Fig. 1.
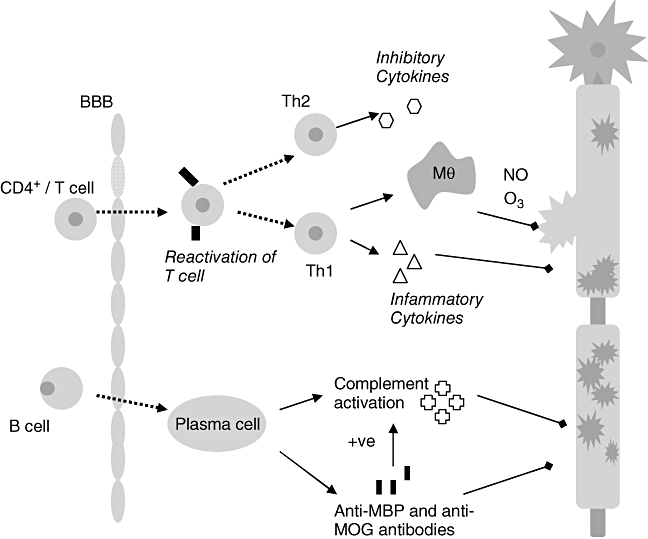
The pathogenic cascade in multiple sclerosis (MS): the initiation of inflammation central to the pathogenesis of MS depends on the peripheral activation of T cells via foreign antigens. Activated T cells express integrins which bind to up-regulated cell adhesion molecules on the blood–brain barrier (BBB) endothelial surface allowing diapedesis of T cells into the central nervous system (CNS). Within the CNS T cells re-encounter specific antigen and are reactivated setting up an inflammatory cascade which results in conduction block and demyelination. Myelin and axon damage is dependent on various effector mechanisms; the extent of involvement of each is thought to vary between individuals. Activated T cells bind directly to myelin epitopes leading to activation of macrophages (Mθ) which can phagocytose myelin directly or, along with T cells and glial cells, can release cytotoxic products and mediators such as proteases [122], inflammatory cytokines, e.g. tumour necrosis factor-α, interferon-γ[123], soluble reactive oxygen (03) and nitrogen (NO) intermediates [124,125], free radicals and glutamic acid. Further attack to myelin comes from antibodies and complement components – mainly the terminal complement complex – C5b–9 [126] triggered principally by infiltrating B cells and myelin antibodies.
