Abstract
Objectives. We estimated associations between poverty in early, middle, and later childhood and adult body mass index to further elucidate the effects of socioeconomic status on health.
Methods. We conducted secondary analyses of data from men and women (N = 885) born between 1968 and 1975 who were tracked between their prenatal and birth years and adulthood in the nationally representative Panel Study of Income Dynamics. We used multivariate regression techniques and spline models to estimate the relationship between income in different stages of childhood and adult body mass index, overweight, and obesity. We controlled for other family characteristics, including income in other periods of childhood.
Results. Mean annual family income in the prenatal and birth years for children whose annual family incomes averaged less than $25 000 was significantly associated with increased adult body mass index, but mean annual family income between 1 and 5 years of age and between 6 and 15 years of age was not.
Conclusions. Our results indicated that economic conditions in the earliest period of life (during the prenatal and birth years) may play an important role in eventual anthropometric measures.
The prevalence of overweight and obesity among US adults has reached alarming proportions, with a national average adult body mass index (BMI; weight in kilograms divided by height in meters squared) of 26.6 kg/m2 and rates of overweight and obesity at 34% and 30%, respectively.1 Although morbid obesity is less common than overweight, rates have also risen over time, to a current prevalence of 4.7%.2 These problems are costly to the affected individual, because overweight has adverse effects on morbidity, mortality, and earnings3; excess body weight is the fifth most important risk factor contributing to the burden of disease in developed countries. Overweight and obesity are also costly for society: obesity is responsible for approximately 5% to 7% of total annual health care expenditures in the United States.3 Given the high prevalence and high cost of adult excess body mass, it is important to identify the factors that predict adult overweight, particularly those factors that might be amenable to intervention.
The key to preventing obesity and other health problems lies in the identification of modifiable risk factors. Socioeconomic conditions are consistent correlates of BMI. A large body of literature links adult socioeconomic conditions and adult BMI or weight gain in adulthood.4,5 In developed countries, individuals with higher socioeconomic status are less likely to be overweight or obese. This inverse relationship between social class and BMI appears as early as 1 year of age.6 Studies have established a gradient in adult BMI correlated with childhood social class (typically indexed by paternal occupation).6,7 This research suggests an enduring role for early childhood socioeconomic conditions on adult BMI but does not provide clear implications for intervention, because it is not obvious how amenable fathers’ occupational status is to change.
Early childhood income is a key predictor of later-life human capital outcomes.8 However, it is uncertain whether low income during this childhood period also plays a uniquely important role in predicting body mass in adulthood. If we can identify the specific associations between income in childhood and adult health, there may be a greater chance of implementing targeted interventions for low-income children in the United States. Why might income in early childhood (the prenatal period to 5 years of age) predict overweight and obesity in adulthood? The fetal origins hypothesis posits a programming process whereby stimulants and insults during the prenatal period have long-lasting implications for physiology and disease risk.9 Low income during the prenatal period may be associated with fetal undernutrition, low birth weight, or slow growth in the first 2 years of life. A pattern of small size at birth and low BMI at age 2, followed by rapid weight gain after age 2, is a risk factor for the development of insulin resistance and a disproportionately high fat mass in relation to muscle mass. Low income is also associated with food insecurity,10 and some research shows positive cross-sectional associations between food insecurity and early childhood overweight status.11
Other pathways could include the effect of low income in childhood on educational attainment or occupational status. Low-income children attain less education as adults, and education is an important determinant of health, in part through knowledge of a healthful diet and health-inducing behaviors.8 Low-income children are also more likely as adults to work in lower-status occupations, in which social norms about thinness, healthful eating, and exercise habits may be less strong or in which opportunities for on-site exercise and healthful eating are less prevalent.5 Low income in childhood may also be related to the early development and persistence of different social norms of eating, exercise, and overweight. Finally, low income in early childhood has been linked to poor physical and mental health in adulthood. Clearly, physical limitations may constrain the physical activity necessary to control weight. Poor mental health, such as depression, may lead to overeating, physical inactivity, or stress, all of which are associated with the development of excess body mass.
Our goal was to estimate associations between early childhood income and later-life body mass. If such a link can be established, it will further support the case for early-life intervention. Several early-life interventions appear to provide practical and cost-effective approaches to promoting human capital development.12 Interventions early in life may be an equally productive way to promote adult health.
METHODS
Study Population
We conducted a secondary analysis of data from the US Panel Study of Income Dynamics (PSID) and estimated links between income early in childhood and later-life BMI. The PSID is a longitudinal survey consisting of individuals (men, women, and children) and the families in which they reside.13 It is the longest-running longitudinal study of household income in the United States and collects detailed economic and demographic information across the life course. Since 1968, the PSID has tracked, interviewed, and disseminated data from a nationally representative sample of approximately 5000 US households. Annually from 1968 to 1996 and biennially from 1997 to 2005, all members of the original households in the study, regardless of whether they were living in the same dwelling or with the same people, were tracked in the study. Thus, children born into study families, who themselves constituted representative birth cohorts,14 were surveyed as they advanced through childhood and into adulthood. Despite attrition (the effects of which appear to be captured in weighting adjustments15) and the challenges of following offspring as they formed their own households, the sample size grew from 4800 families in 1968 to 7435 families in 2005. All respondents were compensated for their time.
Because the original focus of the data collection effort was the dynamics of poverty, the PSID was designed to comprise 2 independent samples, a cross-sectional national sample and a supplemental sample of low-income families. The oversampling of low-income families in the late 1960s resulted in a sizable subsample of African American families (of the original 4802 families, 33% were African American). Because of the sampling strategy, we used probability-of-selection weights, which correct for unequal selection probabilities as well as differential attrition, in our analyses.
Our target study sample consisted of the 2358 individuals born into PSID households between 1968 and 1975, who thus were between 30 and 37 years of age in 2005. These cohorts were chosen to meet the dual needs of being observed during their prenatal years and well into early adulthood (minimum age of 30 years in 2005). Only 1014 survey respondents classified as heads or spouses of heads in 2005 provided the height and weight information needed to calculate adult BMI. We also eliminated individuals who were missing any of our childhood control variables. To ensure that we had sufficient income data across childhood, we eliminated families of these individuals who failed to participate in at least 12 of the 17 surveys conducted between the individual's prenatal year and 15th birthday. These 2 restrictions eliminated 129 individuals, leaving an analysis sample of 885 adults. Without adjustment for differential attrition, the analysis sample was somewhat more advantaged than was the group of individuals born between 1968 and 1975 whose outcomes were not observed in 2005. The PSID's attrition-adjusted weights reduced or completely eliminated the demographic differentials between the 2 groups.
Family Income During Childhood
An important limitation of most large-scale studies that link early childhood socioeconomic conditions to adult health outcomes is their reliance on relatively crude measures of socioeconomic status, such as manual labor versus nonmanual labor social class as indicated by fathers’ occupational status. This is typically measured only once at some nonspecific point before age 18 years and most often retrospectively in large-scale population-based surveys.16–18 Ours was the first study to link high-quality income data across the entire childhood period, with adult BMI measured as late as age 37 years. Family economic conditions can be volatile,19 so yearly measurement of family income during childhood is required to provide an accurate picture of childhood economic conditions.
We used the PSID's edited measure of annual total family income, collected in each survey year for the previous calendar year's income and inflated to 2005 levels according to the Consumer Price Index (http://www.bls.gov/cpi). This income measure included all cash income received by all household members from all sources—earnings, transfers, and income from assets. Annual income reports were averaged across 3 periods: the prenatal year through the calendar year in which the child was born (2-year period), 1 to 5 years of age (5-year period), and 6 to 15 years of age (10-year period). The perinatal interval (i.e., the prenatal year and the birth year) was chosen to isolate poverty effects for very early childhood. Considerable experimentation showed that the latter 2 childhood intervals best balanced the need to control for economic conditions beyond the perinatal period in a flexible way but without introducing undue multicollinearity into our regression models. For each of the 3 periods, the individual's income was averaged over the years during which the family participated in the survey.
Control Variables
To avoid attributing to early childhood income what should be attributed to correlated determinants of both childhood income and our outcomes of interest, we included several additional control variables in all of our regressions. Our first set of regressions included basic demographic characteristics that are important determinants of weight. These included birth year fixed effects to account for differences in weight by age, as well as gender of the individual. We also included dichotomous variables that distinguished African Americans, Whites, and other races/ethnicities.
We ran a second set of analyses, representing our full-adjustment models, which added covariates measured around the time of the child's birth that have been identified in the literature as important correlates of either childhood income, BMI, or both2–8: whether the child's parents were married and living together, whether the child lived in the South, and the age of the mother. We also controlled for the total number of children born to the child's mother. The remaining covariates represented characteristics of the head of the household (defined as the father in 2-parent households and the mother in single-parent households) into which the child was born: the score on a sentence completion test administered in the 1972 interviewing wave, years of completed schooling, and reports of a physical or nervous condition that limited activities.
Outcome Measures
Our measure of adult BMI was derived from reports in the 2005 survey of heads and wives of their weight in pounds and their height in feet and inches. We calculated BMI as follows:
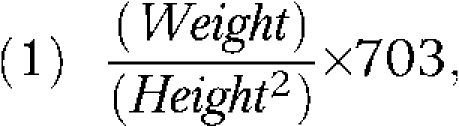 |
where weight was measured in pounds and height was measured in inches.1 We defined overweight as a BMI of 25 kg/m2 or greater (thus including obese individuals) and obesity as a BMI of 30 kg/m2 or greater. We also examined the rare occurrence of morbid obesity, defined as a BMI of 40 kg/m2 or greater.
Data Analysis and Statistical Methods
All data analysis was performed with Stata 9.0 SE for Windows (StataCorp LP, College Station, TX). We calculated descriptive statistics and regression results with the sampling and attrition weights provided by the PSID. Adult continuous BMI was analyzed with ordinary least squares; dichotomous outcomes (overweight, obesity, and morbid obesity) were analyzed with 3 separate logistic regressions. All regressions accounted for the complex sample design of the survey (we used SVY commands in Stata and appropriate stratum and cluster variables provided by the PSID), and we calculated standard errors with Taylor-series linearization. We performed a more general investigation of distributional effects of early poverty on BMI with quantile regressions at the 25th, 50th, and 75th percentiles; we used Stata's QREG command and weighting because survey adjustments were not allowed by the program.
To account for a differential effect of increments to lower as opposed to higher family income, we estimated piecewise linear (spline) models with Stata's MKSPLINE command, with a knot specified at $25 000. Use of a piecewise linear model enabled us to estimate separate slopes for childhood stage–specific incomes below and above $25 000. Experimentation showed that knots below $25 000 reduced precision of the unstandardized parameter estimate on low income without systematically changing the coefficient itself and that knots above $30 000 systematically reduced the coefficients on the first spline segment. We referred to individuals with incomes below $25 000 as low income. We scaled family income in increments of $10 000, so coefficients reflected changes in adult body mass associated with a $10 000 increment to childhood income in the perinatal period, age 1 to 5 years, and age 6 to 15 years.
RESULTS
Descriptive Statistics
Table 1 presents weighted descriptive statistics (means, proportions, and standard deviations) of all study variables for children who spent their perinatal periods in households with mean incomes less than or equal to $25 000 and more than $25 000 per year. On average, sample adults had BMIs of 27.4 kg/m2, slightly higher than the 26.6 kg/m2 national mean reported for adults aged 20 to 74 years in 2000. The obesity rate in the sample (28.8%) was comparable to the 2000 national mean of 30%. However, adults who spent their perinatal periods in low-income families had significantly higher BMIs (F = 46.52; P < .001) and higher rates of overweight (χ2 = 11.69; P = .001), obesity (χ2 = 10.83; P = .001), and morbid obesity (χ2 = 7.58; P < .01) than did those whose perinatal household incomes were above $25 000.
TABLE 1.
Descriptive Statistics of Adults, by Family Income During Early Childhood: Panel Study of Income Dynamics, United States, 1968–2005
| Total Sample (N = 885), Mean (SD) or % | Low Income (n = 226), Mean (SD) or % | High Income (n = 659), Mean (SD) or % | Pa | |
| Adult outcome measures | ||||
| BMI,b kg/m2 | ||||
| Total | 27.4 (5.8) | 30.3 (6.8) | 26.8 (5.4) | <.001 |
| Overweight | 60.7 | 75.6 | 57.7 | <.001 |
| Obese | 28.8 | 45.2 | 25.5 | .001 |
| Morbidly obese | 3.2 | 7.3 | 2.4 | .02 |
| Average income during childhood, $1000 | ||||
| Prenatal to birth | 47.57 (35.19) | 17.11 (5.47) | 53.77 (35.46) | <.001 |
| Aged 1–5 y | 54.00 (31.79) | 31.09 (29.13) | 58.66 (30.26) | <.001 |
| Aged 6–15 y | 68.33 (43.25) | 35.52 (22.03) | 75.02 (43.47) | <.001 |
| Control variables | ||||
| African American | 12.9 | 37.0 | 8.0 | <.001 |
| Male | 51.0 | 45.7 | 52.1 | .26 |
| Born into intact family | 89.4 | 61.5 | 95.1 | <.001 |
| Born in the South | 29.5 | 48.7 | 25.5 | .003 |
| Mother's age at birth, y | 25.6 (5.6) | 21.9 (4.8) | 26.4 (5.5) | <.001 |
| No. of siblings | 2.1 (1.7) | 2.3 (1.7) | 2.1 (1.6) | .22 |
| Head of household test scorec | 9.8 (2.1) | 8.5 (2.4) | 10.1 (1.9) | <.001 |
| Head of household education, y | 12.3 (3.3) | 9.3 (3.7) | 12.9 (2.8) | <.001 |
| Head of household disabled at child's birth | 10.1 | 25.8 | 6.9 | <.001 |
Note. BMI = body mass index. All means and standard deviations were weighted. Low and high income were defined as at or below (low) or above (high) $25 000 average annual family income, respectively, during respondents’ prenatal and birth years.
Based on the test of the null hypothesis that the mean or proportion was identical between the lower- and higher-income groups. Income was in 2005 dollars.
Overweight was defined as a BMI of 25 kg/m2 or greater, obesity was a BMI of 30 kg/m2 or greater, and morbid obesity was a BMI of 40 kg/m2 or greater.
Score for a sentence completion test (highest possible score = 13) administered in the 1972 interviewing wave.
Average annual household incomes increased across childhood but were always much less for children whose perinatal incomes were less than $25 000 than for those whose incomes were $25 000 or greater in the earliest measured period. Children in the 2 income subgroups differed on most of the other demographic characteristics, with the low-income group more likely to be African American and born in the South and less likely to have been born into an intact family. Parents of children in the low-income group had lower test scores and educational attainment when the children were born and were more likely to report health limitations than were higher-income respondents. Most of these demographic differences mirrored the characteristics of poor families in the United States around 1970.
We next examined longitudinal patterns of childhood income. The Pearson correlation between mean income during the prenatal and birth years and between ages 1 through 5 years was 0.70 and between 6 through 15 years was 0.57. Despite the relatively high correlations, income transitions between our 3 childhood periods were fairly common. Table 2 presents the mobility across childhood periods for children classified according to their mean perinatal period incomes. Fewer than one third of the children whose mean annual household income across the perinatal period was below $15 000 had incomes that low between ages 1 and 5 years (32%) or between ages 6 and 15 years (28%). Twenty-eight percent had household incomes greater than $25 000 between ages 1 and 5 years, and half had incomes greater than $25 000 between ages 6 and 15 years. Children whose average perinatal household income was between $15 000 and $25 000 also had similar improvements in household income: 25% had average annual incomes greater than $35 000 between 1 and 5 years of age and 42% between 6 and 15 years of age.
TABLE 2.
Family Income Mobility Across Childhood: Panel Study of Income Dynamics, United States, 1968–2005
| Family Income When Aged 1–5 Years, % |
Family Income When Aged 6–15 Years, % |
|||||||||||
| < $15 000 | $15 000–$24 999 | $25 000–$34 999 | $35 000–$49 999 | ≥ 50 000 | All | < $15 000 | $15 000–$24 999 | $25 000–$34 999 | $35 000–$49 999 | ≥ 50 000 | All | |
| Family income during the perinatal year and the birth year | ||||||||||||
| < $15 000 | 32 | 39 | 19 | 4 | 5 | 100 | 28 | 22 | 23 | 11 | 16 | 100 |
| $15 000–$24 999 | 14 | 37 | 24 | 19 | 6 | 100 | 15 | 20 | 22 | 24 | 18 | 100 |
| $25 000–$34 999 | 2 | 11 | 27 | 42 | 17 | 100 | 8 | 9 | 9 | 28 | 45 | 100 |
| $35 000–$49 999 | 0 | 3 | 13 | 43 | 41 | 100 | 3 | 3 | 8 | 22 | 65 | 100 |
| ≥ $50 000 | 0 | 2 | 3 | 12 | 83 | 100 | 2 | 1 | 4 | 6 | 88 | 100 |
| Unweighted sample size | 49 | 117 | 16 | 245 | 334 | 885 | 70 | 73 | 94 | 164 | 484 | 885 |
Note. Values represent the proportion of each perinatal (prenatal year and birth year) income group in the later-period income groups.
This income volatility enabled us to estimate effects of income very early in childhood while controlling for income in other childhood stages—a key step in controlling for the omitted-variable biases present in most studies of poverty effects.20 Although numerous factors (e.g., genetic endowments) that might simultaneously influence family income and adult body mass were not measured in our data, most omitted variables that we are aware of that would correlate strongly with both body mass and perinatal income would also correlate with income at other childhood stages.
Associations Between Early Childhood Income and Adult Body Mass
Table 3 presents the parameter estimates and 95% confidence intervals (CIs) for the low-income segments of our variables for income in the 3 childhood periods from 2 sets of regressions. The first showed that income in the prenatal and birth years had a significant and negative association with a continuous measure of adult BMI. The coefficient suggested that a $10 000 increase in annual income over these 2 years for the lowest-income children was associated with a reduction in adult BMI of 2.51 kg/m2, a 0.43 SD reduction. By comparison, increases for low-income families in the other 2 childhood periods were not significantly associated with BMI in adulthood. The 3 coefficients on the low-income spline segments were significantly different from each other (adjusted Wald test F = 2.68; P = .08). When the full set of controls was entered into the model, the association between the earliest income and adult BMI was reduced by a little more than 20%, although at −1.94 (95% CI = –3.44, −0.43; P = .01) it was still statistically significant and amounted to one third of a standard deviation. Income in the other childhood stages continued to have a nonsignificant association with BMI.
TABLE 3.
Income Effects From Logistic and Quantile Regression Models for Adults Whose Childhood Family Income Was $25 000 or Less: Panel Study of Income Dynamics, United States, 1968–2005
| BMI Quantile Regression, OR (95% CI) |
|||||||
| BMI, OR (95% CI) | Overweight, OR (95% CI) | Obesity, OR (95% CI) | Morbid Obesity, OR (95% CI) | 25th Percentile | 50th Percentile | 75th Percentile | |
| Prenatal and birth years | |||||||
| Adjusted for age, race, and gender | −2.51 (−4.03, −0.99) | 0.44 (0.26, 0.76) | 0.44 (0.23, 0.86) | 0.77 (0.36, 1.63) | −1.08 (−1.83, −0.32) | −2.38 (−3.14, −1.62) | −3.58 (−4.60, −2.56) |
| Fully adjusteda | −1.94 (−3.44, −0.43) | 0.54 (0.31, 0.95) | 0.59 (0.29, 1.18) | 0.43 (0.23, 0.81) | −1.71 (−1.91, −1.51) | −1.74 (−2.60, −0.88) | −2.83 (−3.83, −1.83) |
| Aged 1–5 y | |||||||
| Adjusted for age, race, and gender | −0.87 (−4.35, 2.61) | 1.22 (0.48, 2.72) | 1.63 (0.79, 3.36) | 0.44 (0.07, 2.87) | −0.02 (−1.16, 1.11) | −0.07 (−1.10, 0.97) | 0.01 (−1.61, 1.64) |
| Fully adjusteda | −0.86 (−4.58, 2.85) | 1.30 (0.53, 3.23) | 1.63 (0.74, 3.58) | 0.30 (0.06, 1.60) | 0.73 (0.47, 0.98) | 1.32 (0.15, 2.48) | −0.58 (−1.93, 0.76) |
| Aged 6–15 y | |||||||
| Adjusted for age, race, and gender | 0.17 (−1.99, 2.32) | 0.91 (0.37, 2.24) | 0.71 (0.33, 1.52) | 3.16 (0.85, 11.76) | −1.01 (−1.92, −0.11) | −0.66 (−1.42, 0.09) | −0.55 (−1.82, 0.73) |
| Fully adjusteda | 0.12 (−2.28, 2.52) | 0.92 (0.32, 2.62) | 0.75 (0.31, 1.77) | 2.45 (0.80, 7.50) | −0.80 (−0.97, −0.63) | −0.88 (−1.74, −0.02) | 0.55 (−0.52, 1.61) |
Note. BMI = body mass index; OR = odds ratio; CI = confidence interval. Values are ORs or regression coefficients and associated CIs for the low income ($0–$25 000) spline segments. Weighted regression coefficients are given for BMI and weighted ORs for overweight, obesity, and morbid obesity. BMI, overweight, obesity, and morbid obesity models were adjusted for the complex sample design of the survey. Quantile regressions were weighted. Average incomes were scaled in increments of $10 000 and were in 2005 dollars.
Full adjustments included birth year, race, gender, parents’ marital status at respondent's birth, residence in the South at birth, age of mother at birth, number of siblings, head of household's score on a sentence completion test in 1972, years of completed schooling of the household head at respondent's birth, and household head's report of physical or nervous condition in respondent's birth year.
Logistic regressions of overweight, obesity, and morbid obesity showed that a $10 000 annual increase in mean prenatal and birth year incomes for low-income children reduced the odds ratios (ORs) of both overweight and obesity to 0.44. The fully controlled model estimates (ORs = 0.54 and 0.59) were somewhat larger, with the perinatal income OR in the obesity regression no longer statistically significantly different from unity at P at less than .05.
With only 3% of the weighted sample classified as morbidly obese (BMI ≥ 40 kg/m2), the PSID provided relatively little power to detect associations between childhood conditions and morbid obesity. Nevertheless, a logistic regression with morbid obesity as a dependent variable and our full set of control variables produced a statistically significant estimate of risk associated with low early childhood income (OR = 0.43; 95% CI = 0.23, 0.81; P = .011).
To further explore distributional differences, we estimated quantile regressions for BMI at the 25th, 50th, and 75th percentiles of the BMI distribution. In our sample these percentile cutoffs were equivalent to BMIs of 23.6 kg/m2, 27.3 kg/m2, and 31.3 kg/m2, respectively. We found statistically significant effects of early childhood income in both the partially and the fully controlled models at the 25th, 50th, and 75th percentiles, with the largest BMI reduction at the 75th percentile of the distribution. These findings were consistent with our logistic analysis of overweight, obesity, and morbid obesity and suggested that the associations between early poverty and adult body mass were particularly strong at the upper portion of the BMI distribution.
DISCUSSION
Understanding socioeconomic inequalities in health is a public health priority. We examined whether income in 3 different periods during childhood was associated with BMI, overweight, and obesity when the child reached adulthood (age 30–37 years). Our results indicated that low household income in the earliest period of life (averaged across the prenatal and birth years) had a significant association with eventual anthropometric measures, even after we controlled for other family characteristics at birth and for income in other periods of childhood. By contrast, we found no significant association between later income and our outcomes. Previous research found an important relationship between socioeconomic characteristics in childhood and adult health, but our study was the first to use longitudinal data spanning the entire period of childhood on a nationally representative US sample.
Our finding of the particular importance of income during the prenatal and birth years for adult BMI is consistent with the hypothesis that fetal programming induced by early stimulants and insults has long-lasting implications for physiology and disease risk.21,22 If the prenatal and birth years represent a sensitive period during which social processes become embedded in biology, epigenetic modifications could be responsible for these associations.9 In particular, overnutrition or undernutrition during pregnancy (both of which could be correlated with low income during the prenatal period) affect, among others things, fat cells and pancreatic B-cell development, which can result in irreversible changes in appetite regulation.9 Low income is also associated with exposure to environmental stressors, which can result in physiological changes that affect eating behavior.23,24 These findings provide initial evidence that social and environmental influences may be especially relevant for individuals vulnerable to weight gain, suggesting that genotypes may moderate children's sensitivity to environmental insults.
Although the PSID is well suited to estimating the unique contribution of early childhood income to adult BMI, it lacks key mediational measures during childhood, such as BMI (of the child or the parent), physical activity, stress exposure, health risk behaviors, diabetic status of the mother at the time of the child's birth, and breastfeeding practices, all of which might help provide an understanding of the process by which early economic conditions matter. Despite this limitation, existing literature about the role of these childhood measures finds that they are associated with children's health but do not explain the relationship between socioeconomic status and health.25–27
PSID data relate to children born in the late 1960s and early 1970s, before much of the recent increase in childhood and adult BMI levels. Associations between childhood income and adult BMI may differ for more recent cohorts. A further limitation was the use of self-reported height and weight. Previous studies indicated that height is overestimated and weight is underestimated among both men and women.28 This suggests that obesity prevalence determined by self-report is underreported29 and that our findings may be lower-bound estimates of the relationship between early childhood poverty and adult BMI.
Our findings point to the potential importance of income transfers, particularly investments in early childhood, on influencing eventual health. In particular, our findings indicate that we should focus our efforts on those who are the most economically disadvantaged. Virtually all countries have a variety of tax and transfer programs that redistribute income. In the United States, the Earned Income Tax Credit pays up to $4400 per year to low-income working families, the Temporary Assistance for Needy Families program provides cash grants to low-income families for limited periods, and the child tax credit grants a nonrefundable credit of up to $1000 per year per child (as of the 2008 tax year). Targeting these transfers, or similar programs, to families with the youngest children may offer the largest benefit for health and well-being.
Acknowledgments
This project was funded by the Partnership for America's Economic Success and the Robert Wood Johnson Foundation Health and Society Scholars program (RWJ HSS grant number 053572).
We thank participants at the University of Chicago Department of Health Studies seminar series, Robert Wood Johnson Foundation–Health and Society Scholars seminar participants at Harvard University, and Andrea Danese for helpful comments and suggestions.
Note. The funding organizations were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the article. The views expressed are those of the authors and not the Partnership for America's Economic Success or The Robert Wood Johnson Foundation.
Human Participant Protection
No protocol approval was needed for this study.
References
- 1.Centers for Disease Control and Prevention Healthy weight, overweight, and obesity among US adults. 2003. Available at: http://wwwcdcgov/nchs/data/nhanes/databriefs/adultweightpdf. Accessed November 1, 2007
- 2.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288:1723–1727 [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein EA, Ruhm CJ, Kosa KM. Economic causes and consequences of obesity. Annu Rev Public Health 2005;26:239–257 [DOI] [PubMed] [Google Scholar]
- 4.Ball K, Crawford D. Socioeconomic status and weight change in adults: a review. Soc Sci Med 2005;60:1987–2010 [DOI] [PubMed] [Google Scholar]
- 5.McLaren L. Socioeconomic status and obesity. Epidemiol Rev 2007;29:29–48 [DOI] [PubMed] [Google Scholar]
- 6.Laitinen J, Power C, Järvelin MR. Family social class, maternal body mass index, childhood body mass index, and age at menarche as predictors of adult obesity. Am J Clin Nutr 2001;74:287–294 [DOI] [PubMed] [Google Scholar]
- 7.Langenberg C, Hardy R, Kuh D, Brunner E, Wadsworth M. Central and total obesity in middle aged men and women in relation to lifetime socioeconomic status: evidence from a national birth cohort. J Epidemiol Community Health 2003;57:816–822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duncan GJ, Yeung WJ, Brooks-Gunn J, Smith JR. How much does childhood poverty affect the life chances of children? Am Sociol Rev 1998;63:406–423 [Google Scholar]
- 9.Strauss RS. Effects of the intrauterine environment on childhood growth. Br Med Bull 1997;53:81–95 [DOI] [PubMed] [Google Scholar]
- 10.Casey PH, Szeto K, Lensing S, Bogle M, Weber J. Children in food-insufficient, low-income families: prevalence, health, and nutrition status. Arch Pediatr Adolesc Med 2001;155:508–514 [DOI] [PubMed] [Google Scholar]
- 11.Casey PH, Simpson PM, Gossett JM, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics 2006;118:e1406–e1413 [DOI] [PubMed] [Google Scholar]
- 12.Heckman JJ. The economics, technology, and neuroscience of human capability formation. Proc Natl Acad Sci USA 2007;104:13250–13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Panel Study of Income Dynamics. Ann Arbor: Institute for Social Research, University of Michigan; Available at: http://psidonline.isr.umich.edu. Accessed September 10, 2008 [Google Scholar]
- 14.Duncan GJ, Hill MS. Conceptions of longitudinal households: fertile or futile? J Econ Soc Meas 1985;13:361–375 [Google Scholar]
- 15.Fitzgerald J, Gottschalk P, Moffitt R. An analysis of sample attrition in panel data: the Michigan Panel Study of Income Dynamics. J Hum Resour 1998;33:251–299 [Google Scholar]
- 16.Lawlor DA, Sterne JA, Tynelius P, Davey Smith G, Rasmussen F. Association of childhood socioeconomic position with cause-specific mortality in a prospective record linkage study of 1 839 384 individuals. Am J Epidemiol 2006;164:907–915 [DOI] [PubMed] [Google Scholar]
- 17.Lawlor DA, Ronalds G, Macintyre S, Clark H, Leon DA. Family socioeconomic position at birth and future cardiovascular disease risk: findings from the Aberdeen Children of the 1950s cohort study. Am J Public Health 2006;96:1271–1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Power C, Graham H, Due P, et al. The contribution of childhood and adult socioeconomic position to adult obesity and smoking behaviour: an international comparison. Int J Epidemiol 2005;34:335–344 [DOI] [PubMed] [Google Scholar]
- 19.Duncan GJ, Rodgers WL. Longitudinal aspects of childhood poverty. J Marriage Fam 1988;50:1007–1021 [Google Scholar]
- 20.Mayer S. What Money Can't Buy Cambridge, MA: Harvard University Press; 1997 [Google Scholar]
- 21.Barker DJP. Mothers, Babies, and Health in Later Life 2nd ed Edinburgh, Scotland: Churchill Livingstone; 1998 [Google Scholar]
- 22.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol 2002;31:1235–1239 [DOI] [PubMed] [Google Scholar]
- 23.Gunstad J, Paul RH, Spitznagel MB, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res 2006;142:31–37 [DOI] [PubMed] [Google Scholar]
- 24.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol 2005;67:259–284 [DOI] [PubMed] [Google Scholar]
- 25.Currie A, Shields MA, Price SW. The child health/family income gradient: evidence from England. J Health Econ 2007;26:213–232 [DOI] [PubMed] [Google Scholar]
- 26.Currie J, Lin W. Chipping away at health: more on the relationship between income and child health. Health Aff (Millwood) 2007;26:331–344 [DOI] [PubMed] [Google Scholar]
- 27.Case A, Lubotsky D, Paxson C. Economic status and health in childhood: the origins of the gradient. Am Econ Rev 2002;92:1308–1334 [DOI] [PubMed] [Google Scholar]
- 28.Gorber SC, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev 2007;8:307–326 [DOI] [PubMed] [Google Scholar]
- 29.Visscher TL, Viet AL, Kroesbergen IH, Seidell JC. Underreporting of BMI in adults and its effect on obesity prevalence estimations in the period 1998 to 2001. Obesity (Silver Spring) 2006;14:2054–2063 [DOI] [PubMed] [Google Scholar]


