Abstract
OBJECTIVE
To describe a 2-year follow-up of A1C outcomes of a self-regulation intervention for youth with type 1 diabetes.
RESEARCH DESIGN AND METHODS
A total of 81 youths with type 1 diabetes ages 11–16 years were randomized to usual care versus a diabetes personal trainer intervention consisting of six self-monitoring, goal-setting, and problem-solving sessions with trained nonprofessionals. A1C data were obtained from medical records 2 years postintervention, and ANCOVA adjusting for age and baseline A1C was conducted.
RESULTS
An overall intervention effect on A1C (8.93% control vs. 8.43% intervention; F = 8.24, P = 0.05) and a significant intervention-by-age interaction (F = 9.88; P = 0.002) were observed, indicating a greater effect among older than younger youths. Subgroup analyses demonstrated no treatment group differences among pre-/early adolescents but a significant difference in A1C among middle adolescents (9.61% control vs. 8.46% intervention; F = 7.20, P = 0.011).
CONCLUSIONS
Findings indicate maintenance of intervention effects on A1C observed at 1-year follow-up.
Effective behavioral programs designed to counter the deterioration in glycemic control that typically accompanies adolescence (1) could contribute substantially to improving diabetes management in this population, with the potential of impacting long-term management trajectories and health outcomes (2,3). The objective of this study was to assess 2-year A1C outcomes of a self-regulation intervention, delivered by nonprofessionals, for youth with type 1 diabetes. Short-term and 1-year outcomes have previously been reported; these showed a significant A1C effect and a treatment-by-age interaction, indicating a greater intervention effect among older than younger youths (4). The current analyses assessed whether these effects were maintained at 2-year follow-up.
RESEARCH DESIGN AND METHODS
The study design and methods have previously been reported (4). Youth ages 11–16 years diagnosed with type 1 diabetes for at least 1 year and having no other major chronic illnesses or psychiatric diagnoses were recruited during routine visits at two pediatric endocrinology clinics serving a multistate area with urban, suburban, and rural populations. Of 113 eligible youth, 81 (72%) consented to participate. Data were collected by medical record review and in-home assessments with the youth and parents. Random assignment was stratified by age (11–13 vs. 14–16 years) and A1C (<8.0 vs. ≥8.0%) for a total of four strata. The study protocol was approved by the National Institute of Child Health and Human Development institutional review board and the Western institutional review board (for participating clinical sites).
The intervention consisted of six in-person semistructured sessions, supplemented with telephone calls, conducted over ∼2 months by trained nonprofessionals (4). The approach was guided by principles of motivational interviewing, applied behavior analysis, and problem solving. Youth were assisted to identify areas of diabetes-management difficulty and use a structured problem-solving process to improve these areas. The intervention approach was primarily youth focused but encouraged youth to identify and communicate ways in which parents and family members could assist as part of the problem-solving process.
A1C was assessed per standard care protocol at the clinics, and data were extracted from medical records. All analyses control for baseline A1C. Descriptive analyses were conducted with the change in A1C from baseline to each follow-up period in the total sample and in each age subgroup. To determine whether the intervention effect differed across follow-up periods, a repeated-measures ANOVA was conducted and the interaction of group by follow-up period tested. To assess for between-group differences at the 2-year follow-up, ANCOVA was conducted with baseline A1C and age included as covariates. An interaction term (group by age) was added to the model to test whether effects differed by age. If a significant interaction was found, stratified analyses were conducted, with separate models run for youth ages 11–13 and 14–16 years.
RESULTS
At baseline, mean diabetes duration was 7.7 years, 63% of subjects used an insulin pump, 15% were minorities, 80% of households had two or more adults in the home, and 64% of households had income >50,000 USD. For the study, 41 subjects were assigned to the educational control group and 40 to the intervention group. There were no significant differences in demographic characteristics between groups. No subjects changed insulin delivery from injection to pump or vice versa during the study. A1C data were available for 78 participants (39 intervention and 39 control) at the 2-year follow-up.
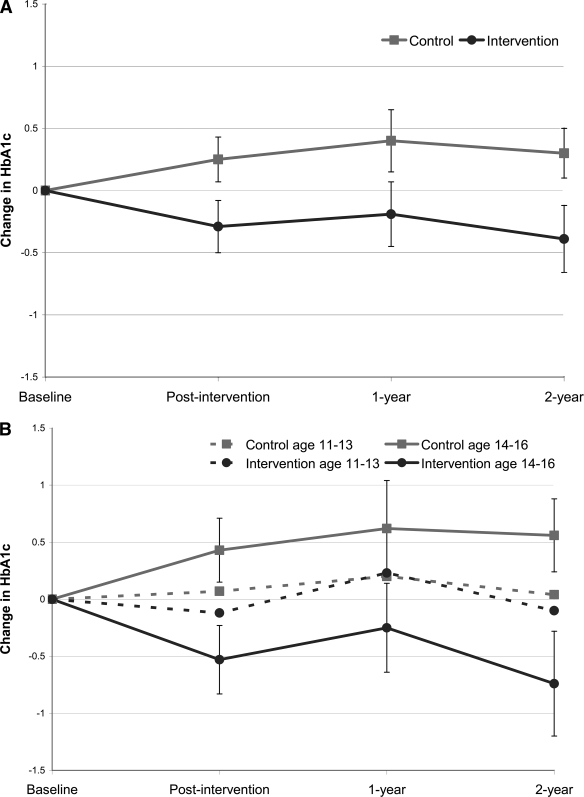
From baseline to 2-year follow-up, the control group showed a mean increase in A1C of 0.30%, whereas the intervention group showed a mean decrease in A1C of 0.39%. The difference between groups at 2-year follow-up paralleled that of the previous follow-up periods (Fig. 1). In early adolescents, A1C for the control group increased 0.04% from baseline, whereas that for the intervention group decreased 0.10%. In middle adolescents, A1C for the control group increased 0.56% from baseline, whereas that of the intervention group decreased 0.74%.
Figure 1.
Change in A1C from baseline to each follow-up period. A: Full sample. B: Age subgroups. Error bars included for groups demonstrating significant differences.
Repeated-measures ANOVA indicated a significant intervention effect (F = 6.92; P = 0.01) and intervention-by-age interaction (F = 7.71; P < 0.01). There was no group–by–follow-up interaction, indicating that the intervention effect did not differ across follow-up periods. Results of the ANCOVA, adjusting for age and baseline A1C, indicated an intervention effect on A1C (8.93% control vs. 8.43% intervention; F = 8.24, P = 0.05) and a significant intervention-by-age interaction, indicating a greater effect among older than among younger youths (F = 9.88; P = 0.002). Stratified analyses for pre-/early adolescents (ages 11–13 years; n = 40) and middle adolescents (ages 14–16 years; n = 38) indicated a significant positive intervention effect for the latter only (9.61% control vs. 8.46% intervention; F = 7.20, P = 0.011).
CONCLUSIONS
Our findings indicated maintenance of the intervention effect on A1C previously demonstrated at short-term and 1-year follow-up (4), suggesting the utility of this behavioral self-regulation intervention for preventing the decline in blood glucose control that typically occurs during adolescence. As was observed previously, however, the intervention only impacted A1C among middle adolescents and not among pre-/early adolescents. These findings suggest that a youth-focused intervention that facilitates the development of self-management and problem-solving skills and uses youth solicitation of parent involvement is an effective strategy for middle adolescents, who are beginning to achieve some autonomy in aspects of diabetes management (5). However, an intervention design that collectively engages both parents and children may be more appropriate during pre- or early adolescence.
The magnitude of difference in glycemic control between treatment groups among middle adolescents was substantial and clinically meaningful; maintenance of this effect could significantly reduce long-term complications of diabetes (6–8). The effect on A1C was comparable in size with that obtained in behavioral interventions of substantially greater intensity, such as that reported by Grey et al. (9) at 12-month follow-up after 6 weekly plus 12 monthly sessions of coping skills training and that by Wysocki et al. (10) at 6-month follow-up in response to 12 sessions of behavioral family systems therapy delivered by professional therapists over 6 months. Few behavioral interventions have reported 2-year follow-up outcomes. Importantly, the degree of difference at 2-year follow-up in this study was virtually identical to that at 1-year follow-up, providing evidence that the effect of a behavioral intervention at this important developmental time could influence adolescents' disease-management trajectory (2,3).
Acknowledgments
This research was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Mortensen HB, Hougaard P: the Hvidøre Study Group on Childhood Diabetes. Comparison of metabolic control in a cross-sectional study of 2,873 children and adolescents with IDDM from 18 countries. Diabetes Care 1997; 20: 714– 720 [DOI] [PubMed] [Google Scholar]
- 2. Brink SJ, Moltz K: The message of the DCCT for children and adolescents. Diabetes Spectrum 1997; 10: 259– 267 [Google Scholar]
- 3. Wysocki T, Hough BS, Ward KM, Green LB: Diabetes mellitus in the transition to adulthood: adjustment, self-care, and health status. J Dev Behav Pediatr 1992; 13: 194– 201 [PubMed] [Google Scholar]
- 4. Nansel TR, Iannotti RJ, Simons-Morton BG, Cox C, Plotnick LP, Clark LM, Zeitzoff L: Diabetes personal trainer outcomes: short-term and 1-year outcomes of a diabetes personal trainer intervention among youth with type 1 diabetes. Diabetes Care 2007; 30: 2471– 2477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Palmer DL, Berg C, Wiebe DJ, Beveridge RM, Korbel CD, Upchurch R, Swinyard MT, Lindsay R, Donaldson DL: The role of autonomy and pubertal status in understanding age differences in maternal involvement in diabetes responsibility across adolescence. J Pediatr Psychol 2004; 29: 35– 46 [DOI] [PubMed] [Google Scholar]
- 6. Diabetes Control and Complications Trial Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005; 353: 2643– 2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Diabetes Control and Complications Trial Research Group. The absence of a glycemic threshold for the development of long-term complications: the perspective of the Diabetes Control and Complications Trial. Diabetes 1996; 45: 1289– 1298 [PubMed] [Google Scholar]
- 8. The Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J Pediatr 1994; 125: 177– 188 [DOI] [PubMed] [Google Scholar]
- 9. Grey M, Boland EA, Davidson M, Li J, Tamborlane WV: Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. J Pediatr 2000; 137: 107– 113 [DOI] [PubMed] [Google Scholar]
- 10. Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, Mauras N, White NH: Effects of behavioral family systems therapy for diabetes on adolescents' family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006; 31: 928– 938 [DOI] [PubMed] [Google Scholar]