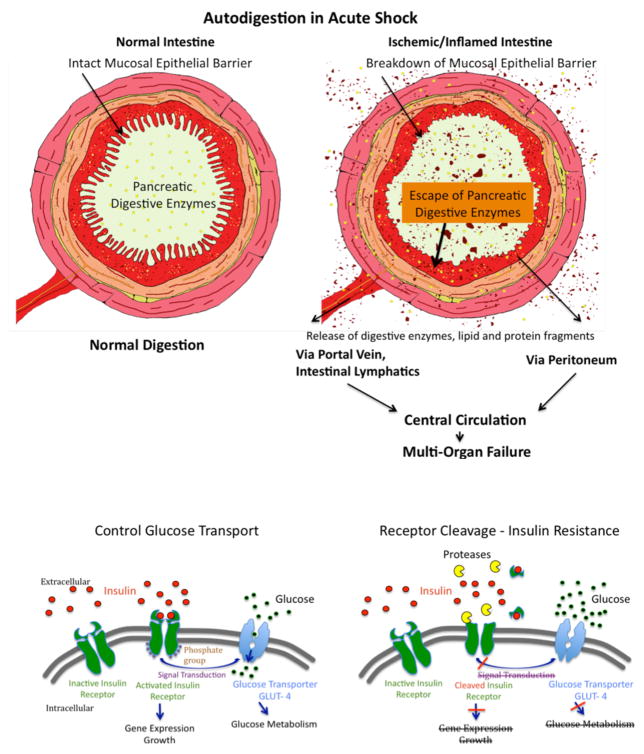
Figure 7.
(A) Schematic Diagram of Autodigestion by Pancreatic Enzymes in the Intestine. The fully activated pancreatic digestive enzymes are during normal digestion contained within the lumen of the intestine by the mucosal epithelial barrier (Left Panel). Compromise of the mucosal barrier, e.g. due to ischemia or infection of the mucosal barrier, permits entry of fully activated pancreatic enzymes into the wall of the intestine (Right Panel). This creates two complications, generation if proinflammatory and cytotoxic mediators, and morphological destruction of the mucosal barrier allowing further entry of digestive enzymes into the wall of the intestine. Pancreatic enzymes as well as inflammatory mediators are carried out of the intestinal wall via the intestinal venous system, the intestinal lymphatics and by leakage across the outer coat of intestine connective tissue (serosa) into the peritoneum and into the central circulation. Appearance of pancreatic enzymes and these inflammatory mediators leads to central inflammation and innocent bystander organ damage. i.e. multi-organ failure.
(B) Schematic Diagram of Protease Activity, Insulin Receptor Cleavage, and Insulin Resistance. The normal transmembane transport of glucose into the cell cytoplasm via the glucose transporter GLUT-4 as well as gene expression and growth factor synthesis requires intracellular signaling from the activated (phosphorylated) insulin receptor after binding of insulin to its extracellular domain (left panel). The appearance of uncontrolled degrading enzyme activity (e.g. due to MMPs, serine proteases) leads to cleavage of the extracellular domain of the insulin receptor (right panel), a lack of insulin binding sites on the insulin receptor, reduced intracellular signaling with attenuated glucose transport by GLUT-4, i.e. type II diabetes with insulin resistance due to reduced insulin receptor binding sites.