Abstract
Susceptibility and lethality studies of inhalational tularaemia were undertaken using the common marmoset (Callithrix jacchus) to determine its suitability as a non-human primate model. Pairs of marmosets were exposed to varying challenge doses of Francisella tularensis by the airborne route and monitored for up to 14 days postchallenge (p.c.). Lethal infection was achieved following a retained dose of less than 10 bacterial colony-forming units (CFU). However, precise LD50 determination was not possible. The model was characterized using a target challenge dose of approximately 100 CFU. Increased core body temperature was the first indicator of disease, at approximately 2.5 days p.c. Overt clinical signs were first observed 12–18 h after the temperature increase. Significantly decreased activity was observed after approximately 3 days. All animals succumbed to infection between 4.5 and 7 days p.c. At postmortem examination, gross pathology was evident in the liver, spleen and lungs of all animals and high bacterial numbers were detected in all the organs assessed. Bacteraemia was demonstrated in all animals postmortem. Histopathological observations included severe suppurative bronchopneumonia, severe multifocal pyogranulomatous hepatitis, splenitis and lymphadenitis. Tularaemia disease progression in the common marmoset therefore appears to be consistent with the disease seen in humans and other animal models. The common marmoset may therefore be considered a suitable model for further studies of inhalational tularaemia.
Keywords: Francisella tularensis, inhalation, marmoset, tularaemia
Francisella tularensis is a Gram-negative intracellular pathogen and the causative agent of tularaemia. Disease is prevalent in many countries in the northern hemisphere (Ellis et al., 2002). Because of its high infectivity and virulence, F. tularensis has been developed previously for use as a bioweapon (Dennis et al., 2001) and is considered a Category A agent on the Centers for Disease Control and Prevention threat lists (CDC 2008).
In order to determine the efficacy of pre- or postexposure therapies, there is a need to develop and characterize animal models of inhalational tularaemia. A number of animal models have been studied for these purposes (Lyons & Wu 2007). To date most research has focused on the development of murine models of infection (Chen et al. 2003; Conlan et al. 2003). Such work has increased the understanding of disease progression and identified important immunological responses to infection. In order to undertake the pivotal studies, however, that would be required for licensure of any therapy, non-human primate (NHP) models of infection are likely to be required. Early work, undertaken during 1960s and 1970s, used the rhesus macaque (Macaca mulatta) to model tularaemia pathogenesis (Tulis et al. 1970; Day & Berendt 1972; Schricker et al. 1972; Hall et al. 1973). Studies evaluating medical countermeasures such as antibiotics (Sawyer et al. 1966), and the efficacy of the live vaccine strain (LVS) tularaemia vaccine (Eigelsbach et al. 1962; Tulis et al. 1969) were also undertaken in the rhesus macaque. Some antibiotic evaluation was undertaken using vervet monkeys (Baskerville et al. 1978). These studies suggested that NHPs were representative models of the disease processes seen in human cases of tularaemia infection. However, many gaps in experimental data still exist.
The current study focused on determining whether reproducible inhalational tularaemia infection could be experimentally induced in the common marmoset (Callithrix jacchus), a New World NHP species, followed by the subsequent characterization of disease. The marmoset presents a number of ethical and practical advantages over other NHP species because of its small size (approximately 400 g), particularly with the need to handle infected, sick animals within biocontainment. Reports from the literature also suggested that the marmoset might be susceptible to tularaemia infection, following two naturally occurring infections in captive marmosets (Posthaus et al. 1998; Splettstoesser et al. 2007).
Materials and methods
Animals
Healthy, sexually mature common marmosets (C. jacchus) were obtained from the Dstl Porton Down breeding colony and housed in vasectomized male and female pairs. Animals were aged between 18 and 61 months, and weighed between 360 and 484 g at the time of challenge. The animals were allowed free access to food and water as well as environmental enrichment. Prior to use in challenge studies, all animals were surgically implanted intra-peritoneally with a Remo 200 device, under general anaesthesia (ketamine/isofluorane), to record core body temperature (Tc) (Remo Technologies Ltd, Salisbury, UK). Data were transmitted from the devices at 10-s intervals to locally placed antennas and relayed to receivers. Data were analysed using the eDacq software to provide real-time and recordable Tc (EMMS, Bordon, Hampshire, UK). In one study, both animals had Actiwatch®-Mini devices (Cambridge Neurotechnology Ltd, Cambridge, UK) attached to their collars to monitor activity. All animal studies were carried out in accordance with the UK Animals (Scientific Procedures) Act of 1986 and the Codes of Practice for the Housing and Care of Animals used in Scientific Procedures 1989.
Housing
Animal rooms were maintained at 25 °C on a 12-h light/dark cycle with 30-min ‘dawn’ and ‘dusk’ periods. Animals were fed 20 g of primate pellets (Special Diet Services, Withham, Essex, UK) each day supplemented by fruit (orange, apple, banana). In addition, 1–2 tablespoons of forage mix consisting of cereal, raisins and sunflower seeds were given daily. Animals had unlimited access to water at all times.
Prior to challenge, animals were transferred to animal containment level 3 (CL3) conditions (US Biosafety level 3) and housed within purpose built cages within a half-suit isolator compliant with British Standard BS5726. Animals were acclimatized to their new environment for a minimum of 3 days to obtain baseline temperature data. Following the challenge, animals were monitored at 8-h intervals until the onset of clinical signs at which time they were monitored at 4-h intervals. At each observation period, temperature and clinical signs such as posture, respiration (visual check), condition of coat, behaviour and locomotion were recorded. Animals were humanely culled wherever possible based on an assessment of the criteria above.
Bacterial strain and culture
Glycerol stocks of F. tularensis strain SCHU S4 were obtained from DynPort Vaccine Company LLC (DVC) (Frederick, Maryland, USA). Bacteria were recovered from the vial onto blood cysteine glucose agar (BCGA) plates and incubated at 37 °C for 48 h, prior to recovery into phosphate-buffered saline (PBS), pH 7.3. The optical density reading (OD590) of the suspension was adjusted to 0.1, equivalent to approximately 1 × 108 CFU/ml, 1 ml of which was used to inoculate 100 ml of modified cysteine partial hydrolysate broth (MCPH). The broth was shaken at 180 rpm for 48 h. Prior to challenge, the OD590 of the culture was adjusted to 0.1 and serially diluted to the appropriate concentration for challenge. Viable counts were performed on BCGA retrospectively to determine the actual value. All procedures were carried out at ACDP CL3 in class 3 microbiological safety cabinets compliant with British Standard BS5726.
Challenge
Marmosets were anaesthetised with 25 mg/kg ketamine intra-muscularly prior to exposure and were challenged either singly or in pairs by the airborne route (Lever et al. 2008). Briefly, a collison nebulizer containing 20 ml F. tularensis and three drops of Antifoam 289 (Sigma, Poole, UK) was used to generate aerosol particles of approximately 1–3 μm. The aerosol was conditioned in a modified Henderson apparatus (Druett 1969). Marmosets were placed in a head-only exposure chamber (plethysmograph tube) and exposed for 10 min to a dynamic aerosol maintained at 50–55% relative humidity and 18–20 °C. The total accumulated tidal volume for each animal during challenge was determined by whole body real-time plethysmography with a Fleisch pneumotacograph (EMMS, Bordon, Hampshire, UK). The concentration of the aerosol cloud was quantified after sampling from a sample port into an all glass impinger (AGI-30) by serial dilution and plating onto BCGA.
In order to determine the LD50, the Dixon staircase method for small samples (Dixon & Fotheringham 1993) was employed. A log increase or decrease in colony-forming units (CFU) was to be used for each step-up or step-down stage, starting from a target estimated susceptible dose of approximately 100 CFU. This was based on a reported LD50 of 14 CFU in macaques (Day & Berendt 1972). Steps 1 and 2 of the study progressed as planned, however, because of the low infectivity of the bacteria, step 3 consisted of three experiments at a target dose of 100 CFU.
Postmortem examinations were performed on all animals upon humanely culling or immediately after they were found dead. Organs were removed and assessed for gross pathology, bacteriology and histology. Blood was removed from anaesthetized marmosets at postmortem by cardiac puncture for the assessment of bacteraemia.
Bacteriology
At postmortem examination, bacterial loads in the blood, liver, spleen, kidneys and lungs were assessed. Weighed organ sections (approximately 50% of tissue) were removed aseptically and homogenized in 5 ml PBS using cell sieves and a plunger. Homogenates and blood were serially diluted in PBS and appropriate dilutions were sub-cultured onto BCGA plates, which were incubated at 37 °C for 72 h prior to enumeration. Bacterial counts were expressed as CFU/g tissue or CFU/ml of blood.
Histopathological studies
Tissues were fixed in 10% buffered formalin solution and processed for paraffin wax embedding using standard techniques. Sections (5 ± 2 μm) were cut and stained with haematoxylin and eosin.
Statistics
Pearson's correlation analysis was used to determine the relationship of gender, body weight, time to death and inhaled dose. Analysis of variance for square roots was used to determine the relationship between body temperature data and activity data pre- and postexposure.
Results
Challenge dose determination, susceptibility – step 1
To determine the susceptibility of marmosets to F. tularensis infection, two animals were exposed to an aerosol containing target doses of 1.8 × 102 CFU/l [male (M)] or 2.8 × 102 CFU/l [female (F)] (Table 1). The actual doses received were not determined in this case, but were estimated to be in the region of 200–400 CFU. An increase in Tc at 60 h (M) and 62 h (F) postchallenge (p.c.) was the first indication of disease. The Tc continued to increase steadily for approximately 16 h, reaching approximately 41.5 °C (normally approximately 39 °C). This high temperature was then maintained until the point of death. Further signs of infection appeared at 3 (M) or 4 days (F) p.c. Both animals became more subdued and exhibited piloerection, followed by a visible abnormal respiration rate around day 4 p.c. Throughout this p.c. period, both animals remained alert and responsive to external stimuli such as food treats. Approximately 1–2 h prior to death, both animals showed reddening of the face. Both animals died at approximately 5.5 days p.c. (133.5 and 132.5 h for the male and female respectively).
Table 1.
Summary of animal weight, age, plethysmography data, exposure dose and time to death data
| Step (Dixon method) | Gender | Age (years) | Body weight (g) | Accumulative volume (l) | Aerosol concentration (CFU/l) | Inhaled dose (CFU) | Time to death [hours (days)] |
|---|---|---|---|---|---|---|---|
| Step 1 | M | 5.1 | 400 | NA | 180 | NA | 133.5 (5.5) |
| F | 3.3 | 382 | NA | 280 | NA | 132.5 (5.5) | |
| Step 2 | M | 3.4 | 364 | 0.5 | 17 | 9 | 204 (8.5) |
| F | 2.0 | 360 | 0.2 | 18 | 4 | 319 (13) | |
| Step 3 | M | 3.3 | 364 | 0.9 | 44 | 40 | 107 (4.5) |
| F | 1.6 | 484 | 1.0 | 65 | 66 | 120 (5) | |
| M | 3.3 | 410 | 2.0 | 130 | 260 | 118 (5) | |
| F | 1.5 | 398 | 0.9 | 150 | 130 | 167 (7) | |
| M | 5 | 404 | 0.9 | 190 | 180 | 162 (6.5) | |
| F | 2.2 | 380 | 1.5 | 190 | 300 | 105 (4.5) |
NA, not available.
Macroscopically, there was extensive gross pathology in the lungs of both animals, characterized by large areas of haemorrhage or discrete hardened nodules (Table 2). Small lesions were seen in the spleens, with a few lesions apparent in the liver of one animal. No gross pathology was evident in the kidneys of either animal. Histopathology in both animals indicated severe suppurative bronchopneumonia and severe multifocal pyogranulomatous hepatitis, splenitis and lymphadenitis (Figures 1–4). The liver, spleen, lung and lymph tissue all showed evidence of neutrophils, lymphocytes and macrophages infiltration in the parenchyma and neutrophil degeneration.
Table 2.
Gross pathology observed at postmortem, in marmosets infected with Francisella tularensis by the airborne route
| Number affected | |||||
|---|---|---|---|---|---|
| Challenge step | Organ | Lesion | Enlargement | Haemorrhagic lesion | Discolouration |
| Step 1 (n = 2) | Liver | 1 | 2 | 0 | 0 |
| Spleen | 2 | 2 | 0 | 0 | |
| Kidney | 0 | 0 | 0 | 0 | |
| Lungs | 1 | 2 | 1 | 0 | |
| Step 2 (n = 2) | Liver | 2 | 2 | 0 | 0 |
| Spleen | 1 | 0 | 0 | 1 | |
| Kidney | 0 | 0 | 0 | 0 | |
| Lungs | 0 | 1 | 1 | 0 | |
| Step 3 (n = 6) | Liver | 1 | 3 | 0 | 1 |
| Spleen | 2 | 6 | 0 | 2 | |
| Kidney | 0 | 0 | 0 | 0 | |
| Lungs | 1 | 4 | 6 | 1 | |
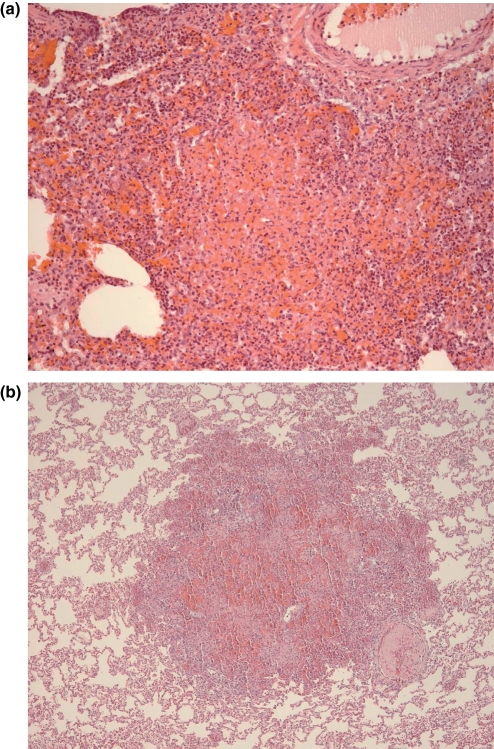
Figure 1.
Haematoxylin and eosin stained lung section from a marmoset challenged with approximately 400 CFU of Francisella tularensis by the airborne route. (a) Suppurative pneumonia with necrosis and haemorrhage (200× magnification). (b) Dense of foci of pyogranulomatous pneumonia with infiltration of neutrophils, macrophages and lymphocyes and areas of haemorrhages (100× magnification).
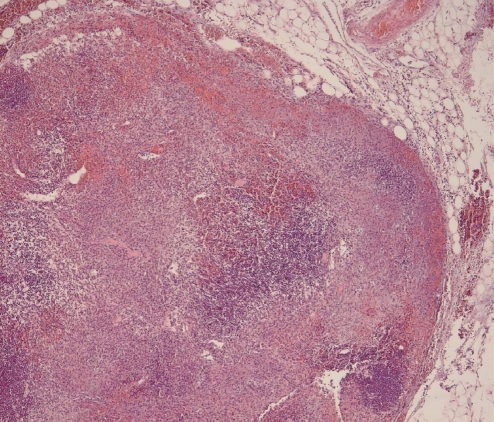
Figure 4.
Haematoxylin and eosin stained lymph node section from a marmoset challenged with approximately 400 CFU of Francisella tularensis by the airborne route. Evidence of mulifocal to coalescent pyogranulomatous lymphadentidtis with abundant necrosis predominantly in the outer cortex (40× magnification).
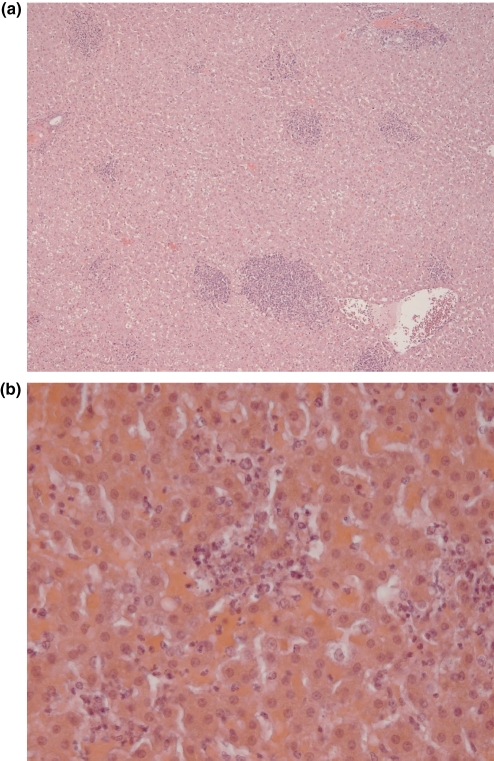
Figure 2.
Haematoxylin and eosin stained liver section from a marmoset challenged with approximately 400 CFU of Francisella tularensis by the airborne route. (a) Multifocal microabscesses (40× magnification). (b) Evidence of multifocal infiltration of neutrophils within the liver parenchyma, mostly degenerative microabscesses (400× magnification).
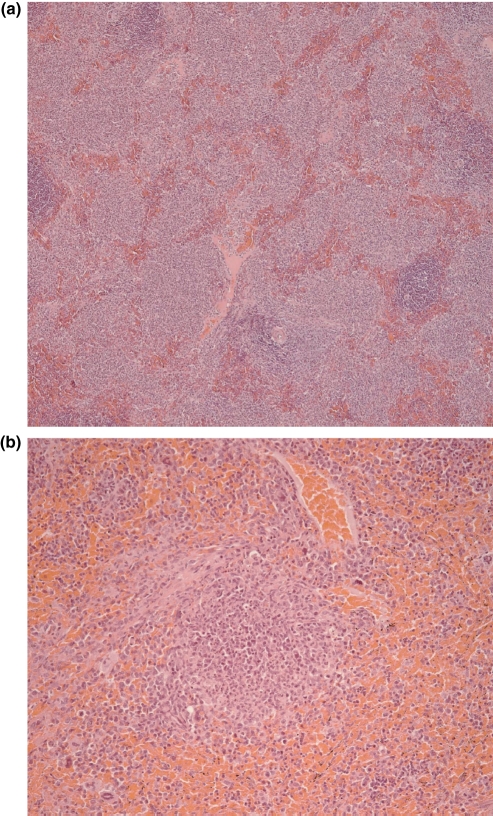
Figure 3.
Haematoxylin and eosin stained spleen section from a marmoset challenged with approximately 400 CFU a Francisella tularensis by the airborne route. (a) Multifocal microabscesses in the red pulp (40× magnification). (b) Evidence of pyogranulomatous splenitis (200× magnification).
At postmortem examination, the highest concentrations of bacterial cells were recovered from the spleens of both animals, followed by blood, lungs, liver and kidneys (Table 3).
Table 3.
Summary of the bacterial numbers recovered from marmoset organs at postmortem
| Bacterial count (CFU/g of tissue or CFU/ml of blood) | ||||||
|---|---|---|---|---|---|---|
| Challenge step | Gender | Liver | Spleen | Kidney | Lungs | Blood |
| Step 1 | M | 9.9 × 106 | 1.6 × 1013 | 5.3 × 105 | 6.6 × 106 | 2.4 × 107 |
| F | 2.5 × 106 | 2.8 × 1010 | 1.6 × 105 | 3.0 × 108 | 2.7 × 107 | |
| Step 2 | M | 2.8 × 107 | 2.7 × 1010 | 8 × 104 | 2.1 × 107 | 3.9 × 105 |
| F | 5.4 × 105 | 5.9 × 105 | 7.6 × 104 | 6.4 × 107 | 4.6 × 105 | |
| Step 3 | M | 4.6 × 108 | 3.7 × 109 | 9 × 105 | 5.4 × 107 | 2.8 × 109 |
| F | 8.9 × 108 | 1.3 × 107 | 1.5 × 105 | 6.1 × 107 | 1.5 × 104 | |
| M | 5.5 × 106 | 3.4 × 109 | 6.4 × 104 | 5.4 × 106 | 1.4 × 105 | |
| F | 2.5 × 107 | 1.3 × 107 | 1.1 × 106 | 9.1 × 108 | 5.0 × 104 | |
| M | 3.7 × 106 | 2.7 × 107 | 1.6 × 107 | 8.4 × 106 | 2.7 × 107 | |
| F | 1.1 × 107 | 5.4 × 108 | 3.4 × 106 | 4.3 × 106 | 3.2 × 106 | |
| Step 3 summary | 2.3 × 108 ± | 1.3 × 109 ± | 3.6 × 106 ± | 1.7 × 108 ± | 4.72 × 108 ± | |
| n = 6 (mean ± SEM) | 1.5 × 108 | 7.2 × 108 | 2.5 × 106 | 1.6 × 108 | 4.7 × 108 | |
SEM is the standard error of the mean.
Organ counts are expressed as CFU/g of tissue and blood counts as CFU/ml of blood.
Challenge dose determination – step 2
A second pair of animals was exposed to an aerosol containing a lower dose of F. tularensis (17 or 18 CFU/l) with calculated inhaled doses of 4 (F) and 9 CFU (M). Both animals died, although an increase in the time to death was observed. In the female, Tc rose at 80 h p.c. and continued to increase slowly, reaching 42 °C at 120 h. Tc was then maintained at approximately 41 °C until the animal was humanely culled at 13 days p.c. In the male, a raised Tc occurred at 124 h and was maintained at around 41.5 °C until death at 8.5 days. Overt clinical signs were apparent at 6.5 and 7 days p.c. with both animals appearing subdued and exhibiting piloerection and unsteadiness. The male showed a visible variable rate of respiration at around 7 days p.c. but there were no further changes in clinical signs in the female until the animal became unresponsive and was humanely culled.
Postmortem examination revealed extensive areas of haemorrhage in the lungs of both animals (Table 2). Splenomegaly was evident in both animals, but there was an absence of lesions. The spleen of the female, however, did exhibit some pale discolouration. Lesions were apparent in the liver of both animals. No evidence of gross pathology was observed in the kidneys of either animal.
Histopathological changes were similar to those of the previous pair of animals (step 1), with the presence of hepatitis, splenitis and lymphadenitis. The presentation of pneumonia, however, differed between the two step 2 animals. The animal culled at day 13 exhibited severe suppurative pneumonia, whereas the animal found dead after 8.5 days exhibited a mild interstitial pneumonia only.
Bacterial counts are shown in Table 3. Much higher counts were recovered from the liver and spleen in the male, but the two animals had similar counts recovered from lung, kidney and blood.
Challenge dose characterization – step 3
A challenge dose of less than 10 CFU had proved lethal in both animals in step 2, therefore it was decided that the establishment of a precise LD50 value using the staircase method would be impractical. The characterization of the infection at a challenge dose of approximately 100 CFU and the establishment of the reproducibility of the model by performing three replicate paired marmoset challenges at this challenge dose was undertaken.
The calculated dose varied according to the specific inhaled volumes; however, an average of 163 ± 39 CFU was achieved (Table 1). The time to death for these animals ranged between 4.5 and 7 days, with a mean time to death of 5.2 ± 0.4 days p.c. There were no significant correlations between gender, body weight, time to death or inhaled dose.
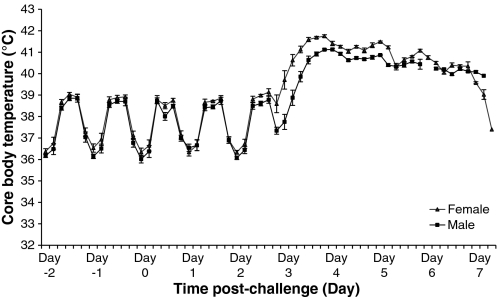
Normal marmoset Tc varied by approximately 3–4 °C because of circadian rhythms, with a higher body temperature of around 39 °C during the active day and around 36 °C during the inactive night (Figure 5). After airborne challenge, with a target dose of approximately 100 CFU F. tularensis strain SCHU S4, there were no significant rises in Tc for approximately 2.5 days p.c. At approximately 63 h p.c., there were significant rises in Tc, independent of gender (P < 0.0001). The temperature remained elevated for approximately 19.5 ± 2.2 h at approximately 41 °C until the animals either died or were humanely culled because of other signs of severe infection.
Figure 5.
The core body temperature of male (n = 3) and female marmosets (n = 3) challenged with approximately 100 CFU of Francisella tularensis by the airborne route at day 0. Error bars represent the standard error of the mean temperature during each 4 h period.
There was a progression of overt clinical signs of infection following the observed temperature increases. Animals initially became subdued in nature, followed by piloerection and unsteadiness or slowness in movement at around 3.5–4 days p.c. Three out of six animals showed a visible change in their respiration rate and/or reddening of face from approximately 12 h prior to death.
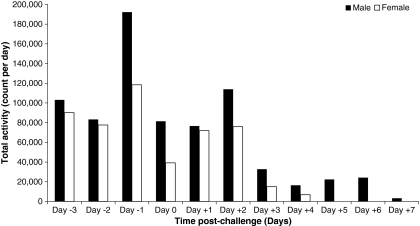
Two animals were also fitted with Actiwatch®-Mini devices to monitor activity. These devices have been used previously with marmosets and were well tolerated by the animals (Mann et al. 2005). Prior to challenge, the normal activity of each animal was determined (Figure 6). The activity counts were similar for 2 days p.c., however, on day 3 p.c., the overall activity of both animals decreased. The total daily activity count continued to decrease until the point of death. Overall, there was a significant difference in the activity of the animals pre- and postchallenge (P = 0.003). During this period, however, there was an increase in the activity during the night period (lights out period between 20:30 and 07:30 hours) (data not shown).
Figure 6.
Total daily spontaneous activity of two marmosets pre-and postexposure to approximately 100 CFU of Francisella tularensis strain SCHU S4 by the airborne route. Each 24 h period runs from 0000 to 2350.
At postmortem, the lungs and spleens were the organs most affected. Macroscopically, there was evidence of haemorrhagic lung lesions and splenomegaly in all animals. In addition, 33% of the spleens had lesions (Table 2). One animal exhibited some discolouration of the liver but no gross pathology was evident in the kidneys of any of the animals.
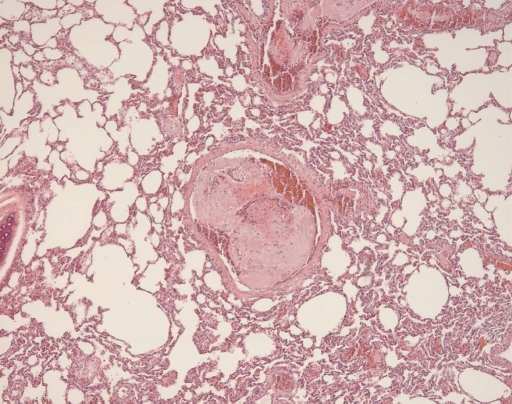
Histopathological observations were similar to those seen in the animals from step 1 and were characterized by severe suppurative bronchopneumonia, severe multifocal pyogranulomatous hepatitis, splenitis and lymphadenitis. Intravascular thrombi of the pulmonary arterioles were observed in all animals that died from infection (steps 1–3) (Figure 7).
Figure 7.
Haematoxylin and eosin stained lung section from a marmoset challenged with approximately 400 CFU of Francisella tularensis by the airborne route. Evidence of intravascular thrombi only observed in animals that had died from infection (100× magnification).
High numbers of bacterial cells were recovered from all organs at postmortem, with the lowest concentrations isolated from the kidneys (Table 3).
Discussion
The susceptibility of the common marmoset to airborne infection of F. tularensis, including the lethal nature of the infection, has been demonstrated. Very few inhaled bacteria were required to cause lethal infection, and as a result, a precise LD50 value could not be determined. Our data suggest that the LD50 value of airborne F. tularensis in the common marmoset is between 1 and 10 CFU. Low LD50 values for F. tularensis in systemic and airborne murine models of infection, of approximately 10–20 CFU have been reported (Conlan et al. 2003). Our results are also consistent with the low LD50 values reported previously in rhesus macaques (approximately 14 CFU) (Day & Berendt 1972) and low infectivity in humans (Saslaw et al. 1961), although the LD50 for humans is not known. The low LD50 reported in this study has provided supporting evidence that the marmoset is highly susceptible to F. tularensis by the airborne route and may be a relevant and comparable model of tularaemia.
As it was not possible to determine an LD50 for F. tularensis in the marmoset, work focused on characterizing the course of the disease following a challenge dose of approximately 100 CFU. In addition, two methods of remote monitoring were employed. Animals were surgically implanted with telemetry devices, to measure the Tc of animals, and, in one study (step 3, third repeat), the use of collar based actimetry devices to measure spontaneous activity. This allowed for real-time continuous monitoring of animals, which reduced both handling stress to the animals and hazards involved with handling infected animals.
During the initial 2.5 days postchallenge, animals exhibited normal behaviour with no apparent signs of infection and a normal diurnal Tc pattern. The diurnal range of between 36 and 39 °C has been reported previously in a large group of marmosets (Hetherington 1978). These studies indicated that there was no significant difference in the Tc between male and female animals. A deviation from this diurnal Tc pattern was the first indication of infection with F. tularensis, with the appearance of overt clinical signs, particularly piloerection, at 12–18 h later. Temperature increases followed by clinical signs have been reported previously in murine studies (Williamson et al. 2007). In the present study, a longer delay between temperature increase and the onset of clinical signs was observed. However, the findings are consistent with human tularaemia, where a sudden onset of fever is the most frequently reported symptom (Saslaw et al. 1961; Evan et al. 1985). In human cases, the Tc peaked at approximately 38–39 °C but decreased with treatment.
Clinical signs in marmosets became more apparent with time as the disease progressed and a reduction in activity was quantified using the Actiwatch®-Mini devices (Mann et al. 2005). In the two marmosets tested (step 3, third repeat), both exhibited a significant decrease in daytime activity postchallenge. Symptoms reported from human cases of tularaemia (Saslaw et al. 1961; Evan et al. 1985) included headache, chills, fatigue, body aches and nausea. However, such clinical symptoms and signs are difficult to observe in animal models. The general demeanour of the marmosets and, the timing of clinical signs suggested that the disease progression was similar in both human and marmoset disease.
In order to determine the reproducibility of the model, three pairs of animals were challenged with a target dose of 100 CFU (step 3). The actual doses received by these animals ranged from 40 to 300 CFU (Table 1), with no statistical correlation between the actual dose received and the time to death. Generally, a dose-related time to mortality can be observed with infections, although this is most apparent between low and high doses. In the current study, the fact that there is no correlation between dose and mortality between 40 and 300 CFU strengthens the reproducibility of the model. The implication is also that a critical number of bacteria are required to cause lethal infection, resulting in a similar course of infection.
The course of the infection in marmosets was similar to previously reported animal models of tularaemia in terms of mean times to death and mortality rates. Mice, vervet monkeys and macaques (Macaca irus) have each been reported to die of infection between 4 and 7 days postchallenge (Tulis et al. 1970; Baskerville et al. 1978; Conlan et al. 2003).
The number of bacteria recovered from organs generally varied from between two and five logs. However, a similar trend was observed for all animals. All animals, except the female in step 2, exhibited the highest number of bacteria in the spleen. The lowest numbers of bacteria were recovered from the kidneys of all animals and, generally, equivalent numbers of bacteria were recovered from the other organs and blood. Interestingly, the animals that varied greatest from this trend were the animals that received the lowest doses (step 2). This may reflect a variation in the pathology and progression of infection at low challenge doses. The magnitude of bacterial load presented in this study is similar to that of murine studies (Conlan et al. 2003). However, the greatest numbers of bacteria in the organs of mice, at the late stage of infection, were isolated in the liver followed by the spleen and then the lung.
The pathology of tularaemia infection in the marmoset is comparable with that seen in humans, murine and other NHP infections. Gross pathology features including the presence of hepatosplenomegaly, multifocal pyogranulomatous inflammation and infiltrating immune cells have been reported in human infection (Avery & Barnett 1966; Syrjala et al. 1986; Martin & Marty 2001; Lamps et al. 2004). The most commonly reported infiltrating cell type in human tularaemia is the neutrophil (Lamps et al. 2004) and evidence of degenerated neutrophils were observed in all marmoset organs. The degeneration of the neutrophils was associated with the presence of microabscesses particularly in the liver and spleen, which were common features in human and animal infection (Lamps et al. 2004). Neutrophils have been reported to have a critical role for host defence against F. tularensis strain LVS in mice by restricting bacterial growth (Sjostedt et al. 1994). The degeneration of the neutrophils in the marmoset may be the evidence for the ability of the pathogen to overwhelm the innate immune response and therefore cause fatal infection. However, the role of the neutrophil in the infection process needs to be further clarified.
Other pathological features reported in human cases of tularaemia infection were also observed in marmosets. These included thrombosis, megakaryocytes and lung oedema (Syrjala et al. 1986; Martin & Marty 2001). The presence of thrombi is likely to be a premortem feature because of the laminated histological appearance. Thrombi are common in several bacterial infections including Actinobacillus pleuropneumoniae and Yersinia pestis infection and are thought to be associated with endotoxic shock (Finegold et al. 1968; Cho & Chae 2003). In airborne infection of rhesus macaques with Y. pestis, as with our present studies, the thrombi were more commonly observed in animals that died of infection rather than animals that were humanely culled (Finegold et al. 1968). In the macaques, the associated intravascular coagulation was associated with the presence of haemorrhagic infarcts in the lungs of the majority of animals.
Granulomatous inflammation in the lungs, liver, spleen and lymph nodes has also been observed in experimental infection in rhesus macaques and vervet monkeys (Eigelsbach et al. 1962; Hall et al. 1973; Baskerville et al. 1978) with the time to lethal infection being dependent on the virulence of the experimental strain of F. tularensis. Indeed the pathological presentation of naturally occurring tularaemia in marmosets is similar despite infection from a less virulent subspecies F. tularensis holarctica (Splettstoesser et al. 2007).
Reports in the literature of pulmonary involvement in human tularaemia are contradictory (Martin & Marty 2001); however, it has been reported to occur in 70% of fatal infections (Stuart & Pullen 1945). The lack of pulmonary involvement may be accounted for due to the different routes of infection or by a difference in the virulence of the strain. In the data presented here, alveolar inflammation and necrosis in the lungs were significant features; however, the severity of the liver pathology seen in the marmoset suggested that liver failure could be a major contributory factor to the cause of death, as has been suggested in murine infection (Conlan et al. 2003).
In conclusion, the common marmoset appears to be an appropriate animal model to investigate inhalational tularaemia. The low infectious dose and disease progression (including fever and time to death) are comparable with human disease and other animal models of tularaemia. Disease progression was reproducible in the small numbers of animals challenged thus far. High bacterial loads were recoverable from vital organs and there was a significant bacteraemia in all animals.
Acknowledgments
This project has been funded with Federal funds from the National Institute of Allergy and Infectious Diseases (NIAID), under contract No. N01-AI-30062 through our Prime Contractor, the Health Protection Agency, Porton Down, UK. The authors would also like to thank the numerous people at Dstl that contributed technically to this work.
References
- Avery FW, Barnett TB. Pulmonary tularemia. Am. Rev. Respir. Dis. 1966;95:584–591. doi: 10.1164/arrd.1967.95.4.584. [DOI] [PubMed] [Google Scholar]
- Baskerville A, Hambleton P, Dowsett AB. The pathology of untreated and antibiotic-treated experimental tularaemia in monkeys. Br. J. Exp. Pathol. 1978;59:615–623. [PMC free article] [PubMed] [Google Scholar]
- CDC. CDC Emergency Preparedness and Response website, Bioterrorism Agents/Diseases, by Category. 2008. [accessed on 19 June 2008]. Available at: http://emergency.cdc.gov/agent/agentlist-category.asp.
- Chen W, Shen H, Webb A, KuoLee R, Conlan JW. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen: protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine. 2003;2125–26:3690–3700. doi: 10.1016/s0264-410x(03)00386-4. [DOI] [PubMed] [Google Scholar]
- Cho W-S, Chae C. Expression of cyclooxygenase-2 in swine naturally infected with Actinobacillus pleuropneumoniae. Vet. Pathol. 2003;40:25–31. doi: 10.1354/vp.40-1-25. [DOI] [PubMed] [Google Scholar]
- Conlan JW, Chen W, Shen H, Webb A, KuoLee R. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb. Pathog. 2003;34:239–248. doi: 10.1016/s0882-4010(03)00046-9. [DOI] [PubMed] [Google Scholar]
- Day WC, Berendt RF. Experimental tularemia in Macaca mulatta: relationship of aerosol particle size to the infectivity of airborne Pasteurella tularensis. Infect. Immun. 1972;5:77–82. doi: 10.1128/iai.5.1.77-82.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DT, Inglesby TV, Henderson DA, et al. Tularaemia as a biological weapon - medical and public health management. JAMA. 2001;285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- Dixon WJ, Fotheringham N. Application of staircase bioassays in pharmaceutical research. Drug Inf. J. 1993;27:741–751. [Google Scholar]
- Druett HA. A mobile form of the Henderson apparatus. J. Hyg. 1969;67:437–448. doi: 10.1017/s0022172400041851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eigelsbach HT, Tulis JJ, McGavran MH, White JD. Live tularaemia vaccine 1. J. Bacteriol. 1962;84:1020–1027. doi: 10.1128/jb.84.5.1020-1027.1962. Host-parasite relationship in monkeys vaccinated intra-cutaneously or aerogenically. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis J, Oyston PC, Green M, Titball RW. Tularaemia. Clin. Microbiol. Rev. 2002;15:631–646. doi: 10.1128/CMR.15.4.631-646.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evan ME, Gregory DW, Schaffner W, McGee ZA. Tularemia: a 30-year experience with 88 cases. Medicine (Baltimore) 1985;64:251–269. [PubMed] [Google Scholar]
- Finegold MJ, Petery JJ, Berendt RF, Adams HR. Studies on the pathogenesis of plague. Am. J. Pathol. 1968;53:99–114. Blood coagulation and tissue responses of Macaca mulatta following exposure to aerosols of Pasteurella pestis. [PMC free article] [PubMed] [Google Scholar]
- Hall WC, Kovatch RM, Schricker RL. Tularaemic pneumonia: pathogenesis of the aerosol-induced disease in monkeys. J. Pathol. 1973;110:193–201. doi: 10.1002/path.1711100302. [DOI] [PubMed] [Google Scholar]
- Hetherington CM. Circadian oscillations of body temperature in the marmoset, Callithrix jacchus. Lab. Anim. 1978;12:107–108. doi: 10.1258/002367778780953215. [DOI] [PubMed] [Google Scholar]
- Lamps LW, Havens JM, Sjostedt A, Page DL, Scott MA. Histologic and molecular diagnosis of tularemia: a potential bioterrorism agent endemic to North America. Mod. Pathol. 2004;17:489–495. doi: 10.1038/modpathol.3800087. [DOI] [PubMed] [Google Scholar]
- Lever MS, Stagg AJ, Nelson M, et al. Experimental respiratory anthrax infection in the common marmoset (Callithrix jacchus) Int. J. Exp. Pathol. 2008;89:171–179. doi: 10.1111/j.1365-2613.2008.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons RC, Wu TH. Animal models of Francisella tularensis infection. Ann. N. Y. Acad. Sci. 2007;1105:238–265. doi: 10.1196/annals.1409.003. [DOI] [PubMed] [Google Scholar]
- Mann TM, Williams KE, Pearce PC, Scott EAM. A novel method for activity monitoring in small non-human primates. Lab. Anim. 2005;39:169–177. doi: 10.1258/0023677053739783. [DOI] [PubMed] [Google Scholar]
- Martin GM, Marty AM. Clinicopathologic aspects of bacterial agents. Clin. Lab. Med. 2001;21:513–548. [PubMed] [Google Scholar]
- Posthaus H, Welle M, Morner T, Nicolet J, Kuhnert P. Tularemia in a common marmoset (Callithrix jacchus) diagnosed by 16S rRNA sequencing. Vet. Microbiol. 1998;61:145–150. doi: 10.1016/s0378-1135(98)00180-1. [DOI] [PubMed] [Google Scholar]
- Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Tularemia vaccine study. Arch. Intern. Med. 1961;107:702–714. doi: 10.1001/archinte.1961.03620050068007. II. Respiratory challenge. [DOI] [PubMed] [Google Scholar]
- Sawyer WD, Dangerfield HG, Hogge AL, Crozier D. Antibiotic prophylaxis and therapy of airborne tularemia. Bacteriol. Rev. 1966;30:542–550. doi: 10.1128/br.30.3.542-550.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schricker RL, Eigelsbach HT, Mitten JQ, Hall WC. Pathogenesis of tularemia in monkeys aerogenically exposed to Francisella tularensis 425. Infect. Immun. 1972;5:734–744. doi: 10.1128/iai.5.5.734-744.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjostedt A, Conlan JW, North RJ. Neutrophils are critical for host defense against primary infection with the facultative intracellular bacterium Francisella tularensis in mice and participate in defense against reinfection. Infect. Immun. 1994;62:2779–2783. doi: 10.1128/iai.62.7.2779-2783.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Splettstoesser WD, Mätz-Rensing K, Seibold E, et al. Re-emergence of Francisella tularensis in Germany: fatal tularaemia in a colony of semi-free-living marmosets (Callithrix jacchus) Epidemiol. Infect. 2007;135:1256–1265. doi: 10.1017/S0950268807008035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart BM, Pullen RL. Tularemic pneumonia. Am. J. Med. Sci. 1945;210:223. Review of American literature and report of 15 additional cases. [Google Scholar]
- Syrjala H, Sutinene S, Jokinen K, Nieminen P, Tuuponen T, Salminen A. Bronchial changes in airborne tularemia. J. Laryngol. Otol. 1986;100:1169–1176. doi: 10.1017/s0022215100100775. [DOI] [PubMed] [Google Scholar]
- Tulis JJ, Eigelsbach HT, Hornick RB. Oral vaccination against tularemia in the monkeys. Proc. Soc. Exp. Biol. Med. 1969;132:893–897. doi: 10.3181/00379727-132-34331. [DOI] [PubMed] [Google Scholar]
- Tulis JJ, Eigelsbach HT, Kerpsack RW. Host-parasite relationship in monkeys administered live tularemia vaccine. Am. J. Pathol. 1970;58:329–336. [PMC free article] [PubMed] [Google Scholar]
- Williamson ED, Savage VL, Lingard B, Russell P, Scott EAM. A biocompatible microdevice for core body temperature monitoring in the early diagnosis of infectious diseases. Biomed. Microdevices. 2007;9:51–60. doi: 10.1007/s10544-006-9007-5. [DOI] [PubMed] [Google Scholar]