Abstract
The aim of this study was to test how practitioners’ pain communication affects the pain information provided by older adults. A posttest only double blind experiment was used to test how the phrasing of practitioners’ pain questions, open-ended and without social desirability bias; closed-ended and without social desirability bias; or open-ended and with social desirability bias, affected the pain information provided by 312 community living older adults with osteoarthritis pain. Older adults were randomly assigned to one of the three pain phrasing conditions to watch and orally respond to a computer displayed videotape of a practitioner asking about their pain. All responded to a second videotape of the practitioner asking if there was anything further they wanted to communicate. Lastly all responded to a third videotape asking if there was anything further they want to communicate about their pain. Transcripts of the audio taped responses were content analyzed using 16 a priori criteria from national guidelines to identify important pain information for osteoarthritis pain management. Older adults described significantly more pain information in response to the open-ended question without social desirability. The two follow up questions elicited significant additional information for all three groups, but did not compensate for the initial reduced pain information from the closed-ended and social desirability biased groups. Initial use of an open-ended pain question without social desirability bias and use of follow-up questions significantly increases the amount of important pain information provided by older adults with osteoarthritis pain.
Keywords: pain, osteoarthritis, communication, elderly
Deficiencies in pain communication continue between practitioners and patients. Physicians discussed pain during only 72% of the outpatient palliative care visits and initiated the pain topic only half of the time.1 Forty-three percent of the terminally ill inpatients encouraged to talk with their physicians about their pain continued to have pain problems at hospital discharge, and less than half received a pain intervention.2 Even when pain communication was increased between postoperative patients and their practitioners, increased pain relief did not result, perhaps because communication was restricted to discussing pain treatments, and asking the patient to alert practitioners when pain occurred.3 Patients and practitioners need research-based support to help them communicate about pain in ways that lead to greater pain relief for patients. Older adults are a particularly vulnerable to pain. A total of 12.1% of adults age 60 and older have symptomatic osteoarthritis of the knee,4 yet many older adults remain unaware of effective treatment options.5 The purpose of the current study was to test the effect of practitioners asking patients an open-ended question about pain that did not encourage a socially desirable response.
Reasons for the inadequate pain communication might be directly attributable to the way that practitioners speak with patients. Constructing pain assessment questions in the form of social conversation (i.e. “How are you today?”) encourages patients to respond in a socially desirable manner by suppressing their pain concerns.6,7 These types of approaches might be seen as directing social exchange rather than soliciting important clinical assessment data. Giving little attention to patients’ reports of pain, and controlling pain communication by interrupting patients, minimizing or dismissing the reports of pain, and curtailing patient responses to yes/no responses were techniques observed to be used by physicians in a descriptive study of oncology patients consulting with their physicians.7 Again, these methods of asking for pain information solicit a directed response rather than merely asking a patient, “Tell me about your pain.” Physicians challenged and attempted to disconfirm biological explanations for the pain, insisting on psychological explanations when talking with chronic pain patients who had no apparent medical reason for their pain.8 Patients who were subjected to a biasing statement suggesting where their pain would be felt reported significantly more referred pain, and more intense pain than patients not subjected to the biasing statement.9 The preceding communication techniques thwart complete and accurate pain discussions between patients and practitioners. Randomized controlled clinical trials are needed to link specific pain communication strategies to patient outcomes.
Promising interventions to assist patients to describe their pain have been tested, such as individual coaching prior to an office visit,10 and combinations of written scripts and individual coaching.11 Both interventions resulted in a significant decrease in pain. These findings suggest that patients can be assisted to effectively communicate their pain and receive interventions that significantly reduce their pain. The cost of the individual coaching interventions might limit the widespread use of coaching interventions, however. Both studies involved patients with cancer pain. Individual coaching interventions for patients with different pain etiologies might not be as effective in eliciting more responsive pain management from practitioners.
Health care communication research provides helpful insight into communication factors that might influence pain management. The Bayer Institute for Health Care Communication literature review on health care practitioner and patient communication identified only six medical studies that examined eliciting patients’ agenda.12 All six were limited to descriptive medical studies. Primary care physicians interrupted opening statements by their patients during 77% of the visits, and patients completed only 1 out of 52 interrupted statements.13 Physician communication remained virtually unchanged 12 years later when physicians again interrupted 72% of the opening statements.14 Physicians starting off with an open-ended question to delineate the patient’s problem identified significantly more patients with emotional distress than physicians not taught problem defining skills. Six months later patient distress remained significantly reduced for patients of physicians using problem defining communication skills.15 Ability to gather or omit potentially important information from patients is influenced by how health care practitioners communicate with patients.
Communication Accommodation Theory (CAT) describes the motivations and behaviors of people as they adjust their communication in response to their own needs and the perceived behavior of the person with whom they are communicating.16,17 Paying attention to the other person when communicating provides information that can enhance communication. Attention strategies include evaluating the social aspects of the communication interaction, such as selecting and sharing a topic; and identifying the relationship between the communicators.18 Studies of communication between older adults and nurses,19 and physicians and adult patients20 have used CAT to examine health care practitioner lack of accommodation towards their patients.
Within the context of pain management communication CAT provides strategies that practitioners can use to enhance communication with patients. For example, practitioners could use a topic sharing strategy by using an open-ended question to inquire about pain, allowing patients more freedom to respond in the way they feel most helpful in communicating their pain. An interpersonal control strategy by practitioners would be to avoid phrasing questions about pain in a socially desirable way, clarifying that the pain communication is taking place within a health care rather than a social context. Testing how different strategies affect pain communication between practitioners and patients can lead to more effective use of the communication strategies to decrease pain. The following hypothesis was tested:
Older adults asked about their pain with an open-ended question without social desirability bias will describe more important pain information and omit less information than older adults asked about their pain with a closed-ended question without social desirability or an open-ended question with social desirability bias.
Method
Design
A posttest only randomized double blind experiment was used to test how the phrasing of health care practitioners’ pain question, open-ended without social desirability, closed-ended without social desirability, or open-ended with social desirability bias, affected the pain information provided by older adults with chronic osteoarthritis pain. To control for the covariate pain measurement effect, half of each of the three groups responded to the Brief Pain Inventory Short Form (BPI-SF) before watching the videos, and the remaining half responded after watching the final video.
Sample
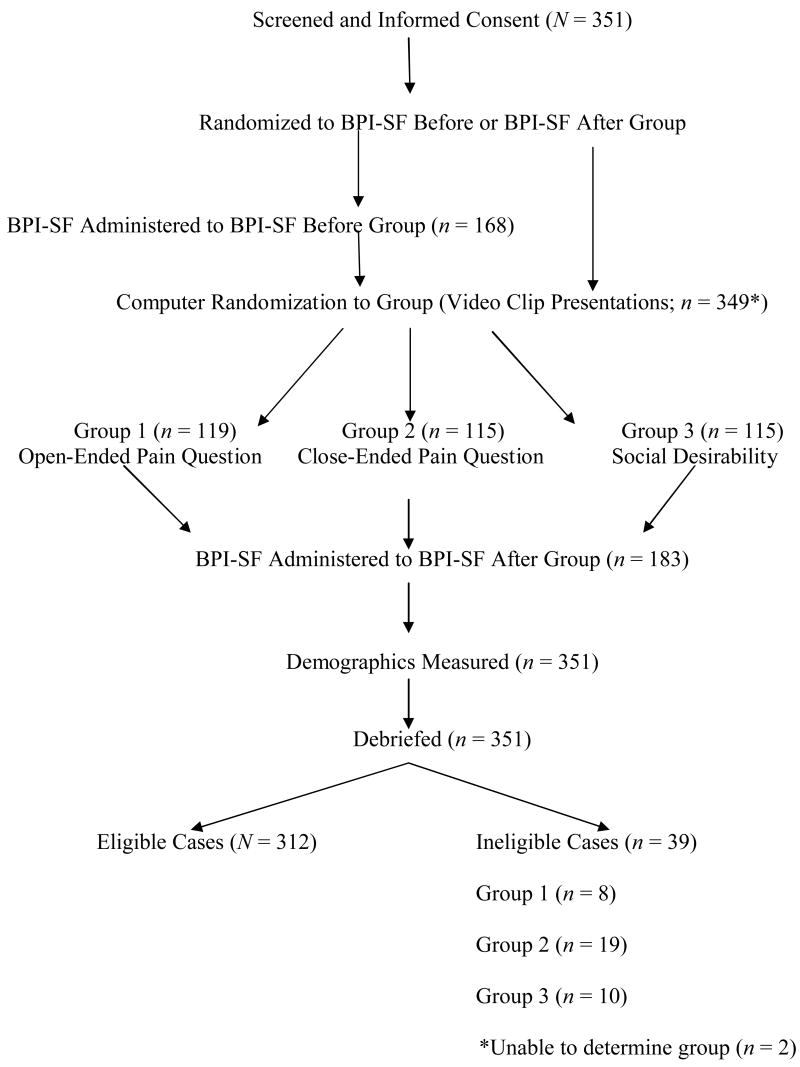
Older adult participants were recruited from 15 urban and suburban independent living congregate housing sites for older adults in eight cites and towns in one state located in the northeastern United States. Inclusion criteria consisted of community dwelling adults, age 60 and older who spoke, read, and understood English; and who reported osteoarthritis pain. People with self identified malignant pain were excluded. Figure 1 depicts the flow of participants from recruitment through completion of the study. A sample size of 300 was needed for a multivariate analysis of covariance (MANCOVA) with three groups (open-ended without social desirability, closed-ended without social desirability, or open-ended with social desirability bias), two dependent variables (pain information included and pain information omitted), .05 level of significance, .80 power, and a small estimated effect size.21 The final sample consisted of 312 older adults.
Figure 1.
Procedure
The study was approved for human subjects’ protection by the University Institutional Review Board. Data collection took place from July 2006 to July 2007. Older adults were recruited and screened for eligibility by one of two trained research assistants (RA). Informed consent was obtained from all participants.
A cover story was provided to increase experimental realism and to decrease response bias. Participants were told that the study was testing the feasibility of helping people prepare for their health care office visit while waiting in the office for their appointment. Participants were randomized to one of the three conditions by the SuperLab 3.0 computer software program, keeping the RA blind to the condition. A web-based random number generator was used to randomize oral administration of the Brief Pain Inventory Short Form (BPI-SF) to before or after the videotape portion of the study to control for pain differences among groups and the effect of BPI-SF timing. Following brief computer training, participants were left alone in the room to view and orally respond to three separate computer-generated videotape of a female health care practitioner asking questions about their pain. After completing their oral response, participants used the touch screen to continue to the next practitioner question. Responses were audiotaped. The first videotape differed across the three groups. The second and third videotapes were the same across groups. Demographic information was collected last prior to debriefing participants. Debriefing consisted of questioning to determine whether participants remained blind to the specific purpose of the study, and providing a more in-depth explanation of the study.
Participants’ oral responses to the practitioner’s first pain question were transcribed and content analyzed for included pain information. Oral responses to the second and third practitioner questions which were the same across the three groups were transcribed and content analyzed to measure pain information omitted when responding to the first pain question.
Experimental Conditions
The randomized video clips consisted of the same female healthcare practitioner stating one of the following initial statements corresponding to the three experimental conditions.
Tell me about your pain, aches, soreness, or discomfort (open-ended and without social, desirability).
What would you rate your pain, aches, soreness, or discomfort on a 0 to 10 scale with 0, no pain, and 10 the worst pain possible (closed-ended and without social desirability bias)?
How are you feeling (social desirability bias)?
The second practitioner video consisted of the practitioner asking all participants, “What else can you tell me?” The third and final practitioner video consisted of the practitioner asking, “What else can you tell me about your pain, aches, soreness or discomfort?” The video clips comprising the three experimental conditions were reviewed by a panel of three health care practitioners who deemed the video clips to have adequate face validity, and to be comparable regarding nonverbal communication, voice tone, and inflection. In response to the expert panel suggestion, an oral prompt instructing the participants to touch the screen to continue was added to reinforce the visual prompt. The researchers noted after approximately 100 participants had completed the study that the oral prompt appeared to interrupt responses from the participants. The oral prompt was removed for the remaining participants, and entered as an additional variable in the study.
Measures
Brief Pain Inventory Short Form (BPI-SF) Pain Measure
The BPI-SF consistes of 15 questions that measure pain location, intensity, pain treatment, and functional interference of pain on mood and every day activities. Cronbach’s alpha for the overall BPI-SF has been reported as .77 to .87.22,23 For the current study the overall BPI-SF internal consistency was α= .87. Validity of the BPI-SF has been evidenced by a correlation of r = 61, p < .001 with the Short Form McGill Pain Questionnaire (SF-MPQ).23
Demographic Form
Older adults’ demographic information was measured for the following information: age, gender, race, ethnic group, marital status, highest completed education, if they were currently followed by a health care practitioner for their osteoarthritis and for their osteoarthritis related pain.
Analysis
Content Analysis of Included and Omitted Pain Information
The American Pain Society Guidelines for the Management of Pain in Osteoarthritis, Rheumatoid Arthritis, and Juvenile Chronic Arthritis24 was used to identify important osteoarthritis pain management content included or omitted from older adults’ transcribed responses to the practitioner’s pain communication question. The 16 a priori osteoarthritis pain management criteria included type of pain (nociceptive/neuropathic), quality of pain, source, location, intensity, duration/time course, pain affect, effect on personal lifestyle, functional status, current pain treatments, use of recommended glucosamine sulfate, effectiveness of prescribed treatments, prescription analgesic side effects, weight management to ideal body weight, exercise regimen or physical therapy and/or occupational therapy, and indications for surgery.
Krippendorff’s25 components for content analysis were used to content analyze transcripts of the responses to the practitioner questions. The unit of analysis was any word or phrase that described one of the a priori criteria. One point was given for each word or phrase describing a criterion. Repeated use of the same word or phrase was counted only the initial time. Each distinctly different word or phrase about the same criterion was credited with one point.
Coding was conducted by two trained, independent RA’s who were blind to participants’ condition. Coding disagreements were noted in order to determine inter-rater reliability, and disagreements were resolved through discussion. Inter-rater reliability was calculated for the content analysis using Krippendorff’s25 more conservative formula for alpha where α = 1 –(Do/De) with Do the measure of observed disagreements and De the measure of disagreements expected by chance (.50). The content analysis resulted in 285 rater disagreements and 1833 rater agreements across a total of 2118 observations. The inter-rater reliability was .73. The percent agreement of 1833 agreements out of a total of 2118 observations was 86.5%.
The coded data was entered into an SPSS database. The included pain communication score was calculated by summing all of the important pain content described by participants in response to the first practitioner pain question. The omitted important pain information was calculated by summing all important pain content described by participants in response to the practitioner’s two follow up questions.
Results
A total of N = 351 older adults completed the study. Despite screening only 312 of those participants were eligible for the study. Reasons for ineligibility included absence of arthritis pain, insufficient English language skills, less than 60 years of age, and presence of malignant pain. For example, participants who responded that they currently had osteoarthritis pain during screening, but who indicated no current pain when responding to the BPI-SF were identified as ineligible. Spanish speaking participants who stated that they spoke, read, and understood English, but who were unable to orally respond to the videos were also identified as ineligible. Eligible older adults did not differ from ineligible older adults in pain intensity, pain interference, pain relief, number of pain sites, number of pain treatments, practitioners’ treatment for arthritis, practitioners’ treatment for pain, age, gender, race, ethnic group, or education. The two method variables, order of the BPI-SF (before or after responding to the practitioner questions) and use of the oral prompt also did not differ between eligible and ineligible participants. Use of the oral prompt neared significance, however, χ2(1) = 3.74, p < .053. There was a trend for more ineligible participants in the oral prompt condition, 46.2% versus 30.8% of eligible participants. Significantly more ineligible participants were in the closed-ended group, χ2(2) = 6.58, p < .04, with n = 8 (21.6%), n = 19 (51.4%), and n = 10 (27.0%) of open-ended, closed-ended, and social desirability bias group ineligible participants, respectively.
Table 1 contains means and standard deviations and Table 2 contains frequencies from the descriptive statistics for the full sample of N = 312; and the open-ended, closed-ended, and social desirability biased groups. The three groups did not differ significantly in pain intensity, pain interference, pain relief, number of pain sites, number of pain treatments, practitioners’ treatment for arthritis, practitioners’ treatment for pain, age, gender, race, ethnic group, or education. Frequency of the two method variables, timing of the BPI-SF (before or after responding to the practitioner questions) and use of the oral prompt also did not differ between the three groups. The interaction effect of BPI-SF timing and groups was not significant for included or omitted pain information; for present pain intensity, or for pain interference. The timing effect of the BPI-SF was not included in any further analyses as a result of the insignificant effect.
Table 1.
Full Sample and Group Means and Standard Deviations
| Variable | Full | Open-ended | Closed-ended | Social Desirable |
|---|---|---|---|---|
| N = 312 | n = 111 | n = 96 | n = 105 | |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Age | 75.6 (8.50) | 76.4 (8.53) | 75.4 (8.03) | 75.0 (8.90) |
| %Pain Relief* | 67.2 (28.89) | 65.1 (30.80) | 67.8 (28.03) | 68.9 (27.68) |
| Pain Intensity** | 4.6 (1.90) | 4.5 (1.84) | 4.6 (1.97) | 4.7 (1.90) |
| Functional Pain*** | 4.2 (2.47) | 4.0 (2.39) | 4.1 (2.54) | 4.6 (2.48) |
Pain relief percentage was measured on the BPI-SF 0 to 100% scale.
Pain intensity was the computed as the mean of the four BPI-SF 0 – 10 pain intensity items.
Functional pain was computed as the mean of the seven BPI-SF 0 – 10 functional interference items.
Table 2.
Full Sample and Group Frequencies
| Variable | Full | Open-ended | Closed-ended | Social Desirable |
|---|---|---|---|---|
| N = 312 | n = 111 | n = 96 | n = 105 | |
| N (%) | n (%) | n (%) | n (%) | |
| Women | 225 (72.3) | 79 (71.2) | 72 (75.0) | 74 (71.2) |
| Hispanic | 24 (7.9) | 7 (6.4) | 9 (9.6) | 8 (7.8) |
| Race | ||||
| Am Indian | 4 (1.3) | 0 (0.0) | 1 (1.0) | 3 (2.9) |
| Asian | 1 (0.3) | 0 (0.0) | 0 (0.0) | 1 (1.0) |
| Black | 74 (23.8) | 26 (23.4) | 28 (29.2) | 20 (19.2) |
| Pacific Islander | 1 (0.3) | 0 (0.0) | 0 (0.0) | 1 (1.0) |
| White | 213 (68.5) | 77 (69.4) | 64 (66.7) | 72 (69.2) |
| Multiracial | 18 (5.8) | 8 (7.2) | 3 (3.1) | 7 (6.7) |
| HS Education or > | 198 (64.1) | 75 (68.2) | 59 (62.1) | 64 (61.5) |
| Tx for Arthritis | 229 (73.9) | 83 (75.5) | 65 (67.7) | 81 (77.9) |
| Tx for Pain | 200 (64.5) | 71 (64.5) | 57 (59.4) | 72 (69.2) |
Pearson’s r correlations were calculated between included and omitted important pain information on the one hand, and the two a priori covariates, present pain intensity and functional interference from pain, in order to examine the relationship between the variables. Present pain intensity was unrelated to included or omitted pain information, r = −.07, p < .24 and r = .09, p < .12, respectively. Functional interference from pain was unrelated to included pain information, r = .02, p < .68, and slightly related to omitted pain information, r = .13, p < .02. Functional pain interference was retained as a covariate for the multivariate analysis of variance.
Multivariate analysis of covariance with functional pain interference as the covariate was used to test for differences between the three groups (open-end, closed-ended, and social desirability biased) on the two response measures, included and omitted pain information. Groups differed significantly, Wilk’s Lamba = 0.646, F( 4, 614) = 37.46, p < .001, partial eta2 = .20, and eta2 = .35. Functional interference with pain as the covariate also was significant, Wilk’s Lambda = 0.974, F(2, 307) = 4.09, p < .02, partial eta2 = .03, and eta2 = .026. Univariate tests for between subjects effects demonstrated that included information was significantly different between the groups, F(2,308) = 79.89, p < .001, partial eta2 = .34, eta2 = .20; but that omitted information was not significantly different, F(2,308) = 2.61, p < .08. Functional interference with pain was not significantly different for included pain information, F(1,308) = 2.69, p < .10; but was significantly different for omitted pain information, F(1,308) = 5.86, p < .02, partial eta2 = .02, eta2 = .006. Table 3 contains the means and standard deviations for included and omitted important pain information across the open-ended, closed-ended, and social desirability biased groups.
Table 3.
Group Means and Standard Deviations for Included and Omitted Pain Information (N = 312)
| Pain Information | Open-ended | Closed-ended | Social Desirability |
|---|---|---|---|
| n = 111 | n = 96 | n = 105 | |
| M (SD) | M (SD) | M (SD) | |
| Included | 3.6 (2.46) | 1.4 (1.61) | 0.5 (1.23) |
| Omitted | 3.8 (2.42) | 4.6 (2.86) | 4.0 (2.77) |
Multivariate analysis of variance was conducted to compare the three groups without functional interference with pain as the covariate in order to conduct post hoc tests for groups differences on included and omitted important pain information, Wilks’ Lambda = 0.651, F(4, 616) = 36.82, p < .001, partial eta2 = .19, eta2 =.35. Post hoc Scheffe’ tests for included important pain information demonstrated significant differences between the open-ended and closed-ended group, p < .001, 95% CI = 1.60 to 2.87; open-ended and social desirability bias group, p <. 001, 95% CI = 2.44 to 3.69; and closed-ended and social desirability group, p < .007, CI = 0.18 to 1.48. In contrast, post hoc Scheffe’ tests for omitted important pain information demonstrated no significant differences between groups.
One-way ANOVA was conducted to clarify how groups differed on the total amount of important pain information in response to the first, second and third three practitioner questions. Groups differed significantly, F(2,309) = 20.10, p < .001 with group means for the open-ended, closed-ended, and social desirability group M = 7.4 (SD = 3.76), M = 6.0 (SD = 3.10), and M = 4.5 (SD = 3.10), respectively. Post hoc Scheffe’ tests supported significant differences between the open-ended and closed-ended group, p < .009, CI = 0.29 to 2.59; and open-ended and social desirability group, p < .001, CI = 1.77 to 4.01; and closed-ended and social desirability group, p < .01, CI = 0.29 to 2.62.
Discussion
Phrasing of the practitioner’s pain questions significantly impacted the amount of important pain information provided by older adults. Use of an open-ended question, “Tell me about your pain, aches, soreness, or discomfort” resulted in significantly more pain information than the closed-ended question, “What would you rate your pain, aches, soreness, or discomfort on a 0 to 10 scale with 0, no pain, and 10 the worst pain possible?,” or the social desirability biased question, “How are you feeling?” The addition of two to three additional items of pain information might significantly impact pain treatment, with a more tailored pain management approach for each older adult. Use of an open-ended pain question conveys a more collaborative relationship. As predicted by Communication Accommodation Theory18 the practitioner’s use of the open-ended pain question encouraged a greater exchange of information.
Practitioners continue to inadequately assess pain across different clinical contexts ranging from acute care patients with hip fractures26 and cancer27 to long term care facility patients.28 The current study provides direct evidence about the impact of open-ended pain questions on patients’ report of important pain information. The findings should encourage health care practitioners across practice settings to routinely use open-ended pain questions when initiating pain assessment dialog with their patients.
Initial phrasing of the pain question impacted the total amount of pain information provided by older adults, even after the practitioner asked two additional questions to elicit further information. The results might be explained by the primacy effect29,30 where an initial stimulus has greater impact on attitudes than subsequent stimuli. Older adults might be influenced more to select pain information in response to practitioners’ pain questions rather than their need to convey specific pain information. Older adults might be inexperienced in communicating pain information to their practitioners,31 assume that the practitioner knows best about the pain management,32 or forget to bring up an important pain issue once they have been distracted by responding to other questions. The finding that the open-ended group responded with more pain information overall, even after all groups were asked the open-ended question as the final question indicates the importance of initially using an open-ended pain question in order to maximize the exchange of pain information.
Contrary to the hypothesis, omitted pain information (responses to the two follow up questions) was not less for the open-ended group. All three groups responded with similar clinically significant amounts of additional pain information. Compared to the amount of information provided in response to the initial question, the open-ended group doubled their amount of pain information, while the closed-ended group tripled, and the social desirability biased group increased by nearly 8-fold the amount of pain information. Follow up questions were important for eliciting additional important pain information, and should be routinely used with older adults even after initiating the pain communication with an open-ended question.
As predicted by Communication Accommodation Theory, asking about pain in a socially desirable way, “How are you feeling?” resulted in the least amount of communicated pain information across the three groups. Practitioners need to clearly identify that the context of the pain management discussion is a clinical context, and avoid unconsciously suggesting a social context. More neutrally phrased initial greetings such as “tell me what brought you in today” might encourage more clinically focused pain discussions, and reduce socially desirable responses. Patient centered communication has been identified as important in clinical practice.33 Results from the current study indicate the impact on older adults of using patient centered communication strategies.
Responding to the Brief Pain Inventory Short Form (BPI-SF) before or after responding to the practitioner pain questions had no effect on the amount of pain information communicated by older adults. BPI-SF questions included direct face to face questioning by the research assistant about pain location, intensity, treatments, the percent of relief from pain treatments, and multiple items regarding how pain interferes with functional status such as walking and sleeping. While communication prompts from the BPI-SF had no effect on pain communication, the practitioner pain questions produced a significant effect. Pain location, intensity, interference with function, pain treatments, and pain relief from treatments was described by some older adults in response to the practitioner questions. The reasons remain unclear as to the absence of a relationship between timing of the BPI-SF administration and the amount of pain communication by older adults. While coaching interventions have been shown as effective in assisting oncology patients to communicate more about their pain during healthcare visits10,11 responding to the BPI-SF does not appear to “coach” older adults to communicate more about their osteoarthritis pain.
Functional interference from pain as measured by the BPI-SF was unrelated to the amount of pain information provided in response to the first practitioner question, but was slightly related to information provided in response to the two follow up questions. Older adults might perceive functional interference from their chronic osteoarthritis pain (e.g. difficulty walking) as a normal part of aging.34 The finding reinforces the need to ask additional pain questions to elicit pain information about functional interference. Present pain intensity was unrelated to pain communication. In a previous study, older adults’ pain ratings using an 11-point Verbal Numeric Rating Scale were reliable and valid when the pain stimuli was an experimentally induced acute thermal pain,35 supporting older adults’ ability to use a pain intensity scale to report acute pain. The BPI-SF functional pain interference subscale might be a more psychometrically sound pain measure than the BPI-SF present pain intensity subscale when measuring chronic osteoarthritis pain in older adults.
Results must be considered within the context of some study limitations. The older adults’ pain communication was computed by summing the number of distinct items of pain information with which the older adults responded. Although all pain information items included in the analyses were important according to a priori criteria from the American Pain Society Guidelines for the Management of Pain in Osteoarthritis, Rheumatoid Arthritis, and Juvenile Chronic Arthritis,24 importance might vary with the context of the pain situation. For example description of loss of ability to walk due to the pain would generally be considered more critical information than identification of a fourth pain site. Glucosamine was included as an important item of pain information although more recent evidence no longer supports the effectiveness of glucosamine in reducing pain overall.36,37 The rationale for retaining glucosamine was the finding from Clegg and colleagues that glucosamine in combination with chondroitin might decrease moderate-severe pain, and the importance of continued discussion with older adults about appropriate use or nonuse of glucosamine for osteoarthritis pain. Significantly more ineligible participants were in the closed-ended group, possibly reflecting increased difficulty understanding and responding to the 0 to 10 pain intensity scale. The study used a computer displayed practitioner videotape to pose the pain questions. Older adults were trained to use the touch screen prior to beginning the study, and required only to touch the computer screen after answering each practitioner question. Older adults might have been uncomfortable using the touch screen computer, and responded differently as a result. Older adults also might respond differently to a practitioner posing the question face to face. The potential limitation was counterbalanced by the increased treatment fidelity38 of using a videotape rather than face to face format. Furthermore, ecological validity was increased through use of the cover story. Older adults were told that the purpose of the study was to test the feasibility of using a computer to gather preliminary health information while waiting in the practitioner’s office for a health visit. Ecological validity was further increased through the use of videotapes of an actual healthcare practitioner filmed in a health center examination room.
Results from the current study suggest areas for further research. Research is needed to test how teaching practitioners to initiate the pain discussion with an open-ended pain question and to use follow up questions affects practitioners’ subsequent pain discussions and their patients’ pain outcomes. Research is also needed to test how teaching patients about the effect of pain question phrasing on their own pain responses affects their subsequent pain discussions and pain outcomes. Studies examining how the content of patients’ pain communication varies with factors such as age, gender, race, language, malignant versus nonmalignant pain, or chronic versus acute pain are important to determine how to tailor pain communication for more effective discussions. Testing other communication strategies from Communication Accommodation Theory such as the effect of the explicitness of patients’ pain information on practitioners’ pain treatment response might provide additional ways to enhance practitioner and patient pain communication.
Older adults in the current study reported that they experienced moderate pain intensity and functional pain interference. Innovative approaches are needed to assist patients such as these older adults to reduce their pain. Improving communication about pain between patients and their health care practitioners provides a crucial starting point for achieving greater pain relief for older adults.
Acknowledgments
The Project described was supported by Grant Number 5 R21NR009848-02 from the National Institute of Nursing Research. The contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH.
Contributor Information
Deborah Dillon McDonald, 12 Town Line Drive, East Hampton, CT 06424, University of Connecticut, (Email) Deborah.mcdonald@uconn.edu
Maura Shea, 21 Sunrise Drive, Avon, CT 06001, University of Connecticut
Leonie Rose, 103 Capen Street, Windsor, CT 06095, University of Connecticut.
John Fedo, 147 Evergreen Street, Providence, RI 02906, University of Connecticut
References
- 1.Detmar S, Muller M, Wever L, Schornagel J, Aaronson N. Patient-physician communication during outpatient palliative treatment visits. JAMA. 2001;285:1351–357. doi: 10.1001/jama.285.10.1351. [DOI] [PubMed] [Google Scholar]
- 2.Desbiens N, Wu A, Yasui Y, et al. Patient empowerment and feedback did not decrease pain in seriously ill hospitalized adults. Pain. 1998;75:237–46. doi: 10.1016/s0304-3959(97)00225-x. [DOI] [PubMed] [Google Scholar]
- 3.Carlson J, Youngblood R, Dalton J, Blau W, Lindley C. Is patient satisfaction a legitimate outcome of pain management? J Pain Symptom Manage. 2003;25:264–75. doi: 10.1016/s0885-3924(02)00677-2. [DOI] [PubMed] [Google Scholar]
- 4.Dillon C, Rasch E, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the third National Health and Nutrition Examination Survey 1991–1994. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 5.Hill J, Bird H. Patient knowledge and misconceptions of osteoarthritis assessed by a validated self-completion knowledge questionnaire (PKQ-OA) Rheumatol. 2007;46:796–800. doi: 10.1093/rheumatology/kel407. [DOI] [PubMed] [Google Scholar]
- 6.McDonald D, McNulty J, Erickson K, Weiskopf C. Communicating pain and pain management needs after surgery. Appl Nurs Res. 2000;13:70–75. doi: 10.1016/s0897-1897(00)80003-8. [DOI] [PubMed] [Google Scholar]
- 7.Rogers M, Todd C. The “right kind” of pain: talking about symptoms in outpatient oncology consultations. Palliat Med. 2000;14:299–307. doi: 10.1191/026921600669288537. [DOI] [PubMed] [Google Scholar]
- 8.Kenny D. Constructions of chronic pain in doctor-patient relationships: bridging the communication chasm. Patient Educ Couns. 2004;52:297–305. doi: 10.1016/S0738-3991(03)00105-8. [DOI] [PubMed] [Google Scholar]
- 9.Branch M, Carlson C, Okeson J. Influence of biased clinician statements on patient report of referred pain. J Orofac Pain. 2000;15:120–127. [PubMed] [Google Scholar]
- 10.Oliver J, Kravitz R, Kaplan S, Meyers F. Individualized patient education and coaching to improve pain control among cancer outpatients. J Clin Oncol. 2001;19:2206–2212. doi: 10.1200/JCO.2001.19.8.2206. [DOI] [PubMed] [Google Scholar]
- 11.Miaskowski C, Dodd M, West C, et al. Randomized clinical trial of the effectiveness of a self-care intervention to improve Cancer pain management. J Clin Oncol. 2004;22:1713–1720. doi: 10.1200/JCO.2004.06.140. [DOI] [PubMed] [Google Scholar]
- 12.White M, Bonvicini K. Bayer Institute for Health Care Communication annotated bibliography for clinician patient communication to enhance health outcomes. [Accessed January 26, 2005]; available at http://www.bayerinstitute.org/pdfs/biblio/CPC%20Bibliography-2-10-2005.doc.
- 13.Beckman H, Frankel R. The effect of physician behavior on the collection of data. Ann Intern Med. 1984;101:692–696. doi: 10.7326/0003-4819-101-5-692. [DOI] [PubMed] [Google Scholar]
- 14.Marvel M, Epstein R, Flowers K, Beckman H. Soliciting the patient’s agenda have we improved? JAMA. 1999;281:283–287. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- 15.Roter D, Hall J, Kern D, et al. Improving physicians’ interviewing skills and reducing patients’ emotional distress. Arch Intern Med. 1995;155:1877–1884. [PubMed] [Google Scholar]
- 16.Fox S, Giles H. Accommodating intergenerational contact: A critique and theoretical model. J Aging Stud. 1993;7:423–451. [Google Scholar]
- 17.Giles H. Accent mobility. A model and some data. Anthropological Linguistics. 1973;15:87–105. [Google Scholar]
- 18.Coupland N, Coupland J, Giles H, Henwood K. Accommodating the elderly: Invoking and extending a theory. Lang Soc. 1988;17:41. [Google Scholar]
- 19.Ryan E, Hamilton J, See S. Patronizing the old: How do younger and older adults respond to baby talk in the nursing home? Intl J Aging Hum Dev. 1994;39:21–32. doi: 10.2190/M52C-M2D2-R6C2-3PBM. [DOI] [PubMed] [Google Scholar]
- 20.Coupland J, Coupland N. Old age doesn’t come alone: Discursive representations of health-in-aging in geriatric medicine. Intl J Aging and Hum Dev. 1994;39:81–95. doi: 10.2190/2GM4-U3X6-QL19-G9YU. [DOI] [PubMed] [Google Scholar]
- 21.Stevens J. Applied multivariate statistics for the social sciences. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc; 1996. [Google Scholar]
- 22.McDonald D, Thomas G, Livingston K, Severson J. Assisting older adults to communicate their pain after surgery. Clin Nurs Res. 2005;14:109–126. doi: 10.1177/1054773804271934. [DOI] [PubMed] [Google Scholar]
- 23.Zalon M. Comparison of pain measures in surgical patients. J Nurs Meas. 1999;7:135–152. [PubMed] [Google Scholar]
- 24.American Pain Society. Guidelines for the management of pain in osteoarthritis, rheumatoid arthritis, and juvenile chronic arthritis. Glenview, IL: American Pain Society; 2002. [Google Scholar]
- 25.Krippendorff K. Content analysis an introduction to its methodology. 2. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 26.Herr K, Titler M, Schilling M, et al. Evidence-based assessment of acute pain in older adults current nursing practices and perceived barriers. Clin J Pain. 2004;20:331–340. doi: 10.1097/00002508-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Idell C, Grant M, Kirk C. Alignment of pain reassessment practices and national comprehensive cancer network guidelines. Oncol Nurs Forum. 2007;34:661–671. doi: 10.1188/07.ONF.661-671. [DOI] [PubMed] [Google Scholar]
- 28.Williams C, Zimmerman S, Sloane P, Reed P. Characteristics associated with pain in long-term care residents with dementia. Gerontologist. 2005;45:68–73. doi: 10.1093/geront/45.suppl_1.68. [DOI] [PubMed] [Google Scholar]
- 29.Miller N, Campbell D. Recency and primacy in persuasion as a function of the timing of speeches and measurements. J Abnorm Soc Psychol. 1959;59:1–9. doi: 10.1037/h0049330. [DOI] [PubMed] [Google Scholar]
- 30.Petty R, Cacioppo J. Attitudes and persuasion: Classic and contemporary approaches. Dubuque, IA: William C. Brown Company Publishers; 1981. [Google Scholar]
- 31.Sherwood G, Adams-McNeill J, Starck P, Nieto B, Thompson C. Qualitative assessment of hospitalized patients’ atisfaction with pain management. Res Nurs Health. 2000;23:486–495. doi: 10.1002/1098-240X(200012)23:6<486::AID-NUR7>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 32.Zalon M. Pain in frail, elderly women after surgery. J Nurs Scholarsh. 1997;29:21–26. 27. doi: 10.1111/j.1547-5069.1997.tb01135.x. [DOI] [PubMed] [Google Scholar]
- 33.Berrios-Rivera J, Street R, Garcia Popa-Lisseanu M. Trust in physicians and elements of the medical interaction in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum. 2006;55:385–393. doi: 10.1002/art.21988. [DOI] [PubMed] [Google Scholar]
- 34.Appelt C, Burant C, Siminoff L, Kwoh C, Ibrahim S. Arthritis-specific health beliefs related to aging among older male patients with knee and/or hip osteoarthritis. J Gerontol. 2007;62A:184–190. doi: 10.1093/gerona/62.2.184. [DOI] [PubMed] [Google Scholar]
- 35.Herr K, Spratt K, Mobily P, Richardson G. Pain intensity assessment in older adults use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain. 2004;20:207–219. doi: 10.1097/00002508-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Clegg D, Reda D, Harris C, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354:795–808. doi: 10.1056/NEJMoa052771. [DOI] [PubMed] [Google Scholar]
- 37.Towheed T, Maxwell L, Anastassiades M, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2007;3:1–53. doi: 10.1002/14651858.CD002946.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stein K, Sargent J, Rafaeis N. Intervention research establishing fidelity of the independent variable in nursing clinical trials. Nurs Res. 2007;56:54–62. doi: 10.1097/00006199-200701000-00007. [DOI] [PubMed] [Google Scholar]