Abstract
A 58-year-old woman presented with an acute embolic occlusion of the distal basilar artery. She underwent angioplasty and intra-arterial thrombolysis. Angiography performed after recanalization revealed a single perforating thalamic artery. A nonenhanced CT scan carried out immediately after the procedure revealed hyperdense lesions in the bilateral paramedian portions of the thalami, which disappeared on the 24-hour follow-up CT scan. Three months later, the patient improved to functional independence, but had some memory dysfunction and vertical gaze palsy. This case suggests that contrast enhancement or extravasation can occur in the thalamus after intra-arterial thrombolysis performed to recanalize a basilar artery occlusion.
Keywords: Contrast media, Thalamus, Thrombolysis
Anonenhanced CT scan obtained immediately after intra-arterial thrombolysis for an acute ischemic stroke can on rare occasions show hyperdense lesions, which behave differently from the hemorrhage. Recently, it was reported that such lesions could be categorized as an enhancement and an extravasation of the contrast medium given during the angiographic procedures (1). Both contrast enhancement and contrast extravasation have been observed in the region of the basal ganglia after intra-arterial thrombolysis to recanalize a middle cerebral artery occlusion (1-4). This report describes a case of contrast enhancement, which occurred in the bilateral paramedian regions of the thalami on CT after intra-arterial thrombolysis for the recanalization of an acute embolic occlusion of the basilar artery, and considers the pathogenesis of bilateral paramedian thalamic enhancement.
CASE REPORT
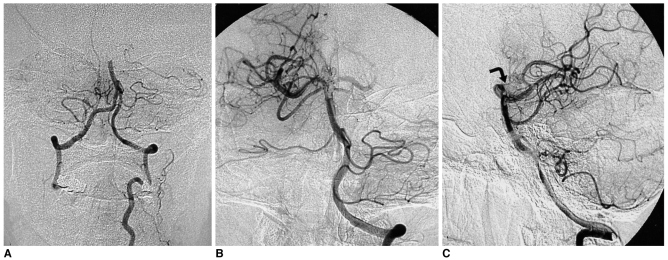
A 58-year-old woman presented to the emergency department with a stuporous mental state, ophthalmoplegia, and severe dysarthria. She had a prior history of cardiac valve replacement surgery for both mitral and aortic regurgitations 10 years earlier. Her National Institutes of Health Stroke Scale (NIHSS) score was 14 and modified Rankin Scale (mRS) score was 5. A CT scan of the head five hours after the onset of symptoms showed a hyperdense basilar artery on two consecutive 5-mm cut images, indicating an acute basilar artery embolism. After obtaining written informed consent for the endovascular therapy from the patient's family, the angiographic procedure began 5.5 hours after the onset of stroke. Angiography revealed a complete occlusion of the distal basilar artery (Fig. 1A). At this point, a loading dose of abciximab (0.25 mg/kg) was administered intravenously. Rapid recanalization was achieved using a minimum dose of thrombolytic agents by performing direct angioplasty first followed by intra-arterial thrombolysis. Angioplasty was performed using a 2.5 mm diameter coronary balloon catheter. The balloon catheter was advanced into the occlusion site and inflated to 4 atm for 30 seconds. Immediately after the angioplasty, the basilar artery was partially recanalized with a restoration of the blood flow to the both superior cerebellar arteries. A microcatheter was then placed just proximal to the occlusion site, and 400,000 units of urokinase were infused at a constant rate for one hour. The completion angiograms demonstrated a partial recanalization of the basilar artery with embolus remaining in the basilar tip and the restoration of blood flow to both the posterior and superior cerebellar arteries. In addition, angiograms demonstrated a single perforating thalamic artery that was divided into two branches (Figs. 1B, C). After the endovascular procedure, the patient showed progressive clinical improvement and regained complete consciousness within a few hours.
Fig. 1.
Left vertebral arteriogram (A) shows a complete occlusion of the distal basilar artery. Anteroposterior (B) and lateral (C) views of the angiogram obtained after the angioplasty and intra-arterial thrombolysis procedures demonstrates partial recanalization of the basilar artery and a single perforating thalamic artery (curved arrow) arising from the midline of the basilar bifurcation.
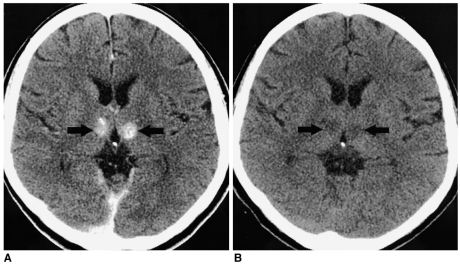
A non-enhanced CT scan obtained immediately after the endovascular therapy showed bilateral symmetrical high attenuations in the paramedian thalamic regions (Fig. 2A). The maximum Hounsfield unit of hyperdense lesions was 67. On the following day, her NIHSS score was 6 and the patient developed hypersomnolence, severe memory impairments, and vertical gaze palsy. The follow-up nonenhanced CT scan obtained 24 hours after completing the intra-arterial thrombolytic therapy showed the disappearance of the hyperdense lesions and the development of hypodensities in the bilateral paramedian thalamic regions without a hemorrhagic transformation (Fig. 2B). The patient's clinical conditions improved continuously. After three months, the patient improved to functional independence (NIHSS score from 14 to 4; mRS score from 5 to 1) but continued to have both short and long-term memory dysfunction as well as vertical gaze palsy.
Fig. 2.
A. Nonenhanced CT scan performed immediately after the intraarterial thrombolytic therapy shows hyperdense lesions (arrows) in the bilateral paramedian regions of the thalami.
B. The follow-up CT scan obtained 24 hours after completing the intra-arterial thrombolytic procedure shows the disappearance of the hyperdense lesions and the development of hypodensities (arrows) in the bilateral paramedian thalamic regions.
DISCUSSION
A hyperdense lesion observed on the post-therapeutic, nonenhanced CT scans obtained immediately after intraarterial thrombolysis has been described as either a hemorrhage or an extravasation of the contrast medium given during the angiographic procedures performed during the thrombolysis procedures (2-4). Yoon et al. (1) reported that a hyperdense lesion that has different characteristics from a hemorrhage in terms of both the CT findings and the clinical outcome could be categorized as two entities: contrast enhancement and contrast extravasation. In their study, contrast enhancement was defined as a hyperdense lesion that disappeared on the 24-hour follow-up CT scan, without leaving a hematoma cavity or a mass effect, and contrast extravasation as a hyperdense lesion with a maximum HU > 90, which persisted on the 24-hour follow-up CT scan. They also concluded that both the contrast enhancement and contrast extravasation develop primarily in the region of the basal ganglia in accordance with the specific vascular territory (1).
The CT findings in the present case are consistent with contrast enhancement, which occurred in the thalamus after an intra-arterial thrombolysis procedure, according to the definition by Yoon et al. (1). It has been reported that contrast enhancement and contrast extravasation occur primarily in the basal ganglia after intra-arterial thrombolysis in those patients with an occlusion of the middle cerebral artery (1-4). To the best of our knowledge, there are no reports regarding thalamic enhancement after thrombolysis in patients with an acute occlusion of the basilar artery. Perforating thalamic arteries are the terminal vessels with poor collaterals. The prolonged infusion of thrombolytic agents and contrast materials in the vicinity of the perforating thalamic branches may have resulted in the leakage of the contrast medium through the injured blood brain barrier (BBB) of the perforating microvessels supplying the thalamus. This can lead to the gradual accumulation of contrast medium, which manifests as contrast enhancement on the nonenhanced CT scans obtained immediately after the thrombolytic procedure.
In this case, the contrast enhancement occurred in the symmetrical bilateral paramedian regions of both thalami. The suggested mechanism for this finding is a disruption of the BBB of a single perforating thalamic artery (paramedian artery), which supplies the paramedian part of the upper midbrain and thalamus, including the intralaminar nuclear group and most of the dorsomedial nucleus (5). In this case, angiography clearly demonstrated a single paramedian artery. It was reported that a single perforating thalamic artery can supply the paramedian territory on both sides, and an occlusion of this artery can result in corresponding bilateral infarctions in the paramedian aspects of the thalami (6). A cadaver dissection study reported that the origin of the perforating thalamic arteries was unilateral in eight of 12 brains (7).
In conclusion, contrast enhancement can occur in the thalamus after an intra-arterial thrombolysis procedure in patients with an acute basilar artery occlusion. In addition, a pathological process involving a single perforating thalamic artery can result in symmetrical bilateral disease in the paramedian regions of both thalami.
References
- 1.Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004;35:876–881. doi: 10.1161/01.STR.0000120726.69501.74. [DOI] [PubMed] [Google Scholar]
- 2.Nakano S, Iseda T, Kawano H, Yoneyama T, Ikeda T, Wakisaka S. Paranchymal hyperdensity on computed tomography after intra-arterial reperfusion therapy for acute middle cerebral artery occlusion: incidence and clinical significance. Stroke. 2001;32:2042–2048. doi: 10.1161/hs0901.095602. [DOI] [PubMed] [Google Scholar]
- 3.Yokogami K, Nakano S, Ohta H, Goya T, Wakisaka S. Prediction of hemorrhagic complications after thrombolytic therapy for middle cerebral artery occlusion: value of pre-and post-therapeutic computed tomographic findings and angiographic occlusive site. Neurosurgery. 1996;39:1102–1107. doi: 10.1097/00006123-199612000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Mericle RA, Lopes DK, Fronckowiak MD, Wakhloo AK, Guterman LR, Hopkins LN. A grading scale to predict outcomes after intra-arterial thrombolysis for stroke complicated by contrast extravasation. Neurosurgery. 2000;46:1307–1315. doi: 10.1097/00006123-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Bogousslavsky J, Regli F, Uske A. Thalamic infarcts: clinical syndromes, etiology, and prognosis. Neurology. 1988;38:837–848. doi: 10.1212/wnl.38.6.837. [DOI] [PubMed] [Google Scholar]
- 6.Roitberg BZ, Tuccar E, Alp MS. Bilateral paramedian thalamic infarct in the presence of an unpaired thalamic perforating artery. Acta Neurochir. 2002;144:301–304. doi: 10.1007/s007010200040. [DOI] [PubMed] [Google Scholar]
- 7.Cosson A, Tatu L, Vuillier F, Parratte B, Diop M, Monnier G. Arterial vascularization of the human thalamus: extra-parenchymal arterial groups. Surg Radiol Anat. 2003;25:408–415. doi: 10.1007/s00276-003-0153-7. [DOI] [PubMed] [Google Scholar]