Abstract
Background
In 2003, the International Liaison Committee on Resuscitation (ILCOR) published the Recommended Guidelines for Uniform Reporting of Data from Drowning: the “Utstein style” (“Utstein Style for Drowning,” USFD) to improve the understanding of epidemiology, treatment, and outcome prediction after drowning.
Aims
The aim of this study was to compare the characteristics and outcome between patients suffering from out-of-hospital primary cardiac arrest (OHPCA) and drowning victims in cardiac arrest (DCA) by analysis of variables based on the USFD.
Methods
All cases of OHPCA and DCA from February 1998 to February 2007 were included in the research and analysis. Data on OHPCA and DCA patients were collected using the Utstein method. Data on DCA patients were then compared with data of OHPCA patients.
Results
During the study period 788 cardiac arrests with resuscitation attempts were identified: 528 of them were OHPCA (67%) and 32 (4%) were DCA. The differences between DCA and OHPCA patients were: the DCA patients were younger (46.5 ± 21.4 vs 62.5 ± 15.8; p = 0.01), suffered a witnessed cardiac arrest less frequently (9/32 vs 343/528; p = 0.03), were more often found in a nonshockable rhythm (29/32 vs 297/528; p < 0.0001), had a prolonged ambulance response time (11 vs 6 min; p = 0.001), had a relatively better (but not statistically significant) return of spontaneous circulation (ROSC) in the field [22/32 (65%) vs 301/528 (57%); p = 0.33], more of them were admitted to hospital [19/32 (60%) vs 253/528 (48%); p = 0.27], and also had a significantly higher survival rate (discharge from hospital) [14/32 (44%) vs 116/528 (22%); p = 0.01]. DCA patients had higher values of initial PETCO2 (53.2 ± 16.8 vs 15.8 ± 8.3 mmHg; p < 0.0001) and average PETCO2 (43.5 ± 13.8 vs 23.5 ± 8.2; p = 0.002). These values of PETCO2 suggest an asphyxial mechanism of cardiac arrest. The analysis showed that DCA patients who survived were younger, had more bystander cardiopulmonary resuscitation (CPR), shorter call-arrival interval, higher values of PETCO2 after 1 min of CPR, higher average and final values of PETCO2, lower value of initial serum K+, and more of them received vasopressin (p < 0.05) in comparison with DCA patients who did not survive.
Conclusion
DCA patients had a better survival rate (discharge from hospital), higher initial and average PETCO2 values, and more of them had nonshockable initial rhythm. Survival (discharge from hospital) in DCA patients is associated with the PETCO2 values, initial serum K+ values, administration of vasopressin, and ambulance response time.
Keywords: Drowning, Asphyxia, Cardiac arrest, Utstein style report, Cardiopulmonary resuscitation, Outcome
Introduction
Drowning is one of the leading preventable causes of unintentional morbidity and mortality [1]. The most important and detrimental consequence of submersion is hypoxia. Therefore, oxygenation, ventilation, and perfusion should be restored as rapidly as possible. A number of terms are used to describe drowning. The Utstein definition and style of data reporting were created to ensure the use of consistent terminology and the uniform reporting of data from drowning and were published as recommended guidelines in October 2003 (“Utstein Style for Drowning,” USFD) [2]. Patients with cardiac arrest caused by drowning present a specific problem and recent guidelines [1] suggest that basic and advanced cardiac life support used in patients with primary cardiac arrest should be modified for the use in patients with cardiac arrest caused by drowning. The aim of this study was to compare the characteristics and outcome between patients suffering from out-of-hospital primary cardiac arrest (OHPCA) and drowning victims in cardiac arrest (DCA) by analysis of variables based on the USFD.
Methods and patients
The study community (town of Maribor with rural area) has a population of circa 200,000 inhabitants spread over an area of approximately 780 km2. The study population was composed of adults over 18 years with out-of-hospital cardiac arrest (OHCA). All OHPCA and DCA patients from February 1998 to February 2007 were included in the research and analysis. Data on OHPCA and DCA patients were collected using the protocol for emergency intervention, which is a uniform protocol in Slovenia based on the Utstein method. All emergency calls in this period which were classified as OHCA in adults older than 18 years and which were dispatched to the prehospital emergency unit were included.
The Center for Emergency Medicine Maribor has two prehospital emergency teams, which are advanced life support (ALS) units consisting of three members with adequately equipped road vehicles (an emergency physician and two registered nurses or nurses/medical technicians). ALS was provided using a regional protocol that incorporates the standards and guidelines of the European Resuscitation Council. After successful resuscitation, patients were transferred to the intensive care unit of the University Clinical Center Maribor. Demographic information, medical data, and PETCO2 values were recorded for each patient by the emergency physician.
During resuscitation, the PETCO2 values were measured and recorded every minute in the first 5 min of cardiopulmonary resuscitation (CPR) and after that every 5 min, beginning with the initial PETCO2 (first PETCO2 value obtained) immediately after intubation and ending with the final PETCO2 value at admission to the hospital or at termination of CPR. Measurements of PETCO2 were performed with a LIFEPAK 12 defibrillator/monitor (Physio-Control, Inc., a division of Medtronic, Inc., Minneapolis, MN, USA) or infrared sidestream capnometer (BCI Capnocheck Model 20600A1, BCI International, Waukesha, WI, USA).
Hospital records were used for laboratory results at admission and for outcome analysis, including assessment of cerebral performance category (CPC) for patients discharged alive. A CPC score of 1 reflected good cerebral performance, CPC 2 and 3 moderate and severe cerebral disability, CPC 4 comatose, vegetative stage, and CPC 5 brain death [3]. Data were expressed as mean ± standard deviation or as a number (percentage). For the analysis of variables, the Fisher exact test and the Wilcoxon rank sum test were used. The null hypothesis was considered rejected at p values of less than 0.05. Analyses of independent predictors for survival from univariate analysis were performed using a multivariate logistic regression. For statistical analysis SPSS software (version 12.01, SPSS Inc., Chicago, IL, USA) was used.
Results
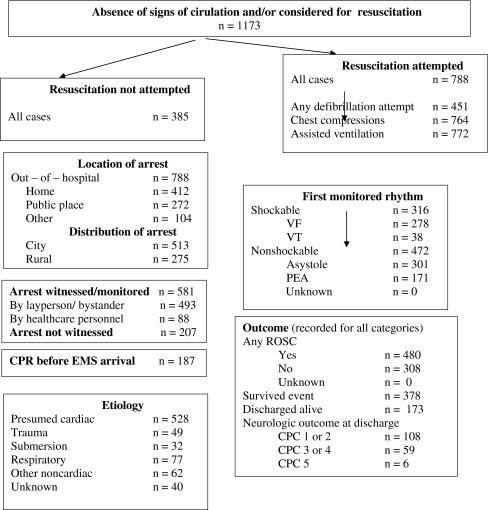
During the study period 788 cardiac arrests with resuscitation attempts were identified: 528 of them were OHPCA (67%) and 32 (4%) were DCA (Fig. 1).
Fig. 1.
Utstein template for reporting out-of-hospital cardiac arrest in Maribor obtained in a 9-year period
The differences between DCA and OHPCA patients were: the DCA patients were younger (46.5 ± 21.4 vs 62.5 ± 15.8; p = 0.01), suffered a witnessed cardiac arrest less frequently (9/32 vs 343/528; p = 0.03), were more often found in a nonshockable rhythm (29/32 vs 297/528; p < 0.0001), had a prolonged ambulance response time (11 vs 6 min; p = 0.001), had a relatively better (but not statistically significant) return of spontaneous circulation (ROSC) in the field [22/32 (65%) vs 301/528 (57%); p = 0.33], more of them were admitted to hospital [19/32 (60%) vs 253/528 (48%); p = 0.27], and also had a significantly higher survival rate (discharge from hospital) [14/32 (44%) vs 116/528 (22%); p = 0.01] (Table 1). DCA patients had higher values of initial PETCO2 (53.2 ± 16.8 vs 15.8 ± 8.3 mmHg; p < 0.0001) and average PETCO2 (43.5 ± 13.8 vs 23.5 ± 8.2; p = 0.002).
Table 1.
Characteristics and resuscitation outcome in patients with OHPCA and drowning victims in cardiac arrest
| Drowning victims (n = 32) | Patients with OHPCA (n = 528) | p value | |
|---|---|---|---|
| Age | 46.5 ± 21.4 | 62.5 ± 15.8 | 0.01a |
| Gender (male)/all | 22 (69%) | 359 (68%) | 0. 98b |
| Bystander | 9 (28%) | 343 (65%) | 0.03b |
| Bystander CPR | 11 (34%) | 105 (20%) | 0.39b |
| Initial rhythm ASY+PEA/VF+VT | 29/3 | 297/231 | <0.0001b |
| Response time (min) | |||
| Call to team arrival (min) | 11 (4–24) | 6 (1–14) | 0.001a |
| Arrest to team arrival | 17 (9–28) | 9 (4–17) | 0.001a |
| Location of arrest at home/public place | 3/29 | 275/253 | <0.0001b |
| PETCO2 (mmHg) | |||
| Initial | 53.2 ± 16.8 | 15.8 ± 8.3 | <0.0001a |
| After 1 min of CPR | 28.9 ± 6.3 | 25.9 ± 5.8 | 0.78a |
| Average | 43.5 ± 13.8 | 16.5 ± 8.2 | 0.002a |
| Final | 28.6 ± 8.6 | 26.3 ± 9.4 | 0.86a |
| Alcohol, n (%) | 12 (38%) | 61 (12%) | 0.0002b |
| Initial core temperature (°C) | 32.8 ± 2.2 | 35.4 ± 1.9 | 0.02a |
| Suicide | 22 (69%) | 2 (0.4%) | <0.0001b |
| ROSC | |||
| ROSC in the field (%) | 21 (65%) | 301 (57%) | 0.33b |
| ROSC with admission to the hospital (%) | 19 (60%) | 253 (48%) | 0.27b |
| Survived (hospital discharge) (%) | 14 (44%) | 116 (22%) | 0.01b |
| Neurological outcome of survivers (CPC), n (%) | |||
| CPC 1 + CPC 2 | 12 (85%) | 71 (61%) | 0.08b |
| CPC 3 + CPC 4 | 2 (15%) | 39 (34%) | 0.22b |
| CPC 5 | – | 6 (5%) | |
ASY asystole, PEA pulseless electrical activity, VF ventricular fibrillation, VT ventricular tachycardia
aWilcoxon rank sum test
bFisher test
The analysis showed that DCA patients who survived were younger, had more bystander CPR, shorter call-arrival interval, higher values of PETCO2 after 1 min of CPR, higher average and final values of PETCO2, lower value of initial serum K+, and more of them received vasopressin (p < 0.05) in comparison with DCA patients who did not survive (Table 2).
Table 2.
Comparison of characteristics of survived (discharged from the hospital) and dead (died before discharge from the hospital) drowning victims in cardiac arrest
| Variables | Survived (hospital discharge) (n = 14) | Dead (n = 18) | p value |
|---|---|---|---|
| Age | 38.9 ± 12.6 | 56.6 ± 18.7 | 0.03a |
| Gender (M/F) | 10/4 | 13/5 | 0.98b |
| Bystander CPR | 8 (57%) | 3(17%) | 0.03b |
| Initial rhythm (PEA+ASY/VF+VT) | 13/1 | 18/2 | 0.98b |
| Call-arrival interval | 6 (4–10) | 10 (5–24) | 0.01a |
| Initial core temp. (°C) | 31.8 ± 1.7 | 32.6 ± 1.5 | 0.46a |
| PETCO2 (mmHg) | |||
| Initial | 56.8 ± 17.6 | 53.8 ± 15.8 | 0.86a |
| After 1 min | 34.3 ± 8.2 | 19.8 ± 8.6 | <0.01a |
| Average | 27.9 ± 7.5 | 18.7 ± 6.4 | 0.02a |
| Final | 31.2 ± 7.3 | 8.6 ± 3.4 | <0.01a |
| Initial serum potassium (mmol/l) | 6.8 ± 2.3 | 4.3 ± 1.3 | <0.01a |
| Vasopressin, n (%) | 9 (64%) | 4 (22%) | 0.03b |
PEA pulseless electrical activity, ASY asystole, VF ventricular fibrillation, VT ventricular tachycardia
aWilcoxon rank sum test
bFisher test
In multivariate analysis we found five independent factors for the increased chance of survival: time to arrival [odds ratio (OR): 1.27; 95% confidence interval (CI): 1.12–1.86; p < 0.01], PETCO2 after 1 min CPR (OR: 1.72; 95% CI: 1.32–2.72; p = 0.02), final PETCO2 (OR: 2.53; 95% CI: 1.82–3.55; p < 0.001), vasopressin (OR: 1.23; 95% CI: 1.09–1.85; p = 0.01), and potassium (OR: 3.45; 95% CI: 1.62–7.21; p < 0.001).
Discussion
The survival rate (patients discharged from hospital) among DCA patients was significantly higher that among OHPCA patients (44 vs 22%; p < 0.01). In a similar study Claesson et al. did not find a significant difference between these groups [4]. In our study very good overall survival in all patients and especially in DCA patients was found. Donoghue et al. [5] reported in a meta-analysis of 41 studies that the survival rate in pediatric patients is 28%. Claesson et al. found that 29% of patients were admitted to hospital (in our study 60%) and 12% of them survived. The presence of an emergency physician in the prehospital setting and application of vasopressin may well be associated with good outcomes (ROSC, admission to hospital, discharge from hospital) and are possible causes [6, 7].
Our study confirms the findings of studies by Claesson et al. and Kuisma et al. that drowning patients are younger and more of them are found in a nonshockable rhythm [asystole/pulseless electrical activity (PEA)] compared to OHPCA patients [1, 4, 8]. Younger patients have a lower incidence of comorbidity and/or greater potential for recovery [4, 5, 9]. DCA patients usually have a nonshockable initial rhythm (asystole/PEA) due to asphyxia after drowning that leads to myocardial hypoxia, which results in progressive bradycardia, finally deteriorating to asystole [1, 4, 9], or prolonged response time resulting in the disappearance of a shockable rhythm [4].
The analysis of PETCO2 values confirmed higher values in patients with ROSC and in patients who survived [6] as well as an asphyxial model of PETCO2 values in DCA patients [10]. In asphyxial model PETCO2 levels were initially high after the onset of arrest, then decreased to subnormal levels after 1–2 min, and then increased again during CPR to near-normal levels. These results confirmed asphyxia as a primary mechanism of cardiac arrest in DCA patients in our study.
In the DCA group 22 (68.8%) suicide (intentional) victims and 12 patients (37.5%) with alcohol intoxications were found [11]. Ten intoxicated patients drowned by accident. The share of intoxicated patients is relatively high in comparison with other reports about drowning [1, 12, 13]. In Slovenia suicide and alcohol intoxication are the leading causes of drowning.
Significantly fewer DCA patients are witnessed than those suffering from OHPCA [4, 9]. In our study there is a high percentage of suicide victims and therefore the probability that the drowning is witnessed is small. On the other hand, more cases of bystander CPR administered to drowning victims were observed (and paradoxically, the number of bystander CPR is higher than the number of witnessed drownings). Probably bystanders easily interpret the emergency situation and action needed in drowning victims than in primary cardiac arrest (evident mechanism of arrest and symptoms) [4]. It is possibly due to the nature of data collection (retrospective chart review) and that data were not entered correctly at the time (limitations of retrospective reviews, irrespective of Utstein style protocol).
The response time (call to arrival of team and arrest to start of CPR) was significantly longer in DCA patients. The primary reasons for the longer response time were: difficult access to the victims (technical rescue) and high number of unwitnessed arrests (suicidal victims). Kuisma et al. [14] reported that a response time of 7 min or more is a cutoff point for survival in patients with arrest of noncardiac origin.
Nevertheless, the ROSC and ROSC with admission were better in DCA patients and the survival rate is significantly higher in DCA. DCA victims had significantly lower core temperatures. Drowning in cool water appears to have a favorable impact and can be mainly explained by the neuroprotective effects of rapid brain cooling (in our study a better neurological outcome was found in DCA patients) [8, 14, 15].
The data collected in some studies [9, 17, 18] suggest that the serum potassium levels may be of value for outcome prediction in DCA patients (hemolysis with hyperkalemia).
Oehmichen et al. [16] explained that in contrast to clinical laboratory findings in experimental drowning of animals (erythrocyte lysis, hyperkalemia, and final cardiac fibrillation) the observations in drowned humans (increase of pCO2, hypoxic encephalopathy) lead to a different pathophysiological interpretation of the drowning process. In their study nearly all cases (96%) revealed a reduction of pH due to hypoxic acidosis, and only two cases (6.5%) exhibited a slight hyperkalemia. As a result of their investigation they had to state that the lack of hyperkalemia as well as of an increase of the hemoglobin level indicate that there is no distinct intravascular red cell lysis due to influx of water into the vascular compartment. Therefore, death by drowning in humans is in most cases the result of a hypoxic cerebral process.
The values of PETCO2 from our study suggest that asphyxia and hypoxia are the primary processes of death, although hyperkalemia can impair survival.
Our recent study [7] confirmed that resuscitated patients treated with vasopressin alone or followed by epinephrine have higher average and final end-tidal carbon dioxide values as well as a higher mean arterial pressure (MAP) on admission to the hospital than patients treated with epinephrine only. This combination of vasopressor therapy is associated with restoration of spontaneous circulation, short-term survival, and neurological outcome. In the subgroup of patients with initial rhythm asystole, it improves the hospital discharge rate. Lienhart et al. [19] and Sumann et al. [20] reported that vasopressors could be useful to restore spontaneous circulation in hypothermic cardiac arrest patients prior to rewarming, thus avoiding prolonged mechanical CPR efforts or use of extracorporeal circulation. Compared with epinephrine, vasopressin exerts greater vasoconstriction in hypoxic and acidotic conditions [21]. It may also support previous experience that the combination of both epinephrine and vasopressin may be necessary to achieve the vasopressor response needed for restoration of spontaneous circulation, especially after asphyxial cardiac arrest or during prolonged CPR efforts.
Conclusion
DCA patients had a better survival rate (discharge from hospital), higher initial and average PETCO2 values, and more of them had a nonshockable initial rhythm. Survival (discharge from hospital) in DCA patients is associated with the PETCO2 values, initial serum K+ values, application of vasopressin, and ambulance response time.
Acknowledgments
Conflicts of interest None.
Abbreviations
- ALS
Advanced life support
- CI
Confidence interval
- CPR
Cardiopulmonary resuscitation
- DCA
Drowning victims in cardiac arrest
- ERC
European Resuscitation Council
- ILCOR
International Liaison Committee on Resuscitation
- MAP
Mean arterial pressure
- OHPCA
Out-of-hospital primary cardiac arrest
- PETCO2
Partial pressure of end-tidal CO2
- OR
Odds ratio
- PEA
Pulseless electrical activity
- ROSC
Return of spontaneous circulation
- USFD
Utstein Style for Drowning
- VF
Ventricular fibrillation
- VT
Ventricular tachycardia
Biography
Štefek Grmec has gathered clinical experience in the last 15 years and focused his scientific and research interests on the areas of emergency medicine (in general), organization of emergency medical services, difficult intubation and airway in the field, capnometry and capnography in CPR and shock, acute medicine and family practice, trauma in the prehospital setting, severe head injury in the prehospital setting, RSI, vasopressin, erythropoietin in CPR, echocardiography in the prehospital setting, cardiac biomarkers in heart failure, and ultrasound. He has concluded postgraduate study (4 years) of emergency and intensive medicine. His contributions were published in the following journals: Intensive Care Medicine, European Journal of Emergency Medicine, Critical Care, Emergency Medicine Journal, Academic Emergency Medicine, Prehospital and Disaster Medicine, Acta Anaesthesiologica Scandinavica, and Critical Care Medicine. He has published about 300 scientific contributions.
Footnotes
Disclaimer: The views expressed in this paper are those of the author(s) and not those of the editors, editorial board or publisher.
Contributor Information
Štefek Grmec, Phone: +386-51-394806, Email: grmec-mis@siol.net.
Matej Strnad, Phone: +386-51-225448, Email: strnadmatej@yahoo.com.
Dejan Podgoršek, Phone: +386-40-774774, Email: dejan.podgorsek@triera.net.
References
- 1.Anonymous Drowning. Circulation. 2005;112:IV-133–IV-135. doi: 10.1161/CIRCULATIONAHA.105.166565. [DOI] [Google Scholar]
- 2.Idris AH, Berg RA, Bierens J, Bossaert L, Branche CM, Gabrielli A, Graves SA, Handley AJ, Hoelle R, Morley PT, Papa L, Pepe PE, Quan L, Szpilman D, Wigginton JG, Modell JH, American Heart Association. Maatschappij tot Redding van Drenkelingen. European Resuscitation Council. US Centers for Disease Control and Prevention. University of Florida. University of North Carolina. Australia and New Zealand Resuscitation Council. InterAmerican Heart Foundation. Heart and Stroke Foundation of Canada. Resuscitation Council of Southern Africa Recommended guidelines for uniform reporting of data from drowning: the “Utstein style”. Resuscitation. 2003;59:45–57. doi: 10.1016/j.resuscitation.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 3.Raina KD, Callaway C, Rittenberger JC, Holm MB. Neurological and functional status following cardiac arrest: method and tool utility. Resuscitation. 2008;79(2):249–256. doi: 10.1016/j.resuscitation.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Claesson A, Svensson L, Silfverstolpe J, Herlitz J. Characteristics and outcome among patients suffering out-of-hospital cardiac arrest due to drowning. Resuscitation. 2008;76:381–387. doi: 10.1016/j.resuscitation.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 5.Donoghue AJ, Nadkarni V, Berg RA, Osmond MH, Wells G, Nesbitt L, Stiell IG, CanAm Pediatric Cardiac Arrest Investigators Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. 2005;46:512–522. doi: 10.1016/j.annemergmed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 6.Grmec Š, Križmarić M, Mally S, Koželj A, Špindler M, Lešnik B. Utstein style analysis of out-of-hospital cardiac arrest—bystander CPR and end expired carbon dioxide. Resuscitation. 2007;72:404–414. doi: 10.1016/j.resuscitation.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Mally Š, Jelatancev A, Grmec Š. Effects of epinephrine and vasopressin on end-tidal carbon dioxide tension and mean arterial blood pressure in out-of-hospital cardiopulmonary resuscitation; an observational study. Crit Care. 2007;11:R39. doi: 10.1186/cc5726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engdahl J, Bång A, Karlson BW, Lindqvist J, Herlitz J. Characteristics and outcome among patients suffering from out of hospital cardiac arrest of non-cardiac aetiology. Resuscitation. 2003;57:33–41. doi: 10.1016/S0300-9572(02)00433-1. [DOI] [PubMed] [Google Scholar]
- 9.Eich C, Bräuer A, Timmermann A, Schwarz SK, Russo SG, Neubert K, Graf BM, Aleksic I. Outcome of 12 drowned children with attempted resuscitation on cardiopulmonary bypass: an analysis of variables based on the “Utstein Style for drowning”. Resuscitation. 2007;75:42–52. doi: 10.1016/j.resuscitation.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Grmec Š, Lah K, Tušek-Bunc K. Difference in end-tidal CO2 between asphyxia cardiac arrest and ventricular fibrillation/pulseless ventricular tachycardia cardiac arrest in the prehospital setting. Crit Care. 2003;7:R139–R144. doi: 10.1186/cc2369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Driscoll TR, Harrison JE, Steenkamp M. Alcohol and drowning in Australia. Inj Control Saf Promot. 2004;11:175–181. doi: 10.1080/156609704/233/289661. [DOI] [PubMed] [Google Scholar]
- 12.Gorniak JM, Jenkins AJ, Felo JA, Balraj E. Drug prevalence in drowning deaths in Cuyahoga County, Ohio: a ten-year retrospective study. Am J Forensic Med Pathol. 2005;26:240–243. doi: 10.1097/01.paf.0000176280.74666.ab. [DOI] [PubMed] [Google Scholar]
- 13.Gulliver P, Begg D. Usual water-related behaviour and ‘near-drowning’ incidents in young adults. Aust N Z J Public Health. 2005;29:238–243. doi: 10.1111/j.1467-842X.2005.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 14.Kuisma M, Alaspää A. Out-of-hospital cardiac arrests of non-cardiac origin. Epidemiology and outcome. Eur Heart J. 1997;18:1122–1128. doi: 10.1093/oxfordjournals.eurheartj.a015407. [DOI] [PubMed] [Google Scholar]
- 15.Golden F. Mechanisms of body cooling in submersed victims. Resuscitation. 1997;35(2):107–109. doi: 10.1016/S0300-9572(97)00065-8. [DOI] [PubMed] [Google Scholar]
- 16.Suominen P, Baillie C, Korpela R, Rautanen S, Ranta S, Olkkola KT. Impact of age, submersion time and water temperature on outcome in near-drowning. Resuscitation. 2002;52(3):247–254. doi: 10.1016/S0300-9572(01)00478-6. [DOI] [PubMed] [Google Scholar]
- 17.Oehmichen M, Henning R, Meissner C. Near-drowning and clinical laboratory changes. Leg Med (Tokyo) 2008;10:1–5. doi: 10.1016/j.legalmed.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 18.Orlowski JP, Szpilman D. Drowning. Rescue, resuscitation, and reanimation. Pediatr Clin North Am. 2001;48:627–646. doi: 10.1016/S0031-3955(05)70331-X. [DOI] [PubMed] [Google Scholar]
- 19.Lienhart HG, John W, Wenzel V. Cardiopulmonary resuscitation of a near-drowned child with a combination of epinephrine and vasopressin. Pediatr Crit Care Med. 2005;6:486–488. doi: 10.1097/01.PCC.0000163673.40424.E7. [DOI] [PubMed] [Google Scholar]
- 20.Sumann G, Krismer AC, Wenzel V, Adelsmayr E, Schwarz B, Lindner KH, Mair P. Cardiopulmonary resuscitation after near drowning and hypothermia: restoration of spontaneous circulation after vasopressin. Acta Anaesthesiol Scand. 2003;47:363–365. doi: 10.1034/j.1399-6576.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- 21.Wenzel V, Lindner KH, Krismer AC, Miller EA, Voelckel WG, Lingnau W. Repeated administration of vasopressin but not epinephrine maintains coronary perfusion pressure after early and late administration during prolonged cardiopulmonary resuscitation in pigs. Circulation. 1999;99:1379–1384. doi: 10.1161/01.cir.99.10.1379. [DOI] [PubMed] [Google Scholar]