Abstract
OBJECTIVE
The purpose of this study was to examine the effects of weight loss on sympathetic nervous system responsiveness to glucose ingestion in obese subjects with metabolic syndrome, in whom such responses are reportedly blunted.
RESEARCH DESIGN AND METHODS
Thirty four subjects, 19 insulin resistant and 15 insulin sensitive and aged 55 ± 1 years (mean ± SE) with BMI 31.6 ± 0.6 kg/m2, who fulfilled the Adult Treatment Panel III criteria for metabolic syndrome participated. Simultaneous measurements of whole-body norepinephrine spillover rate, calf blood flow, and intra-arterial blood pressure were made at times 0, 30, 60, 90, and 120 min postglucose (75 g). The experiment was repeated after a 3-month hypocaloric diet with or without an exercise program.
RESULTS
Body weight decreased by 8.1 ± 0.9 and 8.4 ± 1.1 kg and resting norepinephrine spillover by 94 ± 31 and 166 ± 58 ng/min (all P ≤ 0.01) in insulin-resistant and insulin-sensitive subjects, respectively. Weight loss was accompanied by a marked increase in sympathetic responsiveness after glucose but only in insulin-resistant subjects. In this subgroup, comparative increases in norepinephrine spillover rates at baseline and after weight loss averaged −3 ± 25 versus 73 ± 24 ng/min at 30 min (P = 0.039), 36 ± 21 versus 115 ± 28 ng/min at 60 min (P = 0.045), 9 ± 21 versus 179 ± 50 ng/min at 90 min (P < 0.001), and 40 ± 48 versus 106 ± 39 ng/min at 120 min (P = 0.24).
CONCLUSIONS
Weight loss reverses blunted sympathetic responsiveness to glucose ingestion in insulin-resistant subjects with metabolic syndrome, which is relevant to postprandial energy utilization and body weight homeostasis.
There is much evidence to indicate that the sympathetic nervous system (SNS) is activated by food intake and particularly by carbohydrate ingestion (1–3). Oral glucose elicits a marked and sustained increase in SNS activity over a 2-h period in healthy humans, as assessed by measurements of plasma norepinephrine concentration, by regional norepinephrine spillover, and by direct microneurographic recordings of muscle sympathetic nerve activity (MSNA) (1–3). At least two mechanisms are thought to contribute to this neurophysiological response: the postprandial increase in plasma insulin and the entrance of a nutrient into the gastrointestinal tract (4). Insulin exerts its sympathoexcitatory effects either directly by facilitating central sympathetic outflow or indirectly by activation of the baroreceptor reflex in response to its peripheral vasodilatory effects (5). The observation that C-peptide–negative diabetic patients retain a blunted MSNA responsiveness to oral glucose, even in the absence of endogenous insulin (6), suggests that insulin-independent factors such as hemodynamic adjustment to splanchnic vasodilation and gastrointestinal distension may also contribute to sympathetic activation after carbohydrate ingestion (4). Postprandial SNS stimulation is physiologically important in the regulation of facultative thermogenesis or the rise in energy expenditure after dietary intake (7).
A growing body of data suggests that obesity and the insulin-resistant state are accompanied by impaired sympathetic neural responsiveness to physiological hyperinsulinemia, glucose ingestion, and changing energy states. Vollenweider et al. (8) showed that in lean young subjects MSNA increased by 94% in response to euglycemic hyperinsulinemia, whereas in age-matched obese subjects the increase was only 9%. MSNA responses to oral glucose are diminished in insulin-resistant Pima Indians (9), and short-term under- and overfeeding is accompanied by blunted sympathetic responsiveness in obese subjects (10). The metabolic syndrome is an increasingly prevalent multidimensional risk factor for cardiovascular disease and type 2 diabetes. Several indexes of SNS activity, such as norepinephrine spillover from sympathetic nerves and MSNA at rest, are known to be increased in subjects with the metabolic syndrome even in the absence of hypertension (11,12). We have recently demonstrated that obese insulin-resistant subjects with metabolic syndrome have both blunted and delayed norepinephrine spillover and MSNA responses to oral glucose compared with obese insulin-sensitive subjects with metabolic syndrome (13). Sympathetic responsiveness related inversely to measures of central adiposity and the insulin response and positively to fitness level (13).
Weight loss and exercise are recommended as first-line treatments for the metabolic syndrome, and both lifestyle modalities are known to reduce SNS activity and improve metabolic syndrome components (11). No study to date has examined whether weight loss alters the dynamic sympathetic neural response to glucose ingestion. The aims of the present investigation were twofold: 1) to test the hypothesis that weight loss would reverse the blunted SNS response to glucose in obese individuals with metabolic syndrome and 2) to compare the benefits of weight loss in insulin-resistant and insulin-sensitive subjects. To accomplish these aims, we simultaneously measured plasma glucose, insulin, leptin, whole-body norepinephrine kinetics, calf blood flow, intra-arterial blood pressure, and heart rate during a standard oral glucose tolerance test (OGTT) at baseline and after a 12-week weight loss program.
RESEARCH DESIGN AND METHODS
Nonsmoking, untreated, white subjects (21 male and 13 postmenopausal female) aged 55 ± 1 years (mean ± SE) were studied. All subjects were participating in the lifestyle intervention arms of an ongoing randomized controlled trial examining the benefits of dietary weight loss alone or together with aerobic exercise on sympathetic activity. To be eligible, participants had to have central obesity (waist circumference ≥102 cm in men and ≥88 cm in women) and two or more metabolic syndrome parameters as per the updated National Cholesterol Education Program Adult Treatment Panel III criteria (14). These include elevated triglycerides (≥1.7 mmol/l); reduced HDL cholesterol (<1.03 mmol/l in men and <1.3 mmol/l in women); elevated fasting glucose (≥5.6 mmol/l), and elevated blood pressure (≥130 mmHg systolic or ≥85 mmHg diastolic). Potential study subjects were initially screened by physical examination, medical history, 12-lead electrocardiogram, blood biochemistry, and lipid analyses. Subsequently, they underwent a fitness assessment, during which maximal oxygen consumption (Vo2max) was measured using an incremental cycle ergometry protocol (Quark b2; Cosmed, Rome, Italy). Body composition was determined by dual-energy X-ray absorptiometry scan (GE-LUNAR Prodigy Advance PA+130510; GE Medical Systems Lunar, Madison, WI). Subjects with type 2 diabetes (fasting glucose ≥7 mmol/l or receiving drug treatment for elevated glucose) or a history of secondary hypertension, cardiovascular, cerebrovascular, renal, liver, or thyroid disease were excluded. Written informed consent was obtained from all subjects. The study protocol was approved by the Alfred Hospital Ethics Committee.
OGTT.
Subjects attended at 0800 h, having fasted for 12 h and abstained from caffeine for 18 h and from alcohol and strenuous exercise for 36 h. Before attendance, they collected a 24-h urine specimen to quantify sodium intake. Experiments were performed in a quiet room (ambient temperature 22°C) with subjects lying in a supine position. They voided before commencement of the experiments. A 20-G venous cannula was inserted into an antecubital vein for infusion of tritiated norepinephrine, and an arterial cannula was placed into the brachial artery for blood sampling. Subjects then ingested 75 g glucose in liquid form (Glucaid; Fronine, Taren Point, NSW, Australia). Arterial blood was sampled every 30 min over 2 h for the measurement of glucose, insulin, and leptin concentrations. Whole-body insulin sensitivity was calculated from OGTT parameters according to the formula of Matsuda and DeFronzo (15). This insulin sensitivity index has been validated against the euglycemic insulin clamp and is highly correlated with the rate of whole-body glucose disposal during the clamp (r = 0.73, P < 0.0001) (15). Subjects were stratified into insulin-sensitive and insulin-resistant groups based on cut points of >2.1 and ≤2.1, respectively, which correspond to insulin areas under the plasma concentration–time curve (AUC0–120) of <10,000 and ≥10,000 mU · l−1 · min−1, respectively (13).
SNS activity.
Whole-body SNS activity during the OGTT was assessed by measurement of the apparent rate of appearance of norepinephrine in arterial plasma (“norepinephrine spillover rate”), using the radioisotope dilution method (16). This technique involves the intravenous infusion of [3H]norepinephrine and measurement of norepinephrine-specific activity and endogenous norepinephrine under steady-state conditions. The technique provides a simultaneous estimate of norepinephrine plasma clearance. After a priming bolus of 6 μCi of 1-[ring-2,5,6-3H]norepinephrine (specific activity, 10–30 μC/mmol; Perkin-Elmer), an infusion was commenced at 0.07 μCi/m2 per min. To ensure that steady-state levels of infusate were attained, baseline arterial blood samples (time 0) were taken at least 30 min after commencement of the infusion. Postglucose arterial samples were obtained at 30, 60, 90, and 120 min. Intra-arterial blood pressure and the electrocardiogram-derived heart rate were continuously recorded and averaged over 15 min at time 0 and over 5 min at the other time points (PowerLab recording system, model ML 785/8SP; ADI Instruments).
Calf blood flow measurements.
Calf arterial blood flow (milliliters per minute per 100 ml tissue) was measured in the left leg using automated venous occlusion plethysmography equipment (D.E. Hokansen, Bellevue, WA) as described previously (13) and represented the average of 12 measurements at times 0, 30, 60, 90, and 120 min.
Lifestyle interventions.
After baseline testing, all subjects were prescribed a hypocaloric diet designed to elicit a caloric deficit of 600 kcal/day for a period of 12 weeks. The diet consisted of 30% fat (9% saturated, 15% monounsaturated, and 6% polyunsaturated), 48% carbohydrates, and 22% protein and was based on a modified version of the Dietary Approaches to Stop Hypertension diet (17). Subjects attended fortnightly for body weight and blood pressure checks, and they completed regular prospective 4-day diet records. In addition, a subset of 16 subjects also participated in an exercise-training program during the 12 weeks. This consisted of 30–40 min of aerobic cycling exercise, performed on alternate days at a moderate intensity of 65% of their predetermined maximum heart rate. Compliance was monitored by the measurement of Vo2max and by exercise records. Because weight loss and weight loss plus exercise resulted in similar lowering of whole-body norepinephrine spillover rate (18), the lifestyle groups were pooled for this analysis.
Laboratory measurements.
Plasma concentrations of neurochemicals were determined by high-performance liquid chromatography with electrochemical detection. Intra-assay coefficients of variation (CVs) in our laboratory are 1.3% for norepinephrine and 2.3% for [3H]norepinephrine; inter-assay CVs are 3.8 and 4.5%, respectively. Arterial plasma glucose was quantified by enzymatic methods using an Architect C18000 analyzer (Abbott Laboratories, North Chicago, IL) and insulin and leptin were quantified by radioimmunoassay (Linco Research, St. Charles, MO). Plasma total cholesterol, HDL cholesterol, and triglycerides were determined by automated enzymatic methods and plasma high-sensitivity C-reactive protein (hsCRP) by immunoturbidimetric assay.
Statistical methods.
Data are expressed as means ± SE. Statistical analysis was performed using SigmaStat (version 2.03 for Windows; SPSS). Differences between insulin-sensitive and insulin-resistant subjects were compared by Student's unpaired t tests. The courses of norepinephrine kinetics and other variables during the OGTT were analyzed by two-way repeated-measures ANOVA, with the Holm-Sidak test for multiple pairwise comparisons. Nonparametric data were log transformed before analyses. AUC0–120 values were calculated by the trapezoidal rule. The ratio of the norepinephrine spillover AUC0–120 to the insulin AUC0–120 was calculated for each subject as an index of sympathetic responsiveness for a given increase in insulin concentration. Associations between variables were evaluated by Pearson's and Spearman's rank correlations, as appropriate. Forward stepwise regressions were carried out with those univariate correlations for which P < 0.05. Statistical significance was accepted at two-sided P < 0.05.
RESULTS
Subject characteristics.
Demographic and clinical data for the whole group and two subgroups are shown in Table 1. Age, sex, and lifestyle treatment assignment did not differ between the groups. Insulin-resistant subjects had significantly higher BMI, plasma leptin concentration, fasting insulin, insulin AUC0–120, and homeostasis model assessment of insulin resistance (HOMA-IR) and a significantly lower Matsuda insulin sensitivity index, compared with insulin-sensitive subjects. Resting blood pressure, fitness level, 24-h urinary sodium excretion, arterial norepinephrine concentration, and calculated norepinephrine spillover rate were similar in the two groups; however, norepinephrine plasma clearance was significantly greater in insulin-sensitive subjects.
TABLE 1.
Demographic and clinical characteristics of study subjects
| Whole group | Insulin sensitive | Insulin resistant | |
|---|---|---|---|
| n | 34 | 15 | 19 |
| Sex (male/female) | 21/13 | 11/4 | 10/9 |
| Age (years) | 55 ± 1 | 54 ± 1 | 55 ± 1 |
| BMI (kg/m2) | 31.6 ± 0.6 | 30.3 ± 0.7 | 32.7 ± 0.9* |
| Waist (cm) | 105.8 ± 1.7 | 104.2 ± 2.0 | 107.0 ± 2.5 |
| Total body fat mass (kg) | 35.4 ± 1.2 | 32.9 ± 1.6 | 37.3 ± 1.6 |
| Triglycerides (mmol/l) | 2.0 ± 0.2 | 2.3 ± 0.4 | 1.7 ± 0.2 |
| HDL cholesterol (mmol/l) | 1.23 ± 0.05 | 1.21 ± 0.07 | 1.24 ± 0.06 |
| Leptin (ng/ml) | 17.2 ± 2.8 | 13.9 ± 4.9 | 19.8 ± 3.2* |
| hsCRP (mg/l) | 2.5 ± 0.3 | 2.1 ± 0.4 | 2.8 ± 0.5 |
| Systolic blood pressure (mmHg) | 132 ± 3 | 133 ± 5 | 132 ± 4 |
| Diastolic blood pressure (mmHg) | 76 ± 1 | 76 ± 2 | 76 ± 2 |
| Heart rate (bpm) | 62 ± 1 | 60 ± 2 | 64 ± 2 |
| 24-h urinary sodium (mmol/day) | 149 ± 12 | 160 ± 20 | 140 ± 16 |
| Fasting glucose (mmol/l) | 5.6 ± 0.1 | 5.4 ± 0.1 | 5.7 ± 0.2 |
| Glucose AUC0–120 (mmol · l−1 · min−1) | 1160 ± 25 | 1129 ± 31 | 1184 ± 33 |
| Fasting insulin (mU/l) | 16.8 ± 1.0 | 12.4 ± 0.9 | 20.3 ± 1.0*** |
| Insulin AUC0–120 (mU · l−1 · min−1) | 9974 ± 731 | 6549 ± 539 | 12,997 ± 713*** |
| Whole-body SI | 2.49 ± 0.19 | 3.33 ± 0.25 | 1.75 ± 0.09*** |
| HOMA-IR | 4.33 ± 0.27 | 3.11 ± 0.24 | 5.30 ± 0.29*** |
| Vo2max/FFM (ml · min−1 · kg−1) | 28.7 ± 0.9 | 30.4 ± 1.8 | 27.3 ± 0.9 |
| Lifestyle intervention (WL/WL + EX) | 18/16 | 7/8 | 11/8 |
| Norepinephrine (pg/ml) | 212 ± 20 | 181 ± 28 | 236 ± 28 |
| Whole-body norepinephrine spillover (ng/min) | 399 ± 42 | 465 ± 77 | 347 ± 41 |
| Norepinephrine clearance (l/min) | 2.0 ± 0.1 | 2.6 ± 0.2 | 1.6 ± 0.1*** |
Data are means ± SE. Insulin sensitive and insulin resistant defined as insulin sensitivity index (SI) >2.1 and ≤2.1, respectively (15).
*P < 0.05,
***P < 0.001 vs. insulin-sensitive subjects by Student's unpaired t test. WL, dietary weight loss alone; WL + EX, dietary weight loss and aerobic exercise.
Sympathetic responsiveness to glucose at baseline.
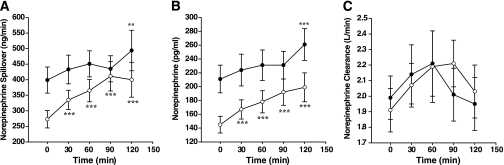
Norepinephrine kinetics during the OGTT are presented in Fig. 1 for the whole group. At baseline, arterial norepinephrine concentration and calculated norepinephrine spillover rate increased significantly only at 120 min. Blunted sympathetic responsiveness was most pronounced in the insulin-resistant subjects at 30 and 120 min postglucose. At these time points, absolute change in norepinephrine spillover averaged −3 ± 40 versus 82 ± 40 ng/min (P = 0.07) and 40 ± 48 versus 165 ± 61 ng/min (P = 0.02) in insulin-resistant and insulin-sensitive subjects, respectively. The ratio of norepinephrine spillover AUC0–120 to plasma insulin AUC0–120 was significantly greater in insulin-sensitive subjects (10.6 ± 1.5 vs. 3.6 ± 0.41, P < 0.001). Sex did not influence sympathetic responsiveness. Plasma leptin levels did not change during the course of the OGTT in the whole group or in the two subgroups.
FIG. 1.
Norepinephrine kinetics in response to 75 g oral glucose at baseline and after weight loss (WL) (n = 34): whole-body norepinephrine plasma spillover rate (A), arterial norepinephrine concentration (B), and norepinephrine plasma clearance (C). Values are means ± SE. Data (log transformed) were analyzed by two-way repeated-measures ANOVA, using the Holm-Sidak test for pairwise comparisons. **P < 0.01 and ***P < 0.001 versus time 0. Whole-body norepinephrine spillover rate: time effect P < 0.001; treatment effect P = 0.01; time × treatment interaction P = 0.003. Arterial norepinephrine concentration: time effect P < 0.001; treatment effect P < 0.001; time × treatment interaction P = 0.07. Norepinephrine plasma clearance: no significant time, treatment, or interaction effects. ●, baseline; ○, post–weight loss.
Correlation analysis showed a positive association between fitness (Vo2max/free fat mass [FFM]) and the increase in norepinephrine spillover at 30 min (r = 0.36, P = 0.04), 60 min (r = 0.45, P = 0.008), and 90 min (r = 0.40, P = 0.02) postglucose. In contrast, the high-sensitivity C-reactive protein (hsCRP) concentration was inversely associated with the norepinephrine spillover response at 60 min (r = −0.46, P = 0.007) and 90 min (r = −0.55, P < 0.001), as was fasting plasma leptin at 90 min (r = −0.53, P = 0.002) and 120 min (r = −0.38, P = 0.03). BMI, HOMA-IR, and fasting insulin correlated inversely with norepinephrine spillover response at 90 min (r = −0.34, P = 0.04; r = −0.34, P = 0.05; and r = −0.39, P = 0.02, respectively). HOMA-IR, insulin AUC0–120, and the absolute change in plasma insulin concentration all correlated inversely with norepinephrine spillover at 120 min (r = −0.33, P = 0.05; r = −0.35, P = 0.05; and r = −0.47, P = 0.007, respectively).
Effects of weight loss on sympathetic responsiveness.
At the end of the 12-week lifestyle intervention program, the 34 subjects lost an average of 8.2 ± 0.7 kg body weight (range 1.8–17.5 kg) and 6.4 ± 0.6 kg fat mass, and their waist circumference decreased by 8.6 ± 0.8 cm (all P < 0.001). Vo2max/FFM increased from 28.7 ± 0.9 to 30.8 ± 1.1 ml · min−1 · kg−1 (P = 0.009). These changes were accompanied by a significant improvement in all metabolic syndrome components (Table 2). Resting norepinephrine spillover rate and plasma norepinephrine decreased by 126 ± 31 ng/min and 66 ± 15 pg/ml, respectively (both P < 0.001), whereas norepinephrine plasma clearance was unchanged.
TABLE 2.
Change in anthropometric, metabolic, and hemodynamic parameters after a 12-week lifestyle intervention
| Whole group | Insulin sensitive | Insulin resistant | |
|---|---|---|---|
| n | 34 | 15 | 19 |
| Body weight (kg) | −8.2 ± 0.7‡ | −8.4 ± 1.1‡ | −8.1 ± 0.9‡ |
| Waist circumference (cm) | −8.6 ± 0.8‡ | −9.8 ± 1.3‡ | −7.6 ± 0.9‡ |
| Total body fat mass (kg) | −6.4 ± 0.6‡ | −6.9 ± 1.1‡ | −6.0 ± 0.7‡ |
| Trunk fat mass (kg) | −3.9 ± 0.4‡ | −4.1 ± 0.8‡ | −3.7 ± 0.6‡ |
| Triglyceride (mmol/l) | −0.7 ± 0.1‡ | −0.9 ± 0.2‡ | −0.6 ± 0.2‡ |
| HDL cholesterol (mmol/l) | −0.06 ± 0.03* | −0.06 ± 0.05 | −0.06 ± 0.03 |
| Fasting glucose (mmol/l) | −0.6 ± 0.1‡ | −0.5 ± 0.1‡ | −0.7 ± 0.1‡ |
| Fasting insulin (mU/l) | −4 ± 1‡ | −3 ± 1* | −5 ± 1‡ |
| Insulin AUC0–20 (mU l−1 · min−1) | −2,232 ± 428‡ | −1,543 ± 489* | −2,913 ± 626† |
| Whole-body SI | 1.11 ± 0.29‡ | 1.6 ± 0.5‡ | 0.7 ± 0.2‡ |
| Fasting leptin (ng/ml) | −7.4 ± 1.4‡ | −5.7 ± 2.2‡ | −8.7 ± 1.9‡ |
| hsCRP (mg/l) | −0.4 ± 0.2* | −0.5 ± 0.3 | −0.4 ± 0.3 |
| Urinary sodium (mmol/day) | −35 ± 10† | −35 ± 17 | −35 ± 12* |
| Systolic blood pressure (mmHg) | −11 ± 2‡ | −13 ± 3‡ | −10 ± 2‡ |
| Diastolic blood pressure (mmHg) | −4 ± 1‡ | −5 ± 2† | −3 ± 1* |
| Heart rate (bpm) | −4 ± 1† | −3 ± 2 | −5 ± 2† |
| Vo2/FFM (ml · min−1 · kg−1) | 2.2 ± 0.7† | 2.0 ± 0.9 | 2.3 ± 1.2* |
| Resting calf blood flow (ml · min−1 · 100 ml−1) | −0.14 ± 0.12 | −0.06 ± 0.20 | −0.20 ± 0.16 |
Data are means ± SE.
*P < 0.05,
†P ≤0.01,
‡P ≤0.001 vs. baseline by two-way repeated-measures ANOVA and Holm-Sidak pairwise comparisons. Blood pressures are the average of five supine Dinamap recordings (model 1846 SX; Critikon, Tampa, FL). SI, insulin sensitivity index.
The norepinephrine spillover response to glucose increased after weight loss, being highly significant at all time points from 30 min onward (all P < 0.001 versus time 0) (Fig. 1). Lifestyle intervention had the greatest effect on sympathetic responsiveness at 90 min, as the absolute change in norepinephrine spillover rate increased threefold at this time point from 36 ± 26 ng/min at baseline to 138 ± 31 ng/min after weight loss (P = 0.02).
Subgroup and correlation analyses.
Subgroup analysis showed that insulin-resistant and insulin-sensitive subjects lost similar amounts of body weight (8.1 ± 0.9 vs. 8.4 ± 1.1 kg), total body fat mass (6.0 ± 0.7 vs. 6.9 ± 1.1 kg), and trunk fat mass (3.7 ± 0.5 vs. 4.1 ± 0.8 kg). Insulin AUC0–120 tended to decrease more in insulin-resistant than in insulin-sensitive subjects (2,913 ± 626 vs. 1,543 ± 489 mU · l−1 · min−1, P = 0.10 between groups). Improvements in fitness level and whole-body insulin sensitivity index and the reductions in 24-h urinary sodium excretion did not differ between the groups (Table 2).
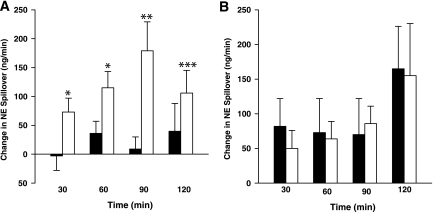
Resting norepinephrine spillover rate decreased by 94 ± 31 and 166 ± 58 ng/min (both P ≤ 0.01) in insulin-resistant and insulin-sensitive subjects, respectively (P = 0.29 between groups). These changes were accompanied by a marked and statistically significant increase in sympathetic responsiveness postglucose but only in insulin-resistant subjects (Fig. 2). Percent change in norepinephrine spillover at baseline and post–weight loss averaged 5 ± 6 versus 36 ± 11% at 30 min (P = 0.03), 14 ± 6 versus 47 ± 9% at 60 min (P = 0.009), 9 ± 6 versus 65 ± 10% at 90 min (P < 0.001), and 20 ± 13 versus 40 ± 9% at 120 min (P = 0.25) in this group. In contrast, absolute and percent changes in norepinephrine spillover did not differ at any of the time points in the insulin-sensitive subjects, indicating that weight loss did not modify sympathetic responsiveness in this group (Fig. 2). The ratio of the AUC0–120 of norepinephrine spillover to the AUC0–120 of plasma insulin increased from 3.57 ± 0.41 to 4.96 ± 0.94 (P = 0.057) in the insulin-resistant subjects but did not change in the insulin-sensitive group. Leptin concentrations were unaltered during the OGTT in both groups. Subgroup analyses by sex showed that weight loss reversed blunted sympathetic responsiveness to glucose in both male and female participants (data not shown).
FIG. 2.
Change in whole-body norepinephrine (NE) spillover (nanograms per minute) from time 0 in insulin-resistant (n = 19) (A) and insulin-sensitive (n = 15 (B) subjects at baseline (■) and after weight loss (WL, □). *P < 0.05, **P < 0.01, and ***P < 0.001 versus baseline by Student's paired t test.
Correlation analysis (n = 34) revealed inverse relationships between the change in the log-norepinephrine spillover AUC0–120–to–insulin AUC0–120 ratio and changes in fasting log leptin (r = −0.433, P = 0.02), abdominal fat mass (r = −0.38, P = 0.03), and body weight (r = −0.33, P = 0.06). Reductions in body weight, central adiposity, and fasting leptin levels were associated with an increase in the sympathetic response for a given level of plasma insulin. In stepwise regression analysis, the change in log fasting leptin concentration was independently associated with the change in norepinephrine spillover AUC0–120–to –insulin AUC0–120 ratio, accounting for 19% of the variance.
Hemodynamic responses during OGTT.
Paired calf blood flow data were available for 32 subjects. At baseline, there was an inverse relationship between resting whole-body norepinephrine spillover and resting calf blood flow (r = −0.35, P = 0.047). During the OGTT, calf blood f low increased significantly from 60 min onward at baseline and after weight loss (time effect both P < 0.001) but was not influenced by weight loss (treatment effect P = 0.22). This was also the case when insulin-resistant and insulin-sensitive subjects were analyzed separately. There were no differences in the magnitude of calf blood flow responses to glucose when analyzed by treatment or subgroup. Change in calf blood flow did not correlate with change in norepinephrine spillover at any of the time points.
Weight loss was associated with a significant reduction in arterial diastolic blood pressure at rest (by 9 ± 2 mmHg, n = 32) and at all time points during the OGTT (treatment effect P < 0.001). At baseline, glucose ingestion was accompanied by a lowering of diastolic blood pressure that was significant from 30 min onward (time effect P = 0.006). After weight loss, there were no significant time effects on diastolic blood pressure (treatment × time interaction P = 0.006). The same findings were confirmed in both insulin-resistant and insulin-sensitive subjects. Resting arterial systolic blood pressure fell after weight loss (by 9 ± 3 mmHg, P = 0.002); however, there were no significant glucose-related time effects at baseline or after weight loss in the whole group or subgroups. Resting heart rate fell after weight loss (by 4 ± 1 bpm, P < 0.001). After glucose administration, heart rate increased significantly at all time points from 30 min onward at both the baseline visit and the visit after weight loss (time effect P < 0.001). There were no differences in the heart rate response between insulin-sensitive and insulin-resistant subjects.
DISCUSSION
It has long been recognized that energy-restricted diets and physical training both exert sympathoinhibitory effects as well as improving the metabolic profile of subjects with metabolic syndrome (11,19). As such, these lifestyle interventions are recommended as first-line treatments for the metabolic syndrome, a condition that is characterized by sympathetic overactivity (12,20). The novel finding of the present study is that weight loss by consumption of a hypocaloric diet with or without exercise not only lowers resting sympathetic drive but also reverses the blunted sympathetic responsiveness to glucose ingestion that has been reported in the obese state. In agreement with previously published data (9,13,21), our study shows that blunted stimulation of the norepinephrine appearance rate is most pronounced in insulin-resistant subjects. In turn, insulin-resistant subjects experienced the greatest increase in sympathetic responsiveness after weight loss, despite comparable weight loss in the insulin-sensitive group. Correlation analysis showed that reductions in body weight, central adiposity, and plasma leptin levels were most strongly associated with the increase in the SNS response for a given level of plasma insulin.
What mechanisms may underlie these changes in SNS responsiveness? Despite increasing evidence for a pathophysiological role of insulin-mediated sympathoexcitation, the mechanisms and sites through which insulin increases SNS activity remain to be fully elucidated. Circulating insulin reaches the central nervous system via a saturable, active transport process across the blood-brain barrier. Insulin receptors are widely distributed in the human brain in several distinct regions, including the hypothalamus (mainly arcuate nucleus), cerebral cortex, and cerebellum (22). In a series of rodent experiments, Muntzel (5) demonstrated that intracerebroventricular insulin infusion evoked acute increases in lumbar sympathetic nerve activity, an effect that was abolished by anteroventral third ventricle lesioning. In healthy humans, euglycemic hyperinsulinemia in the postprandial range increases MSNA, which is consistent with the concept that insulin stimulates central sympathetic outflow (23). Impaired blood-to-brain transport of insulin may be one mechanism contributing to the blunted sympathetic responses to glucose in obese insulin-resistant subjects. A reduced cerebrospinal fluid–to-plasma insulin ratio has recently been reported with increasing BMI and HOMA-IR index, suggesting that obesity in humans is characterized by a relative central nervous system insulin deficit (24). These data are supported by findings in genetically obese rats, which exhibit reduced brain capillary insulin binding compared with lean rats (25). Reduced insulin delivery into the brain has also been demonstrated in canine models of insulin resistance, induced by high fat feeding or dexamethasone administration (26). To date, there are limited data on the benefits of reversing central insulin resistance by therapeutic interventions. Intranasal administration of insulin, which enables a direct delivery of peptide to the brain without substantial absorption into the blood stream, has been shown to acutely raise blood pressure but not muscle sympathetic nerve activity in healthy subjects (27).
An alternative explanation of our findings is that weight loss may have improved insulin-induced vasodilation in skeletal muscle, thus eliciting greater baroreflex-mediated increases in SNS activity postglucose. Blunted vasodilatory responses to insulin have been previously reported in obese compared with lean humans (8) and attributed to impaired release of endothelium-derived mediators. Weight loss alone or together with exercise improves conduit and resistance artery endothelial function in obese adults (19,28). In the present study, baseline calf blood flow was inversely related to whole-body norepinephrine spillover; however, calf blood flow responses to endogenous insulin did not increase after weight loss. Similarly, the increase in heart rate postglucose that purportedly represents an insulin-mediated cardiac vagal withdrawal and/or increased cardiac sympathetic outflow (29) was not influenced by weight loss.
Leptin concentrations were not acutely altered by glucose ingestion at baseline or after weight loss in either subgroup, which concurs with a study in insulin-resistant Japanese men (30) but not with another study conducted in obese women, which showed an elevation in leptin at times 30 and 60 min postglucose (31). In rodents, leptin administration produces regional sympathetic activation, and, conversely, sympathoadrenal stimulation inhibits leptin expression and secretion from adipose tissue (32). The inverse relationships between resting plasma leptin levels and the norepinephrine spillover response at baseline and between the fall in plasma leptin levels after weight loss and the increase in plasma norepinephrine response suggests that adiposity, insulin resistance, and leptin may all modulate sympathetic responsiveness to carbohydrate intake.
In summary, the present study demonstrates a hitherto unrecognized benefit of weight loss: the reversal of blunted sympathetic responsiveness to glucose ingestion in insulin-resistant subjects with metabolic syndrome. Our data suggest that the improvement in central insulin resistance, rather than the peripheral vasodilatory response to insulin, mediated the increased sympathetic response to glucose. Hypothalamic insulin signaling is important in initiating a catabolic response, including reduction in food intake and increase in energy expenditure. Approximately one-third of the thermic effect of food can be accounted for by the meal-induced increment in SNS activity. Therefore, improvements in central insulin resistance and sympathetic responsiveness to food intake would be expected to have beneficial effects on energy expenditure and body weight homeostasis. Further intervention trials using insulin-sensitizing agents are needed to confirm the role of central insulin resistance in mediating blunted sympathetic responsiveness in metabolic syndrome obesity. Intranasal insulin delivery may offer another therapeutic avenue (33) to test whether manipulating brain insulin levels affects SNS function in this clinical setting.
ACKNOWLEDGMENTS
This study was supported by a Diabetes Australia Research Trust grant, a Future Forum Research grant, and a Bennelong Foundation grant to N.E.S. The research group also holds a Heart Foundation Grant-in-Aid and a National Health and Medical Research Council (NHMRC) Project grant (472604) from the Australian Government. G.W.L is supported by an NHMRC Senior Research Fellowship and M.D.E. by an NHMRC Senior Principal Research Fellowship. M.P.S. and E.A.L. are supported by NHMRC Career Development Awards.
No potential conflicts of interest relevant to this article were reported.
We thank radiographer Dianne Payne for her dual- energy X-ray absorptiometry scan analyses.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Cox HS, Kaye DM, Thompson JM, Turner AG, Jennings GL, Itsiopoulos C, Esler MD: Regional sympathetic nervous system activation after a large meal in humans. Clin Sci 1995: 89: 145– 154 [DOI] [PubMed] [Google Scholar]
- 2.Berne C, Fagius J, Nikiasson F: Sympathetic response to oral carbohydrate administration: evidence from microelectrode nerve recordings. J Clin Invest 1989: 84: 1403– 1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scott EM, Greenwood JP, Vacca G, Stoker JB, Gilbey SG, Mary DASG: Carbohydrate ingestion, with transient endogenous insulinaemia, produces both sympathetic activation and vasodilation in normal humans. Clin Sci (Lond) 2002; 102: 523– 529 [PubMed] [Google Scholar]
- 4.Fagius J: Sympathetic nerve activity in metabolic control—some basic concept. Acta Physiol Scand 2003; 177: 337– 343 [DOI] [PubMed] [Google Scholar]
- 5.Muntzel MS: Insulin-mediated sympathoexcitation in obesity and type 2 diabetes. Nephrol Dial Transplant 1999; 14: 2282– 2285 [DOI] [PubMed] [Google Scholar]
- 6.Fagius J, Berne C: The increase in sympathetic nerve activity after glucose ingestion is reduced in type 1 diabetes. Clin Sci (Lond) 2000; 98: 627– 632 [PubMed] [Google Scholar]
- 7.Schwartz RS, Jaeger LF, Silberstein S, Veith RC: Sympathetic nervous system activity and the thermic effect of feeding in man. Int J Obes 1987; 11: 141– 149 [PubMed] [Google Scholar]
- 8.Vollenweider P, Randin D, Tappy L, Jequier E, Nicod P, Scherrer U: Impaired insulin-induced sympathetic neural activation and vasodilation in skeletal muscle in obese humans. J Clin Invest 1994; 93: 2365– 2371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spraul M, Anderson EA, Bogardus C, Ravussin E: Muscle sympathetic nerve activity in response to glucose ingestion: impact of plasma insulin and body fat. Diabetes 1994; 43: 191– 196 [DOI] [PubMed] [Google Scholar]
- 10.Bazelmans J, Nestel PJ, Esler MD: Blunted norepinephrine responsiveness to changing energy states in obese subjects. Metabolism 1985; 34: 154– 160 [DOI] [PubMed] [Google Scholar]
- 11.Straznicky NE, Lambert EA, Lambert GW, Masuo K, Esler MD, Nestel PJ: Effects of dietary weight loss on sympathetic activity and cardiac risk factors associated with the metabolic syndrome. J Clin Endocrinol Metab 2005; 90: 5998– 6005 [DOI] [PubMed] [Google Scholar]
- 12.Grassi G, Dell'Oro R, Quarti-Trevano F, Scopelliti F, Seravalle G, Paleari F, Gamba PL, Mancia G: Neuroadrenergic and reflex abnormalities in patients with the metabolic syndrome. Diabetologia 2005; 48: 1359– 1365, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Straznicky NE, Lambert GW, Masuo K, Dawood T, Eikelis N, Nestel PJ, McGrane M, Mariani JA, Socratous F, Chopra R, Esler MD, Schlaich MP, Lambert EA: Blunted sympathetic neural response to oral glucose in obese subjects with the insulin resistant metabolic syndrome. Am J Clin Nutr 2009; 89: 1– 10 [DOI] [PubMed] [Google Scholar]
- 14.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa FAmerican Heart Association, National Heart, Lung, and Blood Institute Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735– 2752 [DOI] [PubMed] [Google Scholar]
- 15.Matsuda M, DeFronzo RA: Insulin sensitivity indices obtained from oral glucose tolerance testing. Diabetes Care 1999; 22: 1462– 1470 [DOI] [PubMed] [Google Scholar]
- 16.Esler MD, Haskings GJ, Willett IR, Leonard PW, Jennings GL: Noradrenaline release and sympathetic nervous system activity. J Hypertens 1985; 3: 117– 129 [DOI] [PubMed] [Google Scholar]
- 17.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N: A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997; 336: 1117– 1124 [DOI] [PubMed] [Google Scholar]
- 18.Straznicky N, Masuo K, Lambert G, Dawood T, Eikelis N, Nestel P, Socratous F, McGrane M, Chopra R, Schlaich M, Esler M, Lambert E: Sympathetic neural adaptation to hypocaloric diet and aerobic exercise in metabolic syndrome subjects (Abstract). J Hypertens 2008; 26( Suppl. 1): S352 [Google Scholar]
- 19.Trombetta IC, Batalha LT, Rondon MUPB, Laterza MC, Kuniyoshi FHS, Gowdak MMG, Barretto ACP, Halpern A, Villares SMF, Negrao CE: Weight loss improves neurovascular and muscle metaboreflex control in obesity. Am J Physiol Heart Circ Physiol 2003; 285: H974– H982 [DOI] [PubMed] [Google Scholar]
- 20.Straznicky NE, Eikelis N, Lambert EA, Esler MD: Mediators of sympathetic activation in metabolic syndrome obesity. Curr Hypertens Rep 2008; 10: 440– 447 [DOI] [PubMed] [Google Scholar]
- 21.Fagius J, Ellerfelt K, Lithell H, Berne C: Increase in muscle nerve sympathetic activity after glucose intake is blunted in the elderly. Clin Auton Res 1996; 6: 195– 203 [DOI] [PubMed] [Google Scholar]
- 22.Hopkins DF, Williams G: Insulin receptors are widely distributed in human brain and bind human and porcine insulin with equal affinity. Diabet Med 1997; 14: 1044– 1050 [DOI] [PubMed] [Google Scholar]
- 23.Berne C, Fagius J, Pollare T, Hjemdahl P: The sympathetic response to euglycaemic hyperinsulinaemia: evidence from microelectrode nerve recordings in healthy subjects. Diabetologia 1992; 35: 873– 879 [DOI] [PubMed] [Google Scholar]
- 24.Kern W, Benedict C, Schultes B, Plohr F, Moser A, Born J, Fehm HL, Hallschmid M: Low cerebrospinal fluid insulin levels in obese humans. Diabetologia 2006; 49: 2790– 2792 [DOI] [PubMed] [Google Scholar]
- 25.Schwartz MW, Figlewicz DF, Kahn SE, Baskin DG, Greenwood MRC, Porte D, Jr: Insulin binding to brain capillaries is reduced in genetically obese, hyperinsulinemic Zucker rats. Peptides 1990; 11: 467– 472 [DOI] [PubMed] [Google Scholar]
- 26.Kaiyala KJ, Prigeon RL, Kahn SE, Woods SC, Schwartz MW: Obesity induced by a high-fat diet is associated with reduced brain insulin transport in dogs. Diabetes 2000; 49: 1525– 1533 [DOI] [PubMed] [Google Scholar]
- 27.Benedict C, Dodt C, Hallschmid M, Lepiorz M, Fehm HL, Born J, Kern W: Immediate but not long-term intranasal administration of insulin raises blood pressure in human beings. Metabolism 2005; 54: 1356– 1361 [DOI] [PubMed] [Google Scholar]
- 28.Pierce GL, Beske SD, Lawson BR, Southall KL, Benay FJ, Donato AJ, Seals DR: Weight loss alone improves conduit and resistance artery endothelial function in young and older overweight/obese adults. Hypertension 2008; 52: 72– 79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van de Borne P, Hauseberg M, Hoffman RP, Mark AL, Anderson EA: Hyperinsulinaemia produces cardiac vagal withdrawal and nonuniform sympathetic activation in normal subjects. Am J Physiol Regul Integr Comp Physiol 1999; 276: 178– 183 [DOI] [PubMed] [Google Scholar]
- 30.Masuo K, Katsuya T, Ogihara T, Tuck ML: Acute hyperinsulinemia reduces plasma leptin levels in insulin-sensitive Japanese men. Am J Hypertens 2005; 18: 235– 243 [DOI] [PubMed] [Google Scholar]
- 31.Bougoulia M, Tzotzas T, Efthymiou H, Koliakos G, Konstantinidis TH, Triantos A, Krassas GE: Leptin concentrations during oral glucose tolerance test (OGTT) in obese and normal weight women. Int J Obes 1999; 23: 625– 628 [DOI] [PubMed] [Google Scholar]
- 32.Mark AL, Rahmouni K, Correia M, Haynes WG: A leptin-sympathetic-leptin feedback loop: potential implications for regulation of arterial blood pressure and body fat. Acta Physiol Scand 2003; 177: 345– 349 [DOI] [PubMed] [Google Scholar]
- 33.Strachan MWJ: Insulin and cognitive function in humans: experimental data and therapeutic considerations. Biochem Soc Trans 2005; 33: 1037– 1040 [DOI] [PubMed] [Google Scholar]