Abstract
Extramedullary plasmacytoma (EPM) is a plasma cell tumor arising outside of the bone marrow. Solitary EMP is an uncommon neoplasm and rarely occurs in the retroperitoneum and lacks distinctive clinical manifestations. We report a 26-year-old man with a solitary EMP in the retroperitoneum and discuss its clinical features, diagnosis and treatment.
Keywords: Extramedullary plasmacytoma, Retroperitoneal neoplasm, Computed tomography, Histopathology
INTRODUCTION
Extramedullary plasmacytoma (EMP), accounting for approximately 3% of all plasma cell neoplasms, results from uncontrolled plasma cell proliferation and consists of monoclonal plasmacytic infiltration without bone marrow involvement[1]. Approximately 80%-90% of EMPs involve mucosa-associated lymphoid tissue of the upper airway and 75% of them involve the nasal and paranasal regions, while retroperitoneal infiltration is very rare[2]. We report a 26-year-old man with a solitary EMP in the retroperitoneum.
CASE REPORT
A 26-year-old man was referred to our hospital with a history of abdominal distention and effort intolerance persisting for the previous 2 mo. He had no history of fever, weight loss, bladder or bowel dysfunction, and back pain. Physical examination revealed an irregular, firm, non-tender mass occupying almost the whole abdomen. He had no icterus or lymphadenopathy with normal tests. An abdominal computed tomography (CT) scanning showed a large heterogeneous mass in the right retroperitoneal region, surrounding the posterior portion of the right kidney and compressing the right kidney (Figure 1A). The tumor tissue was slightly enhanced after injection of a contrast medium (Figure 1B).
Figure 1.
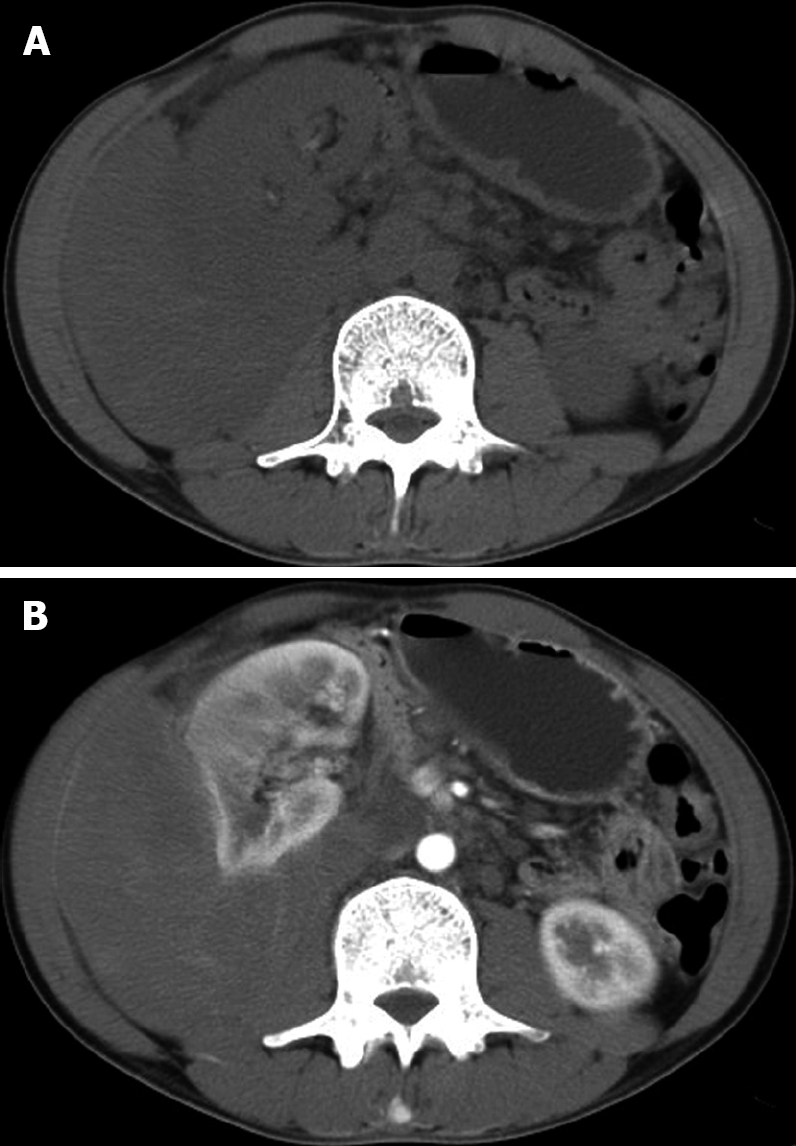
Abdominal computed tomography showing a large heterogeneous mass in the right retroperitoneal region, surrounding the posterior portion of the right kidney and compressing the right kidney (A), and slightly enhanced tumor tissue after injection of a contrast medium (B).
Laboratory test revealed 2.8 × 109/L white blood cells (WBC) (normal range 4-10 × 109/L), 119 g/L hemoglobin (Hb) (normal range 120-160 g/L), 122 × 109/L platelets (PLT) (normal range 100-300 × 109/L), and normal serum levels of creatinine, blood urea nitrogen, amylase, hepatic enzymes, electrolytes including calcium and phosphorus. No erythrocyte or protein was observed in his urine.
Fine needle aspiration cytology of the mass was not done because of refusal of his parents who were afraid of needle track implantation. Thereafter, an extensive resection of the tumor including extirpation of the right kidney, and part of the liver was performed. Postoperative recovery was uneventful.
Histopathology revealed a 30 cm × 16 cm × 10 cm tumor surrounding the posterior portion of the right kidney with adherent liver. Microscopy showed diffusive infiltration of polygonal cells in the retroperitoneum. Homogeneous amphophilic cytoplasm, wheel-type and asymmetric nuclei, coarsely stippled chromatin, and some acidophilic nucleoli were observed in the tumor cells. Binucleate cells were also occasionally observed (Figure 2A). Immunohistochemistry demonstrated tumor cells were positive for CD138 (Figure 2B), Bcl-2 and VS38C, but negative for CD20, CD3, CD79a, CK, CD38, S-100, CD5, CK, myosin and CD10.
Figure 2.
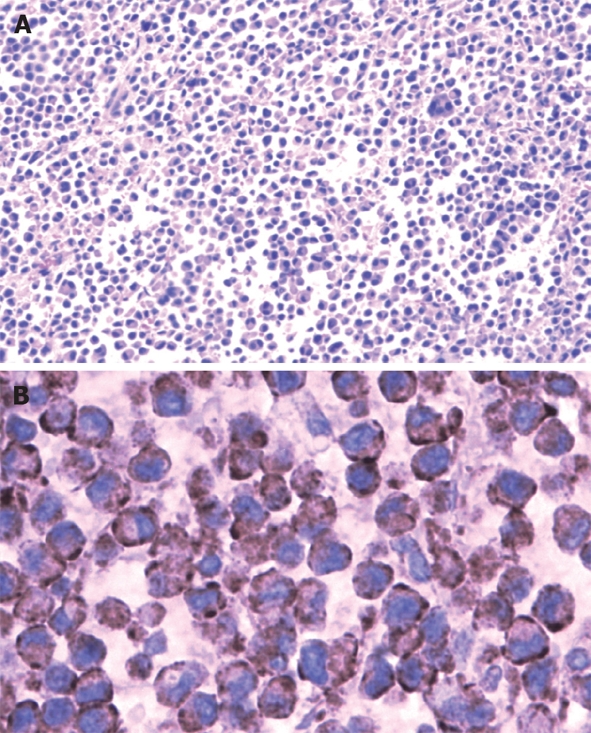
Tumor cells with homogenous amphophilic cytoplasm, whell-type and asymmetric nuclei, coarsely stippled chromatin, some acidophilic nucleoli, and occasional binucleate (A) (HE, × 100) and positive tumor cells for CD138 (B) (× 400) under microscope.
To confirm the diagnosis of EMP, further investigations were done after surgery. Serum IgG was 25.4 g/L (normal range 6.94-16.20 g/L). Serum IgA and IgM levels were within normal range. No Bence-Jones protein was detected in his urine. Iliac crest bone marrow aspiration and biopsy did not find any plasmacytic infiltration. A skeletal survey revealed no osteolytic lesions.
DISCUSSION
Solitary bone and extramedullary plasmacytomas are rare plasma cell proliferative disorders. Their diagnosis is based on the monoclonal plasma cell infiltration at a single disease site and the exclusion of systemic myeloma[3]. WBC and hemoglobin were slightly abnormal, and iliac crest bone marrow aspiration and biopsy showed no plasmacytic infiltration in our case. We ascribed these abnormalities to the fact that he worked as a painter for 8 years prior to surgery. Hematopathy can be found in workers exposed to benzene[4].
EMP occurs most commonly in the head and neck region, followed by gastrointestinal (GI) tract, central nervous system (CNS), thyroid, breast, parotid gland, testis, and lymph nodes[5].
Solitary EMP rarely occurs in the retroperitoneum. Cases of retroperitoneal EMP have different clinical manifestations, such as renal failure due to bilateral renal vein occlusion[6], flank pain, hematuria due to thrombosis of the renal vein[7], obstructive jaundice[8], abdominal distention and pain[9,10], and hyperamylasemia[11]. However, our patient presented with only abdominal distention and effort intolerance.
Retroperitoneal EMP should be differentially diagnosed from lymphoplasmacytic lymphoma and immunoblastic lymphoma[12]. Immunohistochemistry is used for its final diagnosis. In our case, microscopy showed that the tumor cells might be origined from plasmacytic cells confirmed by immunohistochemistry.
Preoperative CT scanning does not contribute to its differential diagnosis from other tumors, while preoperative angiography can indicate the vessels feeding the mass and the correlation to other vessels. Serum electrophoresis can help its diagnosis by finding the M band. However, we considered the mass as a common type of tumors, such as schwannoma, sarcoma before operation and serum electrophoresis was not done.
No clear guidelines for treatment of EMP are available due to its rarity and variable presentations. EMP is highly radiosensitive with excellent results (< 10% of local recurrences and about 50%-65% of patients remain free of disease for > 10 years)[13]. However, it is associated with a high morbidity particularly when used for large retroperitoneal tumors. It was reported that there is no evidence that retroperitoneal EMP progresses one year after chemotherapy in combination with radiotherapy[14]. Chen et al[8] have reported a case of retroperitoneal EMP accompanying obstructive jaundice, who showed a complete response to sequential radiotherapy and chemotherapy.
Sharma et al[10] performed a complete surgical resection of a large bulky retroperitoneal EMP when the patient did not respond to chemotherapy, and found that the patient was symptom free 16 mo post surgery. Our patient did not receive chemotherapy or radiotherapy prior to operation. He was under observation 2 mo after surgery and remained asymptomatic when we wrote this paper.
In summary, EMP should be considered whenever a retroperitoneal soft tissue mass is identified.
Peer reviewer: Ibrahim A Al Mofleh, Professor, Department of Medicine, College of Medicine, King Saud University, PO Box 2925, Riyadh 11461, Saudi Arabia
S- Editor Li LF L- Editor Wang XL E- Editor Yin DH
References
- 1.Dimopoulos MA, Kiamouris C, Moulopoulos LA. Solitary plasmacytoma of bone and extramedullary plasmacytoma. Hematol Oncol Clin North Am. 1999;13:1249–1257. doi: 10.1016/s0889-8588(05)70124-6. [DOI] [PubMed] [Google Scholar]
- 2.Ooi GC, Chim JC, Au WY, Khong PL. Radiologic manifestations of primary solitary extramedullary and multiple solitary plasmacytomas. AJR Am J Roentgenol. 2006;186:821–827. doi: 10.2214/AJR.04.1787. [DOI] [PubMed] [Google Scholar]
- 3.Dimopoulos MA, Hamilos G. Solitary bone plasmacytoma and extramedullary plasmacytoma. Curr Treat Options Oncol. 2002;3:255–259. doi: 10.1007/s11864-002-0015-2. [DOI] [PubMed] [Google Scholar]
- 4.Wocka-Marek T, Zajac-Nedza M, Braszczyńska Z, Zygan U, Wójcik-Chrobok B, Lukas A, Klementys A. [Hematologic disorders in workers exposed to benzene and ethylbenzene] Przegl Lek. 1988;45:836–839. [PubMed] [Google Scholar]
- 5.Weber DM. Solitary bone and extramedullary plasmacytoma. Hematology Am Soc Hematol Educ Program. 2005;45:373–376. doi: 10.1182/asheducation-2005.1.373. [DOI] [PubMed] [Google Scholar]
- 6.Marks ES, Lee KM. Acute renal failure secondary to vascular occlusion by a retroperitoneal plasmacytoma. Cancer. 1984;53:1228–1229. doi: 10.1002/1097-0142(19840301)53:5<1228::aid-cncr2820530534>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi H, Itoh T, Murata R, Tanabe M. Primary retroperitoneal plasmacytoma with tumor thrombus within the renal vein. J Urol. 1992;147:452–454. doi: 10.1016/s0022-5347(17)37268-3. [DOI] [PubMed] [Google Scholar]
- 8.Chen TC, Wu JH, Ng KF, Lien JM, Hung CF. Solitary extramedullary plasmacytoma in the retroperitoneum. Am J Hematol. 1998;58:235–238. doi: 10.1002/(sici)1096-8652(199807)58:3<235::aid-ajh13>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 9.Sered S, Nikolaidis P. CT findings of perirenal plasmacytoma. AJR Am J Roentgenol. 2003;181:888. doi: 10.2214/ajr.181.3.1810888. [DOI] [PubMed] [Google Scholar]
- 10.Sharma LM, Biswas G, Rai SS, Nair R, Gupta S, Parikh PM. Retro-peritoneal plasmacytoma: a case report and review of literature. Indian J Cancer. 2004;41:133–134. [PubMed] [Google Scholar]
- 11.Tsai YS, Cheng HL, Lin JS, Tong YC, Chang KC. Retroperitoneal plasmacytoma associated with hyperamylasemia. J Urol. 1999;162:1681–1682. [PubMed] [Google Scholar]
- 12.El-Sharkawy MS, Siddiqui N, Aleem A, Diab AA. Renal involvement in lymphoma: prevalence and various patterns of involvement on abdominal CT. Int Urol Nephrol. 2007;39:929–933. doi: 10.1007/s11255-007-9224-8. [DOI] [PubMed] [Google Scholar]
- 13.Chao MW, Gibbs P, Wirth A, Quong G, Guiney MJ, Liew KH. Radiotherapy in the management of solitary extramedullary plasmacytoma. Intern Med J. 2005;35:211–215. doi: 10.1111/j.1445-5994.2005.00804.x. [DOI] [PubMed] [Google Scholar]
- 14.Saito M, Tsuchiya N, Iinuma M, Mitsumori K, Matsuura S, Shimoda N, Ohyama C, Satoh S, Sato K. [A case of retroperitoneal extramedullary plasmacytoma] Hinyokika Kiyo. 2003;49:735–739. [PubMed] [Google Scholar]


