Abstract
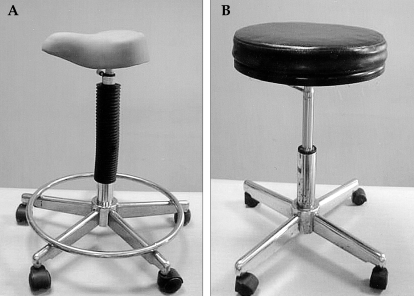
Non-surgical vaginal dilation is a safe and effective method for the creation of neovagina in the patient with vaginal agenesis. Compared to surgical methods, non-surgical vaginal dilation has the advantage of low morbidity, the creation of a more physiologic vaginal milieu, and no surgical scarring. To overcome some technical limitations of original Frank's method, in 1981 Ingram proposed a modification of the technique that used dilators of gradually increasing size mounted on a bicycle seat stool. Although several studies have shown satisfactory outcomes using Ingram's method, there are some practical difficulties in making and handling the bicycle seat stool. This article reports a case of a 24-year-old woman with Mayer-Rokitansky-Küster-Hauser syndrome whose vaginal agenesis is successfully treated with a simplified version of Ingram's method. This method uses dilators of gradually increasing size mounted on an ordinary chair instead of a bicycle seat stool. When necessary, the patient may use a fulcrum under the dilator.
Keywords: Vaginal agenesis, vaginal dilation, Mayer-Rokitansky-Küster-Hauser syndrome, simplified Ingram's method
INTRODUCTION
Müllerian agenesis is the second most common cause of primary amenorrhea. It affects 1/5,000 to 1/10,000 live-born females.1 Since R.T. Frank's earlier description,2 the effectiveness of non-surgical methods for the creation of a neovagina has been assessed in many patients with vaginal agenesis. Based on satisfactory clinical outcomes and low morbidity, several authors have suggested that non-surgical vaginal dilation should be considered the first-line therapy in patients with vaginal agenesis.3,4 As recently reported, in a group of patients with müllerian agenesis, 87-91% of them were able to fashion a functional vagina using vaginal dilation.3,5
Frank's initial technique used hand-held vaginal dilators in the lithotomy position and had technical limitations such as fatigue of patient's hands, loss of time spent during the process of dilation, and uncomfortable positioning. Ingram's method overcomes these difficulties by using the sitting position to take advantage of the patient's body weight.6 This method uses vaginal dilators mounted on a specially designed bicycle seat stool that provides perineal pressure via the narrow and elevated anterior portion of the bicycle seat. Despite the favorable clinical outcome of this method,3 there are some practical difficulties in making and handling the bicycle seat in a busy outpatient clinic. This article reports a case in which vaginal agenesis was successfully treated using a simplified version of Ingram's method. In this modification, vaginal dilators were mounted on an ordinary chair instead of on a bicycle seat stool.
CASE REPORT
A 24-year-old woman came to the adolescent clinic for treatment of vaginal agenesis. At the same clinic, she had been diagnosed with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome 5 years prior. On initial examination, she presented with primary amenorrhea but normal secondary sex characteristics.
She had been in good health with no significant medical history. Her general physical examination was normal. She had no features of associated skeletal abnormalities. Her breasts and pubic hair were Tanner stage 4. External genital examination revealed fully estrogenized external genitalia and a vaginal dimple, 0.5 cm in depth. The uterus and cervix were not palpable on the recto-abdominal examination.
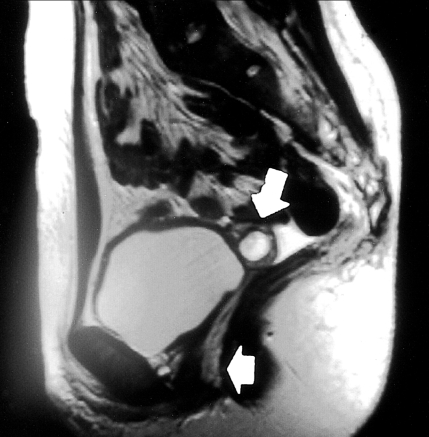
Laboratory study revealed a serum FSH level of 6.78 mIU/mL and an LH level of 9.44 mIU/mL. Thyroid function tests and serum prolactin level were within normal limits. The serum testosterone level was 0.19 ng/mL (0.08-0.86 ng/mL) and karyotype was 46, XX. Pelvic MRI confirmed a diagnosis of müllerian agenesis. The MRI showed complete agenesis of the vagina and small rudimentary uterus. The ovaries were normal bilaterally (Fig. 1). IVP showed a normal urinary tract system.
Fig. 1.
Pelvic MR image shows complete agenesis of the vagina (short arrow) and suggests the presence of a rudimentary uterus (2-cm diameter) (long arrow).
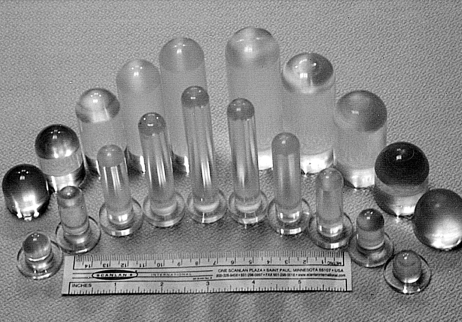
As with Ingram's method, the patient was told to carry out vaginal dilation using acrylic dilators of gradually increasing size (Fig. 2).6 The patient was given careful instructions about the correct use of the dilators. She was instructed to place the tip of the dilator at the vaginal dimple between the anus and the urethra. Unlike Ingram's original method, she was told to sit on the ordinary chair (Fig. 3), instead of a bicycle seat. She was told to lean forward and set her legs apart thus allowing her perineum to be in close contact with the chair. She was instructed to do this at least for an hour a day. Occasionally, if she felt that the dilators fit poorly in spite of these postures, she could put a small fulcrum under the dilators. No specific recommendations were given to the patient in the selection of the chair except to choose a chair with a hard surface.
Fig. 2.
The acrylic dilators. Among the three sets of dilators,6 the first two sets (diameters of 1.5 cm and 2.5 cm) were used in this patient.
Fig. 3.
A bicycle seat stool (A) and an ordinary chair (B). The photo of the ordinary chair is shown as an example, but was not the chair used in our study.
The starting dilator was 3 cm in length 1.5 cm in diameter. After the patient was given instructions and successfully began dilation, she was followed up every 2 weeks for measuring vaginal length and changing the mold number when adequate. She was instructed to use the dilators by increasing the length and width alternatively until a satisfactory vaginal orifice was created. Among the three sets of Ingram's dilators, only the 1.5 cm and 2.5 cm diameter sets were used. She did not want to introduce dilators of the largest diameter (3.0 cm). After 8 weeks of treatment, her vagina increased to 7 cm in length and 2.5 cm in diameter. At this time, she got married and had sexual intercourse without difficulties. After 4 months of treatment, her vagina had increased to 8 cm length and to more than 2.5 cm in diameter. The treatment took place without significant complications. There was no dilation of the urethral meatus nor was there vaginal prolapse. If she could not engage in coitus for long periods of time, the patient was advised to perform dilation several times a week to maintain a functional vagina.
DISCUSSION
Müllerian agenesis, also referred to as MRKH syndrome or müllerian aplasia, is caused by the embryologic failure of the müllerian duct development. This causes a congenital absence of the uterus and vagina. Though a rudimentary uterus can be found in the pelvic cavity it may not function properly.
There are several surgical and non-surgical options for the treatment of vaginal agenesis. After the observation that coitus alone could create a functional vagina in some patients with vaginal agenesis, several attempts for non-surgical vaginal dilation were examined. In 1938, Frank described the use of Pyrex® tubes of gradually increasing sizes (0.8 cm, 1.5 cm and 2.0 cm in diameter). This was used to force the mucous membrane inward into the introital region. No incision was required in this procedure.2 Decades after Frank's first description, several studies reported favorable outcomes using his method.5,7,8 In 2000, Robson and Oliver reported a success rate of 64% in 25 women with MRKH syndrome using Frank's method.7 They noticed that non-surgical dilation was very successful in women motivated by a sexual relationship. In another clinical trial, Costa et al. reported that 87% of patients with ambiguous genitalia who used Frank's vaginal dilation method had satisfactory sexual intercourse. This trial used acrylic molds (1.5 cm, 2.5 cm and 3.0 cm in diameter) with a metallic hook on one end.5
Earlier studies of Frank's method were not as promising. Rock et al., in 1983, reported a 43% success rate with Frank's method in 21 patients with müllerian agenesis.9 They suggested that the failure was associated with a prior vaginal exploration. In 1981, Ingram asserted that the reasons for failure of Frank's vaginal dilation were sheer fatigue of the hands and fingers, the necessity for the use of the awkward position, and the inability to perform other productive activities during the procedure.6 In an attempt to overcome these limitations, Ingram proposed a modification of original Frank's method. In Ingram's method, the weight of the patient is used to substitute manual and digital exertion. The specially designed "male" type bicycle seat stool was used to facilitate perineal mold pressure. Corroborating the results of Ingram's successful trial, Roberts et al. reported a 91% success rate using Ingram's method in their study of 51 patients with MRKH syndrome.3
Despite the noteworthy outcomes using Ingram's method, there were no sufficient efforts to verify the necessity of a bicycle seat.3,6 Ingram noticed the use of this special instrument and suggested that it can be constructed easily, quickly and inexpensively. However, the examiners felt there were some practical difficulties in manufacturing and handling the bicycle seat stool.
In this study, the patient was given instructions to modulate perineal pressure with postural changes instead of using a bicycle seat. In order for her perineum to firmly contact the chair, the patient was asked to lean forward with her legs apart. If the patient felt that there was a lack of adequate pressure in spite of these postures, she was allowed to use a fulcrum under the dilator. This was the case in the later stages of using each dilator. With these simple modifications, the vaginal length had successfully increased to 8 cm within 4 months and the patient experienced satisfactory sexual intercourse. The time required to achieve a functional vagina in this patient was not greater than that of Ingram's original patients.6
A trial using an ordinary chair instead of the bicycle seat stool in Ingram's method has not been previously described in the literature. An ordinary chair is more easily accessible at home and may offer more comfort during the procedure. Following the outcome of this case, an ordinary chair can be considered as a viable alternative to the bicycle seat if the patient is motivated and carefully instructed. Furthermore, it can be used when a bicycle seat is unavailable. However, a clinical study examining a larger number of patients may be necessary to verify the effectiveness and limitations of this modification.
References
- 1.Evans TN, Poland ML, Boving RL. Vaginal malformations. Am J Obstet Gynecol. 1981;141:910–920. doi: 10.1016/s0002-9378(16)32683-7. [DOI] [PubMed] [Google Scholar]
- 2.Frank RT. The formation of an artificial vagina without operation. Am J Obstet Gynecol. 1938;35:1053–1055. [Google Scholar]
- 3.Roberts CP, Haber MJ, Rock JA. Vaginal creation for müllerian agenesis. Am J Obstet Gynecol. 2001;185:1349–1352. doi: 10.1067/mob.2001.119075. [DOI] [PubMed] [Google Scholar]
- 4.Edmonds DK. Vaginal and uterine anomalies in the paediatric and adolescent patient. Curr Opin Obstet Gynecol. 2001;13:463–467. doi: 10.1097/00001703-200110000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Costa EM, Mendonca BB, Inacio M, Arnhold IJ, Silva FA, Lodovici O. Management of ambiguous genitalia in pseudohermaphrodites: new perspectives on vaginal dilation. Fertil Steril. 1997;67:229–232. doi: 10.1016/s0015-0282(97)81902-4. [DOI] [PubMed] [Google Scholar]
- 6.Ingram JM. The bicycle seat stool in the treatment of vaginal agenesis and stenosis: a preliminary report. Am J Obstet Gynecol. 1981;140:867–873. doi: 10.1016/0002-9378(81)90076-4. [DOI] [PubMed] [Google Scholar]
- 7.Robson S, Oliver GD. Management of vaginal agenesis: review of 10 years practice at a tertiary referral centre. Aust NZ J Obstet Gynaecol. 2000;40:430–433. doi: 10.1111/j.1479-828x.2000.tb01175.x. [DOI] [PubMed] [Google Scholar]
- 8.Lappöhn RE. Congenital absence of the vagina - results of conservative treatment. Eur J Obstet Gynecol Reprod Biol. 1995;59:183–186. doi: 10.1016/0028-2243(94)02037-f. [DOI] [PubMed] [Google Scholar]
- 9.Rock JA, Reeves LA, Retto H, Baramki TA, Zacur HA, Jones HW., Jr Success following vaginal creation for Müllerian agenesis. Fertil Steril. 1983;39:809–813. [PubMed] [Google Scholar]