Objectives
To establish the accuracy of the emergency medical dispatcher's (EMD's) decisions to override the automated Medical Priority Dispatch System (MPDS) logic‐based response code recommendations based on at‐scene paramedic‐applied transport acuity determinations (blue‐in) and cardiac arrest (CA) findings.
Methods
A retrospective study of a 1 year dataset from the London Ambulance Service (LAS) National Health Service (NHS) Trust was undertaken. We compared all LAS “bluing in” frequency (BIQ) and cardiac arrest quotient (CAQ) outcomes of the incidents automatically recommended and accepted as CHARLIE‐level codes, to those receiving EMD DELTA‐overrides from the auto‐recommended CHARLIE‐level. We also compared the recommended DELTA‐level outcomes to those in the higher ECHO‐override cases.
Results
There was no significant association between outcome (CA/Blue‐in) and the determinant codes (DELTA‐override and CHARLIE‐level) for both CA (odds ratio (OR) 0, 95% confidence interval (CI) 0 to 41.14; p = 1.000) and Blue‐in categories (OR 0.89, 95% CI 0.34 to 2.33; p = 1.000). Similar patterns were observed between outcome and all DELTA‐level and ECHO‐override codes for both CA (OR 0, 95% CI 0 to 70.05; p = 1.000) and Blue‐in categories (OR 1.17, 95% CI 0 to 7.12; p = 0.597).
Conclusion
This study contradicts the belief that EMDs can accurately perceive when a patient or situation requires more resources than the MPDS's structured interrogation process logically indicates. This further strengthens the concept that automated, protocol‐based call taking is more accurate and consistent than the subjective, anecdotal or experience‐based determinations made by individual EMDs.
“When in doubt, send ‘em out” is a legendary emergency dispatch rule that states an obvious clinical ethic, central to longstanding medical practice in general. This rule has been further defined in 911/999/000 dispatcher practice as “Always err in the direction of patient safety”. Applied at dispatch, this rule gives the emergency medical dispatcher (EMD) the discretion to override any logic‐based, response‐based code in a protocol system to a higher level. EMDs have been given this safety valve as an option when a priority dispatch protocol's logic‐recommended response code appears to be too “low” (insufficient for patient care reasons) to the interrogating EMD. The EMD can then “override” the recommended code to the next highest level.
Anecdotally, it has long been believed that the sum total of acquired dispatch information, coupled with the call taker's previous training and experience may, at times, suggest that the patient's condition warrants a faster or more advanced response than the protocol's structured coding logic has recommended. Until recently, the ability to assess the validity of these subjective choices has not been possible due to incomplete data associations. However, newly acquired, large datasets from high protocol compliance communication centres that associate patient acuity and cardiac arrest encounter data with individual dispatch determinant codes now allows for the evaluation of many longstanding, but to date unproven, dispatch‐related practices. These data associations have enabled this evaluation of the actual use of EMD overrides in a large, metropolitan setting.
Null hypothesis
Subjective EMD decisions to override the automated Medical Priority Dispatch System's (MPDS's) logic‐based response code recommendations are not supported by on‐scene paramedic decisions to transport with lights‐and‐siren or cardiac arrest encounters.
Methods and materials
The London Ambulance Service (LAS) Trust Control Centre provided the International Academies of Emergency Dispatch (IAED) with a dataset of 1 137 873 calls representing 758 695 incidents and 599 107 patients covering a 1 year period from 1 September 2005 to 31 August 2006. LAS uses the automated, computer software version of the Advanced MPDS Omega Protocol (v11.2 UKE‐NHO) (ProQA). LAS is an IAED‐accredited centre1 which requires compliance to protocol interrogation and coding accuracy above 90%. The LAS overall average compliance level during study period was 98.5%.2 This ensures that evaluation and coding findings are consistently the direct result of the protocol's internal structure.3
This dataset contains a subjective, patient acuity decision made by the ambulance crew resulting in a hospital notification “pre‐alert” referred to in the UK as “bluing in”—a reference to initiating a blue‐lights‐and‐siren transport of a critical patient.4,5 In addition, the integrated, computerised data system of the LAS records whether a cardiac arrest was encountered by the arriving crews or whether the patient arrested before arrival at the accident and emergency department. These findings are represented by the percentage of cardiac arrest (CA) encountered versus the number of incidents in each MPDS determinant code. We have previously coined the terms BIQ (blue‐in percentage quotient) and CAQ (cardiac arrest percentage quotient) as standard dispatch code outcome parameters.6
In the automated version of the MPDS (ProQA), the option of overriding the recommended dispatch response‐based code is currently allowed and easily performed by the interrogating EMD. Underriding the code to a lower level has never been allowed as a risk management and liability prevention measure. Every override is captured in the ProQA system's coding records for review.
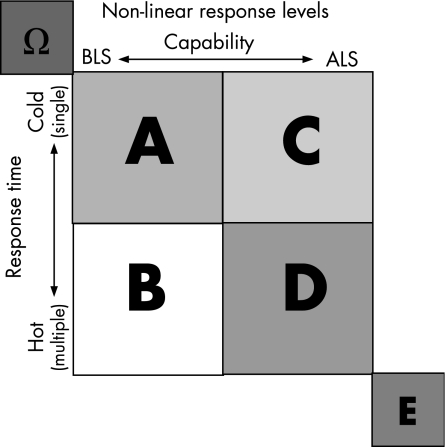
We compared all LAS BIQ and CAQ outcomes of the incidents automatically recommended and accepted (non‐overridden) as CHARLIE level codes, to those of incidents receiving EMD DELTA overrides from the auto‐recommended CHARLIE level. We also compared the recommended DELTA level code‐linked outcomes to those in the higher ECHO override cases. The conceptually designed value of these codes, independent of the local responses that are assigned to each code, is shown in fig 1.
Figure 1 Response determinant methodology.7
Intercooled Stata for Windows software (Stata Statistical Software: Release 9, StataCorp, College Station, Texas, USA) was used in all analyses. To perform a comparison of all protocol determinant code “C” (CHARLIE‐level) vs override code “D‐0” (DELTA override), and all code “D” (DELTA level) vs override code “E‐0” (ECHO override), we constructed 2‐by‐2 contingency tables of these codes, stratifying by outcome (that is, CA and Blue‐in). Fisher's exact p values and odds ratios (OR) with 95% CI were then used to establish and quantify degrees of associations (at α = 0.05 level), respectively.
Results
The “D‐0” determinant code had no CA cases (table 1) and there was no evidence of significant association between outcome and the determinant codes for both CA (OR 0, 95% CI 0 to 41.14; p = 1.000) and Blue‐in categories (OR 0.89, 95% CI 0.34 to 2.33; p = 1.000). The automated, protocol‐based call taking (that is, All “C”) group identified more cardiac arrest and blue‐in encounters than the overrides (that is, “D‐O”) group.
Table 1 All determinant code “C” vs “D‐0”, stratified by outcome (that is, CA/Blue‐in).
| Outcome | n | All “C” | “D‐0” | OR (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| n (%) | n | |||||
| CA | Yes | 125 | 125 (100.00) | 0 | 0 (0 to 41.14) | 1.000 |
| No | 113764 | 113679 (99.93) | 85 | |||
| Blue‐in | Yes | 5998 | 5994 (99.93) | 4 | 0.89 (0.34 to 2.33) | 1.000 |
| No | 107891 | 107810 (99.92) | 81 | |||
CA, cardiac arrest, CI, confidence interval; OR, odds ratio.
Similarly, there were no CA cases (table 2) for the determinant code “E‐0” and the association between outcome and determinant codes for both CA (OR 0, 95% CI 0 to 70.05; p = 1.000) and Blue‐in categories (OR 1.17, 95% CI 0 to 7.12; p = 0.597) was not significant (table 2). Again, the automated, protocol‐based call taking (that is, All “D”) group identified more cardiac arrest and blue‐in encounters than the overrides (that is, “E‐O”) group.
Table 2 All determinant code “D” vs “E‐0”, stratified by outcome (that is, CA/Blue‐in).
| Outcome | n | All “D” | “E‐0” | OR (95% CI) | p Value | |
|---|---|---|---|---|---|---|
| n (%) | n | |||||
| CA | Yes | 1500 | 1500 (100.00) | 0 | 0 (0 to 70.05) | 1.000 |
| No | 273457 | 273447 (99.99) | 10 | |||
| Blue‐in | Yes | 23904 | 23903 (100.00) | 1 | 1.17 (0 to 7.12) | 0.597 |
| No | 251053 | 251044 (99.99) | 9 | |||
CA, cardiac arrest, CI, confidence interval; OR, odds ratio.
Discussion
The first examination of the EMD‐allowed override feature in ProQA was done at the Cleveland EMS (Ohio) Communication “Red” Center in 1993. A 1 year 75 899 case dataset revealed an unexpectedly low override percentage of 0.22%. A subsequent 87 203 case dataset from the same centre in 1995 showed an identical override percentage of 0.22%.8 Previously, it was our unsupported belief that this override upgrading would occur in 3–5% of all cases. Seven additional EMS/EMD datasets examined universally demonstrated a <1% override (choice in San Diego, USA (0.07%); Dorset, UK (0.22%); Pittsburgh, USA (0.05%); AMR‐Denver, USA (0.29%); Kent, UK (0.06%); Cripple Creek, Colorado, USA (0.84%); and London, UK (0.57%) ( J Clawson, ProQA report coding statistics, unpublished data).
The EMD training curriculum of the IAED emphasises that each Key Question represents a dispatch‐relevant objective—otherwise it would not be included in the protocol. There are four basic classes of recognised objectives (table 3).
Table 3 Four basic objectives of key questioning.
| Objective | |
|---|---|
| 1 | To identify the correct problem or situation and the proper response configuration to it without going under |
| 2 | To determine the presence of conditions requiring the provision of pre‐arrival instructions and special advice |
| 3 | To provide necessary information to the responders so they can pre‐plan their actions and appropriate equipment that will be needed while en route |
| 4 | To provide for the safety of all those at the scene: patients, caller, bystanders, and responders |
With a clear understanding of this process, it would appear that an EMD's need to override routinely a recommended dispatch code would be minimised. This may be the case here. Since no automated systems of other dispatch protocol/guideline methodologies are currently in use, it is not possible to see if this is a result of strict protocol compliance‐based training and routine quality assurance review, or if it would be routinely found.
Overrides from lower acuity code levels (OMEGA, ALPHA, BRAVO) were not examined since these levels, and their next higher override levels, would be unlikely to contain enough high acuity cases with which to perform this same acuity‐based study. Given the small numbers of overrides in our study, it is important to note that only a large difference in outcome would be detected.
Limitations
Although this paper is based on the largest dataset available, from the ambulance trust often considered the largest and busiest in the world, some cells (within the contingency tables) still contain small numbers (or frequency) for overridden codes. However, this was adjusted for by the use of Fisher's exact test instead of χ2 test.
It was not possible to determine if the overrides examined belonged disproportionately to certain individuals in the London corps of about 360 EMDs or if they were more heterogeneously distributed among all EMD call takers.
The LAS, as is the case with virtually all ambulance services throughout the UK, utilises the MPDS codes to set response time parameters based on NHS Department of Health‐established response time goals. These response groups are as shown in table 4. There is currently not a spectrum of different crew‐type responses generated for higher codes, as the London fleet is predominately composed of paramedic (ALS) trained crews and no fire brigade first responders are utilised.
Table 4 UK National Health Service response groups9.
| Category | Definition |
|---|---|
| A | Patients who are or may be immediately life threatened and will benefit from a timely clinical intervention |
| B | Patients who require urgent face to face clinical attention but are not immediately life threatened |
| C | Patients who do not require an immediate or urgent response by blue light and may be suitable for alternative pathways of care* |
*This category C dataset is approved on the basis that arrangements for dealing with these calls are clinically appropriate, timely, auditable, and fit within local clinical governance arrangements.
Conclusions
This study contradicts the belief that EMDs can accurately perceive when a patient or situation requires more resources than the MPDS's structured interrogation process logically indicates. This further strengthens the concept that automated, protocol‐based call taking is more accurate and consistent than the subjective, anecdotal or experience‐based determinations made by individual EMDs.
As of this writing, the IAED intends to examine these findings further. However, based on the low number of overrides currently performed in the systems examined, it is the authors' opinion that the allowed override feature should remain in place for the rare cases of logic or machine failure, as well as for uncommon cases of true clinical intuition, or when the EMD encounters confused callers or cases involving language barriers.
Acknowledgements
The authors would like to thank Mike Damiani, Management Information Analyst, LAS, for data sorting and provision; the full corps of LAS EMDs for their dedication and very high compliance to the dispatch protocol, and the six EMD Quality Assurance professionals that conduct the ongoing quality assurance case review that ensures the high compliance necessary for study data inclusion. We sincerely thank Pamela Stewart, Executive Assistant, Research & Standards, PDC, for organizational overview, proofreading, care and feeding of the authors.
Abbreviations
BIQ - “bluing in” percentage quotient
CA - cardiac arrest
CAQ - cardiac arrest percentage quotient
EMD - emergency medical dispatcher
IAED - International Academies of Emergency Dispatch
LAS - London Ambulance Service
MPDS - Medical Priority Dispatch System
NHS - National Health Service
Footnotes
Source of support: No specific funding was provided outside of the employment relationships noted in the competing interests section below.
Conflict of interest: JC is CEO and Medical Director of the Research and Standards Division of Priority Dispatch Corp. and member of the Council of Standards, Board of Certification, and Board of Trustees of the International Academies of Emergency Dispatch. He is the inventor of the Medical Priority Dispatch Protocol and Quality Assurance System studied herein. BP is Academics and Standards Editor for the IAED and Chair of the IAED Council of Research. CO is a medical informatics researcher and statistical expert employed part‐time by the IAED for study development and validation only. AH is the Priority Dispatch Development Officer for the London Ambulance Service NHS Trust and the Emergency Call Management Advisor with lead on Call Categorisation at the Department of Health, UK. GS is a Medical Protocol and Quality Assurance Consultant, Priority Dispatch Corporation.
Ethical approval: Not required. All the data were gleaned from a specific 999 call aggregate database not containing any patient identifying information.
Contributors: AH de‐identified, aggregated and provided the initial one‐year 999 call and outcome database. JC conceived the study idea, formulated the initial study plan and protocol. JC, AH, BP, GS, and CO drafted the manuscript, which was revised based on the comments of all authors. CO provided the statistical structure and validation of the data.
References
- 1.International Academy of Emergency Medical Dispatch The 20 points of accreditation, revised 2000. www.emergencydispatch.org/AM20points.html, (accessed 22 Feb 2007)
- 2.International Academy of Emergency Medical Dispatch Accreditation approved compliance score minimums. 1992. www.emergencydispatch.org/AM20points.html, (accessed 22 Feb 2007)
- 3.Clawson J, Cady G, Martin R.et al Effect of a comprehensive quality management process on compliance with protocol in an emergency medical dispatch center. Ann Emerg Med 199832578–584. [DOI] [PubMed] [Google Scholar]
- 4.London Ambulance Services NHS Trust CAS MEET Blue Call System, London Ambulance Service NHS Trust Central Ambulance Control Training Department Training Brief 2002
- 5.Brown R, Warwick J. Blue Calls – Time for a change? Emerg Med J 200118289–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clawson J. Manhunt! Improve AED response helping: police enrich “The Cardiac Arrest Quotient”, Special educational supplement: The life you save…community defibrillation programs and the public safety responder. National Center for Early Defibrillation, February 2002
- 7.International Academy of Emergency Medical Dispatch EMD v11.2 UKE‐Ω Protocol. Medical Priority Dispatch System. 2006
- 8.Cleveland (Ohio) E M S.1995 master dispatch analysis, principles of emergency medical dispatch, 3rd ed, v11.2, appendix F, pgs A.16–27. Priority Press 2004
- 9.Department of Health, UK Implementing changes to 999 call categorization: Annex A–Call category definitions. 10/09/2004. http://www.dh.gov.uk/en/publicationsandstatistics/lettersandcirculars/dearcolleagueletters/DH_4089082 (accessed 9 June 2007)