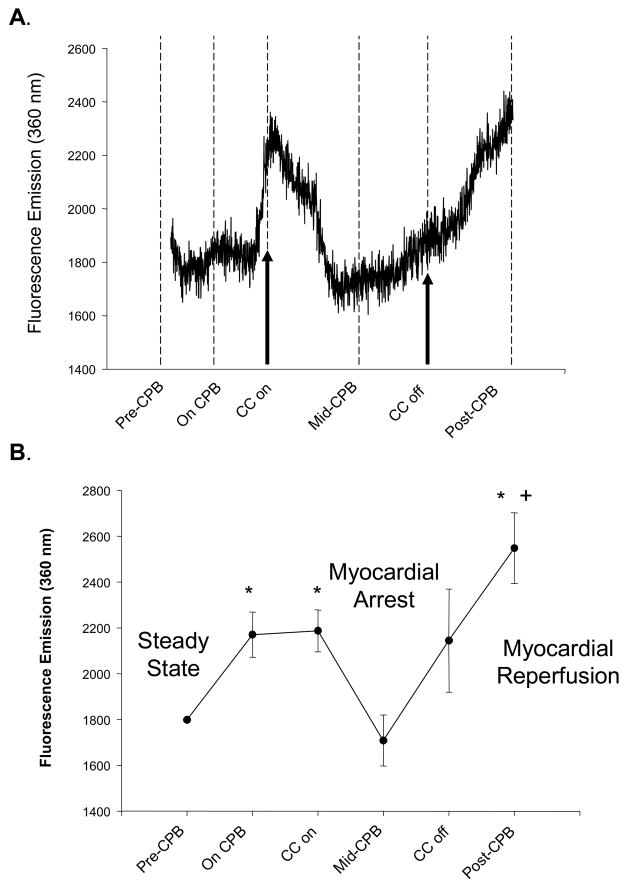
Figure 3.
(A) A representative continuous fluorescence recording of myocardial interstitial fluid from a patient undergoing coronary bypass surgery requiring cardiopulmonary bypass (CPB) and myocardial arrest. After collection of baseline recordings (Steady-State), the patient was placed on CPB and a cross-clamp placed across the ascending aorta interrupting blood flow to the myocardium (Myocardial Arrest). Cardioplegia solution was administered at pre-specified intervals during CPB and this myocardial arrest period. Restoration of myocardial blood flow was achieved by release of the aortic cross-clamp (Myocardial Reperfusion) and following restoration of sinus rhythm and ventricular pump function, the patient was separated from CPB and the probe removed. In this particular example, the baseline, steady-state collection period was 40 minutes, the cross-clamp time was 35 minutes (Myocardial Arrest time), total CPB time was 55 minutes and the probe was removed at 20 minutes following separation from CPB. The initiation of CPB caused a small increase in fluorescent emission, reflective of increased interstitial activity. With myocardial arrest, fluorescent emission fell to within steady-state levels. However, with myocardial reperfusion, there was a surge in fluorescent emission, indicative of heightened MMP activity within the myocardial interstitium. (B) An average of fluorescent emission was computed for all patients with complete recordings (n=14) at critical time points. Fluorescent emission increased with the onset of CPB, significantly fell with myocardial arrest, and increased significantly with myocardial reperfusion. (*p<0.05 vs normalized steady-state values, +p<0.05 vs CPB values prior to myocardial arrest).