Fig. 1.
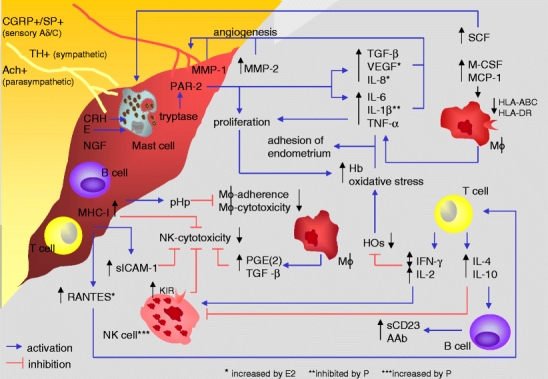
Neuroendocrine–immune disequilibrium in endometriosis. AAb autoantibodies, Ach achetylcholine, CGRP calcitonin-gene-related peptide, CRH corticotropin-releasing hormone, E estrogens, E2 estradiol, Hb hemoglobin, HO heme oxygenases, IL interleukin, HLA human leukocyte antigen, IFN-γ interferon-γ, KIR killer cell inhibitory receptor, M-CSF macrophage colony stimulating factor, MCP-1 monocyte chemotactic protein-1, MHC-I major histocompatibility complex class-I, MMP matrix metalloproteinase, NGF nerve growth factor, NK natural killer, P progesterone, PAR-2 protease-activated receptor-2, PGE(2) prostaglandin E(2), pHp peritoneal haptoglobin, RANTES regulated upon activation normal T cell expressed and secreted, sCD23 soluble CD23, SCF stem cell factor, sICAM-1 soluble intercellular adhesion molecule-1, SP substance P, TGF-β transforming growth factor-β, TH tyrosine hydroxylase, TNF-α tumor necrosis factor-α, VEGF vascular endothelial growth factor. In endometriosis, elevated levels of M-CSF, MCP-1, RANTES, and SCF in peritoneal fluid might lead to increased numbers of macrophages, T cells, and mast cells. Although markers of antigen presentation on macrophages such as HLA-ABC and HLA-DR are decreased in endometriosis, macrophage-derived IL-6, IL-1β, TNF-α, TGF-β, VEGF, and IL-8 are increased in peritoneal fluid, together with MMP-1 and MMP-2 stimulating angiogenesis. IL-6, IL-1β, and TNF-α support adhesion of endometrial cells to the peritoneum, and TNF-α stimulates the proliferation of ectopic tissue, resulting in high levels of Hb. T cell-derived IL-2 and IFN-γ decrease HO, leading to oxidative stress, and would, in sufficient levels, increase NK cell activity. IFN-γ has been inconsistently described as increased or decreased. Increased T cell-derived IL-4 and IL-10 inhibit cellular immunity and stimulate B cells to AAb production. sCD23 is increased in peritoneal fluid in endometriosis and might derive from activated B cells. Lymphocytes are increased in peritoneal fluid and abundantly present in ectopic tissue. Decreased NK cell cytotoxicity might be due to high anti-inflammatory T cytokines, increased KIR, high macrophage-derived PGE(2) and TGF-β, high MHC-I expression on ectopic cells, and high sICAM-1 levels in peritoneal fluid. Nerve fibers found within lesions are positive for CGRP, SP, TH, and Ach, and NGF and CRH were demonstrated. CRH and accumulated E can activate mast cells to release tryptase, activating PAR-2, which leads to increased secretion of VEGF, IL-8, and IL-6 and proliferation of ectopic tissue. pHp, expressed by ectopic tissue, decreases adherence and, in stage 3 and 4, cytotoxicity of peritoneal macrophages. E2 further increases RANTES, IL-8, and VEGF, whereas P inhibits IL-1β secretion from peritoneal macrophages and increases NK cell numbers
