Abstract
Introduction
A comprehensive approach to the prevention of overweight and obesity requires identifying the socioeconomic and cultural factors involved. This study set out to determine the prevalence of overweight and obesity among children starting school in Augsburg, Germany. Another aim was to examine influencing factors and any associations between the findings and the children’s first language.
Methods
In the context of the school entry health examination for the 2006/2007 school year, the parents of 2306 children were surveyed by means of an anonymous questionnaire. The investigators documented each child’s sex, age, body weight, height, and first language, as well as the preschool attended. The data were evaluated descriptively using SPSS 14.0.
Results
Overall, 13.1% (n = 302) of the children were overweight, including 4.9% (n = 113) who were obese. The prevalence of overweight and obesity was nearly twice as high among children whose first language was not German. Half of all children did not attend a sports or dance group. More than half of the overweight children watched television for one to three hours each day.
Discussion
The prevalence of overweight and obesity differs depending on ethnic origin. Children from immigrant families are a high-risk group. Targeted prevention strategies are necessary for children of elementary school age. Our data may serve as the basis for developing neighborhood or district-wide interventions.
Keywords: children starting school, overweight, prevention, children’s health, physical activity
In their review, Koletzko and colleagues describe the important role played by poor eating habits and sedentary lifestyle in the development of childhood overweight and obesity (1). Overweight children and adolescents often become overweight adults, with an increased risk for secondary diseases, such as type 2 diabetes, orthopedic problems, and cardiovascular disease.
A recent Danish study examining the effects of increased body mass index (BMI) during childhood on the risk of coronary heart disease (CHD) in adulthood found a positive linear relationship between the two factors (2). Earlier, the Bogalusa Heart Study examined the association between overweight and cardiovascular risk factors among children and adolescents (3). The results showed associations of varying magnitude between overweight and insulin levels, total cholesterol, triglycerides, low-density lipoprotein (LDL), and systolic and diastolic blood pressure. In addition, a clustering of risk factors was observed in overweight children and adolescents.
The first results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS, Kinder- und Jugendgesundheitssurvey) have been published elsewhere by the Robert Koch Institute; these demonstrate that overweight and obesity are the most common health risks among children and adolescents today (4).
Overweight and obesity are multifactorial in origin; in addition to socioeconomic factors (5), physical activity and nutritional habits play an important role in prevention. In order to follow data available from observational studies, guidelines for health-enhancing physical activity should recommend the accumulation of activity rather than focusing on specific, fitness-oriented exercise sessions. Spontaneous, but more frequent bouts of activity are more effective in children than the training regimens typically used for adults; indeed, it appears that the former correspond more closely to children’s natural patterns of movement (6).
A comprehensive approach to the prevention of overweight and obesity requires indentifying not only individual causes, but also the social, economic, and cultural factors that contribute to the increasing prevalence of these disorders.
Data from the Kiel Obesity Prevention Study (KOPS) show that overweight children differed from normal-weight children more in terms of their physical activity patterns than with regard to their dietary habits. For the most part, differences in body weight were attributable to differences in physical activity and television time, as well as to social factors (educational level of parents) and possible genetic risk (parental body weight) (7).
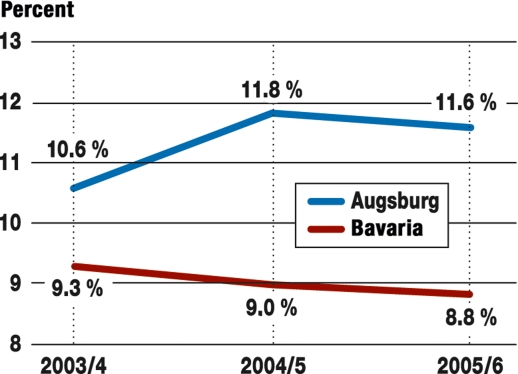
In recent years, the percentage of schoolchildren in Augsburg with overweight or obesity has been substantially higher than the Bavaria average (8). During the 2005/2006 school year, 11.6% of children starting school were overweight, including 5.5% who were obese. In Bavaria as a whole, these figures were 8.8% and 3.4%, respectively (figure 1).
Figure 1.
Prevalence of overweight (incl. obesity) in percent (2003–2006)
The aim of the present study was to determine the prevalence of overweight and obesity among children starting school in Augsburg, to examine possible influencing factors, and to develop a citywide prevention strategy.
Methods
To analyze the current situation, the Augsburg Department of Public Health developed an anonymous questionnaire to survey parents as part of their child’s school entry health examination. The questionnaire consisted of 11 questions about the child’s dietary habits, physical activity patterns, and television viewing time. The child’s first language and the name of his or her preschool were also documented.
During the physical examination, which was performed at the Augsburg Department of Public Health, investigators also recorded each child’s height and body weight. These values were used to calculate the BMI (i.e. the child’s body weight in kilograms divided by the square of his or her height in meters). Overweight was defined as a BMI greater than the 90th percentile for age and sex based on reference data; obesity was defined as a BMI above the 97th percentile. Additional socioeconomic data, such as parental income and education, were not collected.
In total, the parents of 2306 children (i.e. 93.2% of children starting school) participated in the survey. Members of the medical staff were available to assist parents who experienced language or other difficulties in filling out the questionnaire. Investigators recorded each child’s sex, age, body weight, height, and first language. The data were evaluated descriptively using SPSS 14.0.
Results
Prevalence
According to the reference system presented by Kromeyer-Hauschild et al. (9), 13.1% (n = 302) of the 2306 children included in the present study were overweight, including 4.9% (n = 113) who were obese.
The prevalence of overweight and obesity differed by sex. In total, 1125 (48.8%) of the children included in the study were girls and 1172 (50.8%) were boys; nine questionnaires did not specify the children’s sex. Of the girls, 8.7% were overweight and 4.4% were obese; of the boys, 7.7% were overweight and 5.5% were obese. In other words, the girls were more likely than the boys to be overweight, whereas the boys were somewhat more likely than the girls to be obese. However, these differences were not significant (a = 0.05).
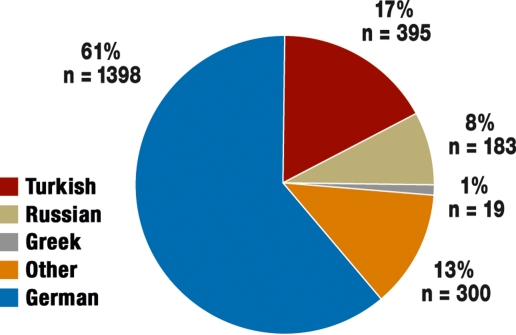
Clear differences could be seen between children with different first languages. Of the 2306 children included in the study, 61% (n = 1398) had German as a first language and 39% (n = 997) had another first language. 17% (n = 395) of the children spoke Turkish and 8% (n = 183) spoke Russian as their first language, making these the second and third most common first languages in our population (figure 2). Overall, children who did not speak German as their first language were twice as likely to be overweight than children who did. Indeed, children from Turkish-speaking families were 2.25 times more likely to be overweight, and 2.53 times more likely to be obese, than children from German-speaking families.
Figure 2.
Native/first languages among children starting school in Augsburg (percent)
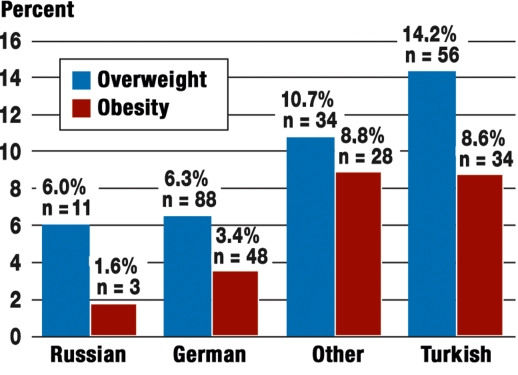
These differences were significant (a = 0.05). Among the children from Russian-speaking families, 7.6% (n = 14) were overweight, including 1.6% (n = 3) who were obese (figure 3). In other words, children from Russian-speaking families were the least likely to be overweight. 13% (n = 300) of the children in our population spoke a first language other than German, Turkish, or Russian (e.g. Croatian, Italian, or Vietnamese). Only 1% (n = 19) of the children were from Greek-speaking families (figure 2). Because the number of children in these language groups was so low, we did not test whether any differences between them were statistically significant. Taken together, 10.7% of the children who spoke Greek or another language other than German, Turkish, or Russian as their first language were overweight and 8.8% were obese (figure 3).
Figure 3.
Overweight and obesity according to first language of children (percent)
In order to provide social services more effectively, the city of Augsburg is divided into four social service regions. Among the children included in our study, variations in the incidence of overweight or obesity between these regions were only marginal.
Physical activity
According to our survey of parents, 50.2% (n = 1157) of all children and 67.3% (n = 76) of obese children did not attend a sports or dance group. As a result, the overall amount of sports activity was correspondingly lower in these groups. Looking at this category in terms of first language reveals that more than 65% of Turkish-speaking children, 59% of Russian-speaking children, and 63.6% of children who had a first language other than German, Turkish, or Russian did not participate in a sports or dance group (table 1).
Table 1. Participation in sports groups among children starting school in Augsburg.
| Children (total) | German | Turkish | Russian | Other | |
| n | 2306 | 1398 | 395 | 183 | 319 |
| One session | 701 | 514 | 83 | 39 | 62 |
| per week | 30.4% | 36.8% | 21.0% | 21.3% | 19.4% |
| Several sessions | 362 | 269 | 29 | 30 | 33 |
| per week | 15.7% | 19.2% | 7.3% | 16.4% | 10.3% |
| None | 1157 | 581 | 260 | 108 | 203 |
| 50.2% | 41.6% | 65.8% | 59.0% | 63.6% | |
| Not specified | 86 | 34 | 23 | 6 | 21 |
| 3.7% | 2.4% | 5.8% | 3.3% | 6.6% |
Other = incl. Greek
Dietary habits
According to data from our survey, 60% of all children had three meals a day, and 33.4% of children had five meals a day. Among the overweight and obese children, roughly two-thirds had three meals, and just under one-fourth had five meals, each day. When broken down by children’s first language, the data show that children from Turkish-speaking families were the least likely (12.4%) to have five meals per day (table 2).
Table 2. Number of meals per day.
| Children (total) | German | Turkish | Russian | Other | |
| n | 2306 | 1398 | 395 | 183 | 319 |
| 2 meals | 53 | 16 | 26 | 4 | 7 |
| 2.3% | 1.1% | 6.6% | 2.2% | 2.2% | |
| 3 meals | 1371 | 743 | 305 | 115 | 204 |
| 59.5% | 53.1% | 77.2% | 62.8% | 63.9% | |
| 5 meals | 771 | 585 | 49 | 53 | 79 |
| 33.4% | 41.8% | 12.4% | 29.0% | 24.8% | |
| More than 5 meals | 38 | 23 | – | 5 | 9 |
| 1.6% | 1.6% | 2.7% | 2.8% | ||
| Not specified | 73 | 31 | 15 | 6 | 20 |
| 3.2% | 2.2% | 3.8% | 3.3% | 6.3% |
Other = incl. Greek
These results are mirrored in the frequency with which parents and children in our study ate together as a family. On the average, overweight and obese children had fewer meals throughout the day, and it is precisely these children who were less likely to eat together with their families. Altogether, 55.3% of the normal-weight children ate together with their families twice each day, compared to 43.4% of the overweight and 45.1% of the obese children. In terms of first language, the majority (59.4%) of children from German-speaking families ate together with their families twice a day. Among children with Turkish as their first language, only 40% ate together with their families twice a day. Nevertheless, a total of 92% of all children ate together with their families at least once a day (table 3).
Table 3. Frequency with which children and parents eat together as a family.
| Children (total) | German | Turkish | Russian | Other | |
| n | 2306 | 1398 | 395 | 183 | 319 |
| Twice a day | 1140 | 831 | 158 | 89 | 157 |
| 53.8% | 59.4% | 40.0% | 48.6% | 49.2% | |
| Once a day | 880 | 484 | 191 | 75 | 125 |
| 38.2% | 34.6% | 48.4% | 41.0% | 39.2% | |
| At least three times a week | 93 | 44 | 26 | 7 | 16 |
| 4.0% | 3.1% | 6.6% | 3.8% | 5.0% | |
| At least once a week | 23 | 12 | 5 | 4 | 2 |
| 1.0% | 0.9% | 1.3% | 2.2% | 0.6% | |
| Never | 1 | 1 | – | – | – |
| 0.0% | 0.1% | ||||
| Not specified | 69 | 26 | 15 | 8 | 19 |
| 3.0% | 1.9% | 3.8% | 4.4% | 6.0% |
Other = incl. Greek
Television viewing
Most normal-weight children in our study watched television or sat in front of a computer for up to one hour each day. Half of the overweight children and 61.9% of the obese children spent between one and three hours in front of a television or computer screen. In terms of first language, some two-thirds of the children from Turkish- and Russian-speaking families spent one to three hours in front of a television or computer screen every day—i.e. twice the rate reported among German-speaking families (table 4).
Table 4. Daily television time (incl. DVD, videos, computer).
| Children (total) | German | Turkish | Russian | Other | |
| n | 2306 | 1398 | 395 | 183 | 319 |
| < 1 hour | 1104 | 812 | 122 | 44 | 122 |
| 47.9% | 58.1% | 30.9% | 24.0% | 38.2% | |
| 1 – 3 hours | 990 | 459 | 234 | 126 | 166 |
| 42.9% | 32.8% | 59.2% | 68.9% | 52.0% | |
| > 3 hours | 61 | 19 | 21 | 5 | 15 |
| 2.6% | 1.4% | 5.3% | 2.7% | 4.7% | |
| No television | 89 | 83 | 3 | 2 | 1 |
| 3.9% | 5.9% | 0.8% | 1.1% | 0.3% | |
| Not specified | 62 | 25 | 15 | 6 | 15 |
| 2.7% | 1.8% | 3.8% | 3.3% | 4.7% |
Other = incl. Greek
Discussion
The results of the present study show a clear increase in the prevalence of overweight and obesity among children starting school in the city of Augsburg; this finding goes against the general trend towards a stagnation in the development of these disorders in preschool children (10). Data on children’s height and body weight were also collected during previous school entry health examinations. The prevalence of overweight (including obesity) rose from 11.6% in the 2005/2006 school year to 13.1% in the 2006/2007 school year.
Although the prevalence of overweight is known to be higher in certain socioeconomic groups (11), we did not collect socioeconomic data, such as parental educational level or income, in the present study. We did, however, indirectly analyze the impact of ethnicity on dietary habits and physical activity patterns by asking parents about their children’s first language.
Measuring physical activity and dietary behavior in a valid manner is difficult. In general, the use of questionnaires limits the ways in which data can be interpreted; indeed, self-report and recall methods are not always suitable for collecting this type of data. Although the number of children in the individual groups is small and the results of the present study are based, in part, on parents’ estimates, various aspects of the data show clear and consistent patterns. Moreover, the prevalence rates seen in our study mirror, at a high level, those observed in Bavaria (8) and Germany (4) as a whole.
The present investigation clearly demonstrates that the tendency observed in Augsburg is similar to that seen in the results of the KiGGS study. In the latter, children from immigrant families and with low socioeconomic status were two to three times less likely than their counterparts from nonimmigrant families and with higher socioeconomic status to engage in sports (12). Similarly, the results of the German Report on Sports for Children and Adolescents (Deutscher Kinder- und Jugendsportbericht) show that socially disadvantaged children in Germany are underrepresented in sports clubs (13).
International surveys point to the generally low levels of physical activity among elementary school students, as well as among older students and adolescents. Spontaneous, but more frequent bouts of physical activity correspond to children’s natural patterns of movement (6), which is perhaps simply another way of describing what children know how to do best: play. Children who associate positive experiences with physical activity are more likely to have an active lifestyle as adults.
The Research Institute of Child Nutrition (Forschungsinstitut für Kinderernährung, FKE) in Dortmund has published scientifically based dietary recommendations for young people for many years now (14). It has developed an optimized mixed diet for children called "optimiX," which recommends that children eat five meals spaced throughout the day. In addition to the total number of calories consumed, the nutritional information, including the percentages of fat and carbohydrates, also plays an important role. The choice of food items appropriate for children is illustrated using a pyramid.
Because rituals and norms are usually conveyed unconsciously when people eat together, parents or siblings often take on the role of communicating healthful eating habits. As such, eating together as a family unit is likely the best way to teach proper nutritional habits, as well as receptiveness to new types of food. Importantly, our study shows that families still eat together very frequently. Our findings also suggest that children who do not eat together with their families eat more often and with fewer restrictions, and thus tend to be overweight.
The relationship between television viewing and overweight has been discussed in a number of publications to date. In one systematic review, reducing sedentary behavior appeared to be effective in preventing overweight in schoolchildren (15). As much as twenty years ago, a significant association was found between television viewing and overweight in children (16), as based on data from the National Health Examination Survey in the United States (17). Researchers found a dose-dependent effect of television viewing on the prevalence of overweight. Children often consume snacks while watching TV, a medium in which these very snacks are also advertized. The increased consumption of these energy-dense foods has an additive effect on obesity when combined with sedentary behavior and reduced energy expenditure (18). This is why the information parents provide about their children’s television viewing or computer time can be so illustrative, even if this information is not objective and must therefore be interpreted with caution. As a trend, however, it seems clear that there is a positive correlation between body weight and time spent in front of the television or computer screen.
Preventive measures should begin as early as possible, because it is easier to influence health-related behavior and avoid secondary diseases in children than in adults. In doing so, however, it is important to distinguish between different groups of children in terms not only of age and sex, but also socioeconomic and ethnic background.
Immigrant families are considered a high-risk group in Germany (4). Language skills play an important role in a family’s ability to access government services, as well as in the extent to which families can be reached through prevention programs. Poor language skills often function as a barrier to a more active lifestyle. Information about age-appropriate dietary, physical activity, and television viewing habits should be provided to parents in their native language. Moreover, families’ willingness to make changes is enhanced if ethnic factors, such as culturally and biographically influenced behavior, are taken into account.
To be effective, neighborhood or district-wide interventions require easy and affordable access to good sports and other recreational facilities, also in terms of public transport. Because children between the ages of three and six, in particular, learn by example, special emphasis should be placed on families and family life (19).
By providing insight into the different factors that play a role in the development and prevention of overweight and obesity, our data can serve as the basis for local preventive measures. In Augsburg, the results of our study are being used to design concepts for targeted and feasible prevention strategies together with preschools, daycare facilities, and local sports clubs.
The "1 + 1 = 3 Project," for example, is currently being developed to facilitate the integration of children from immigrant families, as well as physically challenged children, into sports clubs. Incentives for including a child from an immigrant family, or a child with a disability, for every German child who becomes a member are currently being considered at the political level.
The city council has declared that promoting health by facilitating health-enhancing behavior and environments in preschools and elementary schools is one of its key goals. An example of a project that has gained particular support is "Klasse2000"—the most extensive program in Germany for promoting health in elementary schools (20). In addition, under the direction of the Augsburg Department of Public Health, selected schools will take part in the "Unterwegs nach Tutmirgut" project of the Federal Center for Health Education (Bundeszentrale für gesundheitliche Aufklärung, BZgA) (21). The project was designed for elementary schools and addresses the topics of nutrition, physical activity, and stress management. Health authorities in Augsburg are also continuing to encourage healthy eating at schools with educational programs and inventions, such as the "Organic Foods Lunchbox" campaign ("Bio-Pausenbrotbox-Aktion").
Finally, during the past six months, water fountains have been installed at three schools in Augsburg, thus providing a healthy and free alternative to sugary soft drinks and adding to the growing roster of schools participating in this project ("Wasser trinken in Augsburger Schulen").
Conclusion
During school entry health examinations conducted at the Augsburg Department of Public Health in 2006, investigators collected data on children’s first language, as well as on lifestyle factors, such as television viewing time, dietary habits, and physical activity.
Data collected in previous years had already shown that the prevalence of overweight among children starting school in Augsburg was higher than the Bavaria average. In the present study, results for the 2006/2007 school year revealed that the prevalence of overweight and obesity differed according to children’s first language. Children from Turkish-speaking families had the highest prevalence of these disorders.
In the future, collecting BMI data in each year’s cohort of schoolchildren, as well as analyzing the temporal trend in the prevalence of overweight and obesity in Augsburg, will need to be performed in a way that takes linguistic and other differences into account. Moreover, it will be important to analyze the ways in which potential influencing factors interact with one another.
The development of body weight in children starting school should be examined based on individual language groups and in comparison to one another. Doing so will facilitate the design and implementation of preventive measures that are both concrete and targeted towards groups that are at a high risk for developing overweight or obesity.
Acknowledgments
Dedication
We would like to dedicate this paper to Dr. med. Traude Löscher, our director for many years.
Translated from the original German by Matthew D. Gaskins.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Koletzko B, Dokoupil K, Knoppke B. Powerkids: Ein praktikables Therapiekonzept bei kindlichem Übergewicht. Kinderärztliche Praxis. 2002 [Google Scholar]
- 2.Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–2337. doi: 10.1056/NEJMoa072515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman D, Dietz W, Srinivasan S, Berenson G. The relation of overweight to cardiovascular risk factors among children and adolescents: The Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 4.Kurth B-M, Schaffrath Rosario A. Die Verbreitung von Übergewicht und Adipositas bei Kindern und Jugendlichen in Deutschland. Ergebnisse des bundesweiten Kinder- und Jugendgesundheitssurveys (KIGGS) Bundesgesundheitsblatt. 50:736–743. doi: 10.1007/s00103-007-0235-5. [DOI] [PubMed] [Google Scholar]
- 5.Müller MJ, Kurth BM. Prävention von Übergewicht bei Kindern und Jugendlichen. Prävention und Gesundheitsförderung. 2007;2:240–248. [Google Scholar]
- 6.Biddle S, Sallis JF, Cavill NA. Young people and health-enhancing physical activity-evidence and implications. London: Health Education Authority; 1998. Young and active? [Google Scholar]
- 7.Czerwinski-Mast M, Danielzik S, Asbeck I, Langnäse K, Spethmann C, Müller M. Kieler Adipositaspräventionsstudie (KOPS) Bundesgesundheitsblatt. 2003;46:727–731. [Google Scholar]
- 8.Bayerisches Landesamt für Gesundheit und Lebensmittelsicherheit. Ergebnisse der Schuleingangsuntersuchung zum Schuljahr 2005/2006. [Google Scholar]
- 9.Kromeyer-Hauschild K, Wabitsch M, Kunze D. Perzentilkurven für den Body-Mass-Index. Monatsschr Kinderheilk. 2001;149:807–818. [Google Scholar]
- 10.Bayerisches Landesamt für Gesundheit und Lebensmittelsicherheit. Übergewicht und Adipositas bei Kindern in Bayern. Gesundheitsmonitor Bayern. 2004;2:1–6. [Google Scholar]
- 11.Wabitsch M, Hauner H. Übergewicht und Adipositas bei Kindern und Jugendlichen. Pro-Jugend. 2005;3:10–15. [Google Scholar]
- 12.Lampert T, Starker A, Mensink G. Sport und Bewegung. Robert Koch-Institut Berlin KIGGS Symposium. www.kiggs.de/experten/downloads/dokumente/ppt_SportBewegung.pdf.
- 13.Schmidt W, Hartmann-Tews I, Brettschneider WD. Erster deutscher Kinder- und Jugendsportbericht. Schorndorf: Hofmann-Verlag; 2003. pp. 275–289. [Google Scholar]
- 14. www.fke-do.de.
- 15.Mulvihill C, Quigley R. Evidence briefing. London: Health Development Agency (HDA); 2003. The management of obesity and overweight: An analysis of reviews of diet, physical activity and behavioural approaches. [Google Scholar]
- 16.Dietz W, Gortmaker S. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985;75:807–812. [PubMed] [Google Scholar]
- 17.National Health and Nutrition Examination Survey. www.cdc.gov/nchs/nhanes.htm.
- 18.Andersen R, Crespo C, Bartlett S, Cheskin L, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children. JAMA. 1998;12:938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 19.Graf C, Koch B, Dordel S, et al. Prävention von Adipositas durch körperliche Aktivität - eine familiäre Aufgabe. Dtsch Arztebl. 2003;100(47):A 3110–A 3114. [Google Scholar]
- 20.Storck C, Dupree T, Dokter A, Bölcskei PL. Zwischen Wunsch und Wirklichkeit: Die langfristige Umsetzung schulbasierter Präventionsprogramme in der Praxis am Beispiel Klasse 2000. Präv Gesundheitsf. 2007;2:19–25. [Google Scholar]
- 21. www.tutmirgut.net.