Abstract
Background
Homeless persons depend disproportionately on the health-care safety net for medical services. National reports identify financial strains to this safety net. Whether this has affected homeless persons is unknown.
Objectives
We quantified changes in the proportion of homeless persons reporting unmet need for health care in Birmingham, Alabama, comparing two periods, 1995 and 2005. We assessed whether a period effect was independent of characteristics of persons surveyed.
Design
Analysis of two surveys conducted with identical methods among representative samples of homeless persons in 1995 (n = 161) and 2005 (n = 161).
Measurements
Report of unmet need (inability to obtain care when needed) was the dependent variable. Two survey periods (1995 and 2005) were compared, with multivariable adjustment for sociodemographic and health characteristics. Reasons for unmet need were determined among the subset of persons reporting unmet need.
Results
Unmet need for health care was more common in 2005 (54%) than in 1995 (32%) (p < 0.0001), especially for non-Blacks (64%) and females (65%). Adjusting for individual characteristics, a survey year of 2005 independently predicted unmet need (odds ratio 2.68, 95% CI 1.49–4.83). Among persons reporting unmet need (87 of 161 in 2005; 52 of 161 in 1995), financial barriers were more commonly cited in 2005 (67% of 87) than in 1995 (42% of 52) (p = 0.01).
Conclusion
A rise in unmet health-care needs was reported among Birmingham’s homeless from 1995 to 2005. This period effect was independent of population characteristics and may implicate a local safety net inadequacy. Additional data are needed to determine if this represents a national trend.
Key words: homeless persons, access to care, safety net, survey
INTRODUCTION
Since the 1980s, research and policy initiatives have sought to address homeless persons’ access to health care.1,2 Studies suggest that lack of insurance and competing priorities (e.g., the requirements of finding a place to sleep, store belongings, etc.) limit homeless persons’ access to care when needed,3,4 which may contribute to high mortality and excess hospital utilization.5–7
In 1996, survey data showed that 24.6% of homeless persons reported inability to obtain care when needed, a figure four times higher than contemporaneous national samples.3,8 Homeless persons rely disproportionately on the health-care safety net, including public hospitals and community health centers,9 as well as the Veterans Health Administration, volunteer clinics, and academic teaching hospitals. Some studies suggest strain on the health-care safety net because of the failure of resources to rise in tandem with demand.10–12 Possible safety net stressors include: (1) rising numbers of uninsured adults,13 (2) restricted federal funds for safety net institutions,11 including limits on Disproportionate Share Hospital payments,14 and (3) state and federally imposed restrictions to Medicaid program growth.15,16 Although the number of community health centers has expanded significantly,17 rising demand by moderate-income persons for community health center services could adversely affect homeless persons’ access to these same centers, many of which receive funding under variants of the federal Health Centers Consolidation Act (typically referred to as Section 330).
These complex changes in the safety net led us to examine whether access to health care has improved or declined for homeless persons in Birmingham from 1995 to 2005, using data from a periodic survey. Our approach was to seek evidence of a potential period effect independent of population characteristics, classed conceptually as Predisposing (related to propensity to use care, such as age, sex, and homeless duration), Enabling (characteristics related to means of accessing care, including finances), and Need (related to illness as objectively measured or subjectively assessed)18. This traditional classification in homeless health services research may help to distinguish individual characteristics from the impact of study year, which may reflect changes in the local safety net environment.19–22
METHODS
This study used two structured surveys of representative samples of homeless individuals in Birmingham, administered 10 years apart by the same investigative team (April-May of 1995; April-May of 2005).23,24 Because recruitment methods (and the survey instrument) were nearly identical, measures of health-care access reported by each sample are expected to be representative of conditions for the referent homeless populations in 1995 and in 2005.
RECRUITMENT AND SURVEY PROCEDURES
In both 1995 and 2005 (January), investigators conducted a point-in-time census of the Metropolitan Statistical Area’s visibly homeless (i.e., persons in shelters, other supervised facilities, and staying outdoors), including all shelters, rehabilitation programs, jails, and emergency rooms, in addition to a street census of the 360-square-block area constituting the defined central district of Birmingham, conducted using standard block-to-block methods.25 For the census and subsequent survey, persons qualified as homeless if they spent the last night on the street, in a car or abandoned building, an emergency shelter, transitional (but not permanent) housing, hotel/motel, hospital or jail, or treatment center.26 These enumeration data were used to frame representative samples for in-depth surveys supervised by the same investigators. 24,27 Samples for the subsequent in-depth surveys in April-May of 1995 (n = 161) and 2005 (n = 161) were random probability cluster samples with set quotas for race, sex, and geographic site based on the enumeration data. Thus, if a given shelter had 10% of the homeless, then 16 (10% of 161) interviews were obtained from that shelter. If one-fourth of the adult occupants of this shelter were white females, then 4 of the 16 interviews would be administered to randomly-selected white females. Limited choices of respondents in smaller shelters or street sites required some adjustments to meet these quotas. Nonetheless, the samples closely matched the community census in regard to race and gender. For example, in the 2005 study the survey sample was 66% male and 34% white compared to 70% and 31%, respectively, in the population enumeration.
The target sample size of 161 was based on effect sizes found in a 1987 survey of Birmingham’s homeless population. Prevalence estimates for major categorical variables have a range of error ±7% for a 95% confidence interval.24,27 For regression analysis, a regression coefficient of.048 was significant (p < 0.05) with 80% power. Previous surveys by two authors (FJR, MEL) found effect sizes larger than 0.048 for important predictor variables in this population.
The response rates were 92% and 88% for the 1995 and 2005 surveys, respectively. Where feasible, shelter staff introduced interviewers to respondents and located private interview spaces. Incentives were $10 in 1995 and $20 in 2005. Informed consent was obtained according to procedures approved by the Institutional Review Board of the University of Alabama at Birmingham.
Persons not surveyed were children (under age 19), persons with severely impaired communication skills, and occupants of facilities sheltering persons with dementia or mental retardation. This enumeration also did not capture unsheltered persons in remote rural areas of the metropolitan statistical area, but previous counts indicated that these individuals were less than 10% of the total homeless population.
Surveys were administered face-to-face by trained interviewers. Interviews covered a wide range of topics related to the experience, causes, and consequences of homelessness (instruments available from authors). Average time for completion was 58 min in 1995 and 54 min in 2005.
MEASURES
The primary dependent variable, perceived unmet need for care (referred to as “unmet need for care” below), was based on an affirmative response to this question, “Since you’ve been without your own place, have there been times that you felt that you needed a doctor, but could not go to one?” The item is similar to the general perceived unmet need for care item in the Community Tracking Study,28 the National Health Interview Survey, and the National Survey of Homeless Assistance Providers and Clients.29 In other surveys, the item correlates with lack of health insurance, with emergency department use, and unmet need for care for specific symptoms.30,31
The primary independent variable, reflecting the study question of whether unmet need had changed over time, was year of survey (1995 versus 2005). A range of covariates associated with homeless persons’ service utilization in prior literature was included in the analysis,22,32–38 organized according to the Behavioral Model for Vulnerable Populations: 22
Predisposing Variables
The predisposing variables considered were: age, gender, race (Black versus non-Black), duration of being homeless (>180 days versus <180 days), unsheltered status in the prior 2 weeks, married/partnered status, high school graduate status, military service history, physical or sexual abuse in the past year, victimization by robbery (past 6 months), and jail/prison (ever).
Variables Enabling or Impeding Service Utilization
Prior research has shown that meeting basic needs impedes seeking health care.4 These competing priorities were based on a set of questions asking how often participants had problems finding or obtaining (1) a place to sleep, (2) clothes, (3) a place to clean up and use the toilet, and (4) enough food to eat. Our measure summed responses on a scale of 0–8, where each of the four problems was scored 0 = never, 1 = sometimes, and 2 = often. Additional measures included receipt of financial benefits, receipt of military benefits, main source of income in past month (benefits, paid work, other), health insurance status, and instrumental support from relatives or friends.39 The main source of income in the last 30 days was classed as Benefits (typically Social Security Insurance or Social Security Disability Insurance), Working/Employed, and Other/None (including no income and selling sex, drugs, personal possessions or panhandling).
Variables Reflecting Actual or Perceived Need for Services
Need variables included general self-reported health status (excellent, good, fair, poor), presence of any one of the three chronic conditions specifically queried in the survey (diabetes, hypertension, human immunodeficiency virus infection), and a 23-item index of physical symptoms used in prior homeless research39 (symptoms mapped to conditions in the National Health Interview Survey). We assessed lifetime history of mental illness diagnosis or treatment for mental illness. For substance use, we utilized self-report of at-risk drinking (>5 drinks for men and >4 drinks for women on any day in the last month),40 and recent (past month) illicit drug use.41
Analysis
We compared the percentage of participants with unmet need for care and predisposing, enabling, and need variables in the 1995 and 2005 surveys. Our main analytic objective was to assess whether a period effect, if present, was independent of participant characteristics. Using staged logistic regression analysis, we examined the dependent variable of unmet need for care, incorporating the independent variables of predisposing, enabling, and need characteristics in a series of three multivariable regression models. Year (2005 versus 1995) was retained in all models.
After adjustment for respondent characteristics, the year of survey was posited to represent a proxy for a period effect not related to measurable characteristics of the individuals surveyed and thus a possible indicator of safety net adequacy. Inferences from these statistical models were supplemented by descriptive analysis of selected survey questions. Specifically, persons reporting perceived unmet need for care were asked why they had been unable to obtain care and presented with a standardized list of potential barriers and an “other” response option (persons who denied unmet need were not asked this question). Reasons why care was not obtained were compared for the 1995 and 2005 samples. In addition, for persons who reported having received any outpatient health care, methods of payment for care were compared.
RESULTS
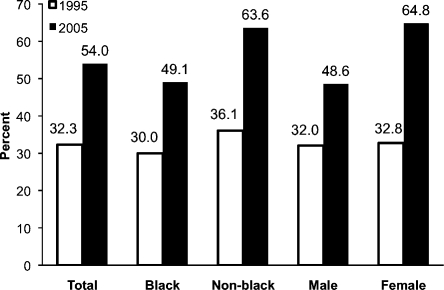
Figure 1 presents the percentages of respondents with unmet need for health care by race and gender for both years. Unmet need was more commonly reported in 2005 (54%) than in 1995 (32%) (p < 0.0001). The increase in unmet need was more pronounced for non-Blacks and females, among whom more than 60% perceived unmet need for care in 2005.
Figure 1.
Percentage of homeless persons in Birmingham unable to obtain care by demographic characteristics and year of survey (n = 161 for each survey).
Table 1 compares the 1995 and 2005 samples with respect to predisposing, enabling, and need characteristics. The 2005 sample was somewhat older and more likely to have been incarcerated and to have been homeless for over 6 months. Respondents in 2005 scored slightly higher on competing needs and were less likely to derive income from paid work. The 2005 sample was less likely to be accompanied by children or to have graduated high school. Regarding need variables, they reported slightly more physical symptoms, and more diagnoses of hypertension and HIV infection. They were more likely to report at-risk drug use and less likely to report at-risk alcohol use.
Table 1.
Comparison of Birmingham Homeless Survey Samples in 1995 and 2005
| Characteristic | 1995 | 2005 | p* |
|---|---|---|---|
| (n = 161) | (n = 161) | ||
| Predisposing variables | |||
| Age: mean (SD) | 37 (10) | 41 (10) | <0.001 |
| Non-Black race, % | 38 | 34 | 0.05 |
| Female, % | 36 | 34 | 0.64 |
| Graduated high school, % | 96 | 74 | <0.001 |
| Presently with children while homeless, % | 14 | 5 | 0.005 |
| Ever been to jail or prison, % | 61 | 78 | 0.001 |
| Homeless >180 days, % | 58 | 69 | 0.05 |
| Unsheltered in last 2 weeks, % | 28 | 30 | 0.71 |
| Married/partnered, % | 4 | 6 | 0.62† |
| History of military service, % | 33 | 21 | 0.01 |
| Physical or sexual abuse in past year, % | 14 | 16 | 0.53 |
| Victimization by robbery, past 6 months, % | 22 | 16 | 0.16 |
| Enabling/impeding variables | |||
| Competing needs, 0–8 scale: mean (SD) | 2.3 (2.4) | 2.4 (2.2) | <0.001 |
| Paid work in 7 days, % | 48 | 30 | <0.001 |
| Main source of income, prior month | 0.008 | ||
| Work, % | 42 | 27 | |
| Benefits, % | 26 | 26 | |
| None/other, % | 32 | 47 | |
| Currently receiving veterans’ benefits, % | 4 | 5 | 1.0† |
| Need variables | |||
| Physical symptom count of 23: mean (SD) | 4.7 (4.0) | 5.9 (4.6) | 0.02 |
| Hypertension, % | 27 | 40 | 0.02 |
| Diabetes, % | 9 | 9 | 0.85 |
| Human immunodeficiency virus infection, % | 0.6 | 8.1 | 0.001 |
| Mental illness diagnosed or treated, lifetime, % | 31% | 36% | 0.34 |
| Drinking caused a problem, ever in life, % | 55% | 55% | 0.92 |
| At-risk drinking in past month, % | 24% | 16% | 0.05 |
| Any illicit drug use, past month, % | 21% | 25% | 0.43 |
| Received drug abuse treatment, ever in life, % | 36% | 69% | <0.0001 |
*Statistical comparisons for the 2 years were t-tests and chi-Square tests
†Compared with Fisher’s exact test
After statistical adjustment for these differences, survey year (2005 vs. 1995) was strongly associated with greater likelihood of unmet health care need (OR 2.69; 95% CI, 1.49–4.83). Among enabling characteristics, more competing needs predicted unmet health-care need, while benefits income predicted lower odds of unmet need. Among need-related characteristics, mental illness predicted unmet need, while HIV infection predicted lower odds of unmet need. Across the staged models, the magnitude of association between year of 2005 and unmet need increased as potential confounders were added to the model (Table 2). Only a small number of participants were adults who were accompanied by their children (n = 23 in 1995; n = 8 in 2005). Accompaniment by children did not predict unmet need in either year (or across both years combined, all p > 0.20). Adding this variable to the statistical model did not alter the odds ratio for year 2005 versus 1995 (OR 2.79, 95% CI, 1.59–4.89).
Table 2.
Adjusted Odds Ratios (95% confidence intervals) for Predictors of Unmet Need for Care among Homeless Persons in Birmingham (Combining Samples from 1995 and 2005, n = 322)*†
| Model 1 | p‡ | Model 2 | p‡ | Model 3 | p‡ | |
|---|---|---|---|---|---|---|
| Predisposing characteristics | Predisposing and Enabling/Impeding characteristics | Predisposing, Enabling/Impeding and Need characteristics | ||||
| Year (2005 vs 1995) | 2.18 (1.32–3.60) | 0.002 | 2.38 (1.39–4.06) | 0.002 | 2.68 (1.49–4.83) | 0.001 |
| Predisposing characteristics | ||||||
| Age (+1 year) | 0.99 (0.78–1.26) | 0.95 | 1.15 (0.89–1.50) | 0.28 | 1.15 (0.86–1.53) | 0.35 |
| Non-Black race | 1.49 (0.93–2.41) | 0.10 | 1.41 (0.85–2.34) | 0.18 | 1.36 (0.77–2.38) | 0.29 |
| Female | 1.52 (0.92–2.51) | 0.11 | 1.54 (0.90–2.64) | 0.11 | 1.29 (0.70–2.38) | 0.42 |
| Ever in jail or prison | 1.33 (0.78–2.26) | 0.29 | 0.84 (0.47–1.52) | 0.57 | 0.71 (0.37–1.35) | 0.29 |
| Homeless >180 days | 1.56 (0.96–2.56) | 0.08 | 1.27 (0.75–2.14) | 0.38 | 1.02 (0.57–1.81) | 0.95 |
| High school graduate | 0.67 (0.34–1.32) | 0.24 | 0.76 (0.37–1.55) | 0.44 | 0.84 (0.38–1.82) | 0.65 |
| Enabling characteristics | ||||||
| Competing needs (+1, 0–8 scale) | – | 1.29 (1.15–1.45) | <0.001 | 1.26 (1.12–1.43) | <0.001 | |
| Health insurance | – | |||||
| Income | 0.02 | 0.002 | ||||
| Paid work | – | 0.80 (0.45–1.44) | 0.93 (0.49–1.74) | |||
| Benefits | – | 0.39 (0.20–0.76) | 0.26 (0.12-.57) | |||
| None or only nonwork/non-benefit (panhandling) | – | 1 (Reference) | 1 (Reference) | |||
| Need characteristics | ||||||
| Symptom score (+1 symptom) | – | – | 1.14 (1.06–1.22) | <0.001 | ||
| Hypertension or diabetes | – | – | 1.25 (0.71–2.22) | 0.44 | ||
| HIV | – | – | 0.21 (0.05–0.89) | 0.03 | ||
| Mental illness | – | – | 2.04 (1.05–3.97) | 0.03 | ||
| Heavy drinking, last month | – | – | 1.91 (0.92–3.97) | 0.08 | ||
| Illicit drug use, last month | – | – | 0.92 (0.46–1.85) | 0.81 | ||
*The outcome Unmet Need for Care is defined as an affirmative response to the question, Since you’ve been without your own place, have there been times that you felt you needed a doctor, but could not go to one?
†Three multivariable logistic regression models are shown, with all adjusted variables for each model shown in a single column. All 322 participants were included in all models, except the final one, where 2 were excluded due to missing data
‡Results in bold are statistically significant at the p = 0.05 level, two-tailed
Table 3 shows the reasons why care was not obtained in the subset reporting unmet need. In both years, cost and transportation problems were commonly cited. From 1995 to 2005, the percentage citing lack of money or insurance rose from 42% to 67% (p < 0.001). The percentage reporting transportation problems rose from 19% to 41% (p < 0.001). The attribution of disliking doctors dropped from 19% (1995) to 7% (2005, p = 0.03).
Table 3.
Reasons Care was not Obtained among Persons Reporting Unmet Need for Care (n = 139)*
| Reasons endorsed | 1995 | 2005 | p† |
|---|---|---|---|
| Did not know where to go, % | 12 | 10 | 0.83 |
| Could not afford doctor due to lack of money or insurance, % | 42 | 67 | 0.01 |
| Problem was not serious enough, % | 13 | 7 | 0.23 |
| Lacked transportation, % | 19 | 41 | 0.01 |
| Too busy to go, % | 6 | 8 | 0.74 |
| Could not get off work, % | 4 | 3 | 1.0 |
| Too sick to go, % | 6 | 10 | 0.53 |
| Too much trouble to wait at hospital, % | 10 | 10 | 0.89 |
| Don’t have service card for the hospital, % | 10 | 16 | 0.28 |
| Don’t like doctors or hospitals, % | 19 | 7 | 0.03 |
*Participants who reported an unmet need for health care (n = 52 in 1995; n = 87 in 2005) were asked to endorse items from a standard list of reasons that they “did not go to a doctor.” They were permitted to endorse more than one reason
†The p-value reflects a chi-squared test comparing the percentage endorsing each reason in 1995 versus 2005
Additional survey data suggested care was more tightly linked to ability to pay in 2005 than in 1995. Among persons who reporting any outpatient health care at least once since becoming homeless (other than inpatient hospitalization), reports of care “for free” declined (from 48% in 1995 to 20% in 2005, p < 0.0001), while rising numbers reported relying on out-of-pocket payment, assistance from family, or sources other than insurance (from 20% to 51%, p < 0.0001). There was no increase in the percentages reporting private insurance, Medicare, or Medicaid.
Perceived unmet need for care carried different implications for hospitalization across the two survey years. In 1995, the percentage of individuals hospitalized since becoming homeless was similar among persons reporting (25%) and not reporting (32%) unmet need (p = 0.36). In 2005, inpatient hospitalization was more common among persons who perceived an unmet need for health care (45% versus 26%, p = 0.01).
DISCUSSION
Our findings suggest a large rise in the percentage of Birmingham’s homeless perceiving an unmet need for medical care from 1995 to 2005, from 32% to 54%. Among Americans in the general population, the percentage reporting unmet need for medical care fell from 6% in the 199428 to 5.2% in 2003.8 The percentage of Birmingham’s homeless with unmet need in 1995 is higher than the 24.6% of homeless persons reporting unmet need in a national survey in 1996 (n = 2,974).3 No subsequent national survey of homeless Americans’ health care access has been conducted. In the Birmingham sample, unmet need was somewhat more common among women and persons characterized as non-Black, a finding not explained by this analysis.
Several characteristics associated with unmet need were more prevalent in 2005 (and are relevant in other research3,22,32,35–37,42). These included older age, higher competing priority scores, higher physical symptom count, and greater proportions with some chronic diseases. Controlling for these characteristics, there remained an independent association between a survey year of 2005 and perceived unmet need for health care. In fact, the magnitude of association increased as potential confounders were entered into the model. This pattern suggests an independent effect of year (i.e., a period effect) and may bear on consideration of Birmingham’s health-care safety net, which we address below.
The present findings are likely relevant to the health of homeless persons in Birmingham. Research documents high medical morbidity among homeless persons43 and elevated mortality.5,6,44–46 Ambulatory care access is associated with decreased hospitalization for preventable conditions47 and decreased nonurgent emergency department use.48 Use of Health Care for the Homeless programs is associated with reduced emergency department use,49 suggesting that timely outpatient care might have averted some hospital visits. The association between unmet need and inpatient hospitalization, apparent in 2005, may indicate cause and effect.
Explaining the rise in perceived unmet need is a matter of informed speculation. Table 4 provides socioeconomic indicators for the Birmingham area for 1995 and 2005. No large-scale socioeconomic change is evident, except for a rising Latino/Hispanic population, but this group remains a small percentage of the population.
Table 4.
Selected Statistics for Birmingham, Alabama, and Surrounding Area, 1995 and 20051,2
| 1995 | 2005 | |
|---|---|---|
| Population, Jefferson County (total) | 663,092 | 662,754 |
| % White | 63% | 57% |
| % Black | 36% | 41% |
| % Other | 0.7% | 1% |
| Hispanic population, Jefferson County | 3,341 | 15,634 |
| Primary industries | Banking, health care, health research | Banking, health care, health research |
| Unemployment, annual, Jefferson County | 3.8% | 3.8% |
| Poverty % (and number), Jefferson County | 16% (n = 105,779) | 15.7% (n = 100,709) |
| Median household income, Jefferson County (2005 dollars) | $41,761 | $41,821 |
| High school dropout (% in 1 year), Jefferson County | 6% | 5% |
| Violent crime, events per 100,000, Birmingham City | 2,456.0 | 1,470.3 |
| Violent crime rate per 100,000 population, Jefferson County | 583.6 | 308.6 |
| Without health insurance % (and number), Alabama3 | 13.5% (n = 595,000) | 14.5% (n = 657,000) |
| Diabetes, % (and number), Alabama | 5.3% (n = 161,000) | 8.9% (n = 318,000) |
| Diabetes, told by doctor, % | 4.8% | 9.8% |
| Overweight or 0bese (BMI >25) | 54.1% | 64.5% |
1. Birmingham sits in Jefferson County, the largest of seven counties in the Birmingham-Hoover Metropolitan Statistical Area (MSA)
2. Data are from the US Census Bureau, US Bureau of Economic Analysis, the Alabama State Department of Education (2005), the website http://www.kidscount.org (Annie E. Casey Foundation), US Bureau of Labor Statistics, the US Bureau of Justice Statistics and FBI Uniform Crime Reports, and Centers for Disease Control Behavorial Risk Factor Surveillance System
3. Comparable estimates of uninsurance at the substate level for 1995 and 2005 are not available. Comparison of 1995 to 2005 is subject to error due to changes in Bureau of Census methods of estimation
Since Birmingham’s count of homeless persons increased only modestly from 2,629 to 2,929 (11%), it is difficult to attribute rising unmet need to competition for services among homeless persons, especially since the number of safety net providers (a county hospital, a federally qualified community health center, a veterans’ hospital, some county primary care clinics) increased slightly with a voluntary faith-based clinic. Neither the geographic distribution of the homeless nor the availability of public transportation resources changed substantially over the 10-year period.
The survey data do show that homeless persons were more likely to cite monetary barriers and less likely to report free care in 2005 than in 1995. Such financial constraints raise concerns about the safety net. A convincing analysis of any community’s health-care safety net requires income, cost, and service delivery data from several organizations; however, these data are difficult to acquire. Some funding streams increased. County allocations for the county hospital’s indigent care rose from $30 million in 1995 to $46 million (nominal dollars) in 2005 (an 11% rise after inflation adjustment). Conversely, Medicaid-associated Disproportionate Share Hospital payments fell by a lesser amount from $8.9 million to $6.1 million (a 53% decline, inflation-adjusted). A rise in funding was noted for the community health center, established as a Health Care for the Homeless (HCH) Program in 1987, where support from the Health Resources and Services Administration (HRSA) rose from $930,930 in 1997 to $2.7 million in 2005 (a 113% increase, adjusting for inflation). However, new awards were not specifically for homeless health care as the program expanded its mission to treat poor persons with homes.
Even if funding streams increased to some safety net entities, their capacity may have been strained if their business costs rose, if collections declined, or if nonsafety net providers reduced their exposure to nonpaying patients, resulting in greater aggregate demand for safety net services from persons who were not homeless. Under such conditions, noted nationally,10,11,50 safety net providers may adjust or relocate services to enhance revenues, limiting their exposure to the poor .51 The recent closure of a community hospital in a poorer section of Birmingham suggests such pressures may be present.
Anecdotal reports received by the investigators, who worked with homeless organizations during the study period, indicated rising procedural barriers to access at some safety net providers. These included more stringent requirements for referral and identification documents, rising copayments, and more detailed financial eligibility evaluations. One institution reversed some changes in 2007.
Limitations
Limitations of this study include inability to identify specific types of care that may have been difficult to obtain. Also, the findings may underestimate unmet need; reports of unmet need rise when specific needs are queried individually.28 Unmeasured changes in population characteristics might account for our findings, but many variables from homeless health services research were included,19,22,34,52,53 and the statistical impact of year 2005 increased as these variables were included. Finally, Hispanic status, assessed only in 2005, was not analyzed; restricting the 2005 sample to non-Hispanics results in 49% with unmet need (versus 54% overall), making it unlikely that this can explain the findings.
Strengths include consistent methodology across two surveys, permitting a credible portrait of change over time. No similar national comparative study exists. A broad range of variables was included, lending credibility to the notion that the statistical impact of year is independent of participant characteristics.
In sum, the rising percentage of homeless persons reporting inability to obtain health care when needed in Birmingham raises questions about the adequacy of its health care safety net. Given concerns about safety net institutions nationally,11,54 homeless persons in other communities may be similarly affected.
Acknowledgements
The authors wish to express their appreciation to Mina Madani and Sheila Samples for their help in reconciling databases, and to Young-il Kim for statistical programming.
Support The original data collection was funded by grants from the Office of Development, City of Birmingham, AL, and the Office of Planning and Community Development of Jefferson County, AL. Dr Kertesz’s effort was supported by a Research Career Development Award from the National Institute on Drug Abuse (K23-DA-015487).
Conflict of Interest The lead author has, or has had in the last 5 years, formal associations including employment or membership on the staff at four nonprofit safety net providers referenced in the manuscript, including a county hospital, a Veterans Administration hospital, and a federally qualified community health center, and an academic teaching hospital. The lead author has provided informal advice to one other referenced safety net provider, a faith-based volunteer clinic. No other author of the manuscript has a potential conflict of interest.
Footnotes
An abstract of these findings was presented at the 2008 Annual Meeting of the Society of General Internal Medicine.
Support: The original data collection was funded by grants from the Office of Development, City of Birmingham, AL, and the Office of Planning and Community Development of Jefferson County, AL. Dr Kertesz’s effort was supported by a Research Career Development Award from the National Institute on Drug Abuse (K23-DA-015487).
References
- 1.Committee on the Health Care of Homeless People. Homelessness, Health, and Human Needs. Washington, D.C.: Institute of Medicine; 1988.
- 2.Brickner PW, Scharer LK, Conanan BA, Savarese M, Scanlan BC. Under the safety net: The Health and Social Welfare of the Homeless in the United States. New York, NY: W.W. Norton & Co.; 1990. [Google Scholar]
- 3.Kushel MB, Vittingoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 4.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87:217–2120. doi: 10.2105/AJPH.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283:2152–2157. doi: 10.1001/jama.283.16.2152. [DOI] [PubMed] [Google Scholar]
- 6.Hwang SW, Orav EJ, O’Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997;126:625–628. doi: 10.7326/0003-4819-126-8-199704150-00007. [DOI] [PubMed] [Google Scholar]
- 7.Salit SA, Kuhn EM, Hartz AJ, Vu JM, Mosso AL. Hospitalization costs associated with homelessness in New York City. N Engl J Med. 1998;338:1734–1740. doi: 10.1056/NEJM199806113382406. [DOI] [PubMed] [Google Scholar]
- 8.Strunk BS, Cunningham PJ. Trends in Americans’ Access to Needed Medical Care, 2001–2003. Washington, DC: Center for Studying Health System Change; 2004. [Google Scholar]
- 9.America’s Health Care Safety Net: Intact but Endangered. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 10.Hoffman C, Sered SS. Threadbare: Holes in America’s Health Care Safety Net. Menlo Park: The Henry A. Kaiser Family Foundation; 2005. [Google Scholar]
- 11.Hadley J, Cravens M, Coughlin T, Holahan J. Federal Spending on the Health Care Safety Net from 2001–2004: Has Spending Kept Pace with the Growth in the Uninsured? Washington, DC: Kaiser Family Foundation; 2005. [Google Scholar]
- 12.Fishman LE, Bentley JD. The evolution of support for safety-net hospitals. Health Aff (Millwood) 1997;16:30–47. doi: 10.1377/hlthaff.16.4.30. [DOI] [PubMed] [Google Scholar]
- 13.Holahan J, Cook A. The U.S. economy and changes in health insurance coverage, 2000–2006. Health Aff (Millwood) 2008;27:w135–144. doi: 10.1377/hlthaff.27.2.w135. [DOI] [PubMed] [Google Scholar]
- 14.Coughlin TA, Zuckerman S, McFeeters J. Restoring fiscal integrity to Medicaid financing? Health Aff (Millwood) 2007;26:1469–1480. doi: 10.1377/hlthaff.26.5.1469. [DOI] [PubMed] [Google Scholar]
- 15.United States Congress. Deficit Reduction Act of 2005. Available at: http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=109_cong_bills&docid = f:s1932enr.txt.pdf. Accessed 3/29/09
- 16.Deficit Reduction Act of 2005: Implications for Medicaid. Washington, DC: Kaiser Family Foundation; 2005. [Google Scholar]
- 17.Duke EM. Remarks to the 33rd Annual Convention of the National Association of Community Health Centers. Washington, DC: United States Department of Health and Human Services Health Resources and Services Administration; September 17, 2002. Available at: http://archive.hrsa.gov/newsroom/releases/2002speeches/nachc-sept.htm. Accessed 3/29/09.
- 18.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- 19.Wenzel SL, Bakhtiar L, Caskey NH, et al. Homeless veterans’ utilization of medical, psychiatric, and substance abuse services. Med Care. 1995;33:1132–1144. doi: 10.1097/00005650-199511000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Koegel P, Sullivan G, Burnam A, Morton SC, Wenzel S. Utilization of mental health and substance abuse services among homeless adults in Los Angeles. Med Care. 1999;37:306–317. doi: 10.1097/00005650-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally ill homeless veterans. Med Care. 2003;41:275–287. doi: 10.1097/00005650-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 23.LaGory M, Ritchey FJ, Gerald L. Homelessness in Birmingham and Jefferson County: A Needs Assessment. Birmingham, AL: Office of Community Development of the City of Birmingham, and the Office of Planning and Community Development of Jefferson County; 1995. [Google Scholar]
- 24.Ritchey FJ, Lagory ME, Fitzpatrick KM, Hale T, Irwin J. Report of Results of the Birmingham, Alabama Metropolitan Area Survey of Homeless Persons, January 27–28, 2005. Birmingham: University of Alabama at Birmingham; 2005. [Google Scholar]
- 25.Rossi PH, Wright JD, Fisher GA, Willis G. The urban homeless: estimating composition and size. Science. 1987;235:1336–1341. doi: 10.1126/science.2950592. [DOI] [PubMed] [Google Scholar]
- 26.United States Congress. McKinney Homeless Assistance Act. Pub L No. 100–77; 1987.
- 27.LaGory M, Ritchey FJ, Fitzpatrick K, Irwin J. A Needs Assessment of the Homeless of Birmingham and Jefferson County. Birmingham: University of Alabama at Birmingham; 2005. [Google Scholar]
- 28.Berk ML, Schur CL, Cantor JC. Ability to obtain health care: recent estimates from the Robert Wood Johnson Foundation National Access to Care Survey. Health Aff (Millwood) 1995;14:139–146. doi: 10.1377/hlthaff.14.3.139. [DOI] [PubMed] [Google Scholar]
- 29.Burt MR, Aron LY, Douglas T, Valente J, Lee E, Iwen B. Homelessness: Programs and the People They Serve. Technical Report of Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC: Urban Institute; 1999. [Google Scholar]
- 30.Cunningham PJ, Hadley J. Differences between symptom-specific and general survey questions of unmet need in measuring insurance and racial/ethnic disparities in access to care. Med Care. 2007;45:842–850. doi: 10.1097/MLR.0b013e318053678f. [DOI] [PubMed] [Google Scholar]
- 31.Long SK, King J, Coughlin TA. The implications of unmet need for future health care use: findings for a sample of disabled Medicaid beneficiaries in New York. Inquiry. 2005;42:413–420. doi: 10.5034/inquiryjrnl_42.4.413. [DOI] [PubMed] [Google Scholar]
- 32.Robertson MJ, Cousineau MR. Health status and access to health services among the urban homeless. Am J Public Health. 1986;76:561–563. doi: 10.2105/AJPH.76.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92:778–784. doi: 10.2105/AJPH.92.5.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim TW, Kertesz SG, Horton NJ, Tibbetts N, Samet JH. Episodic homelessness and health care utilization in a prospective cohort of HIV-infected persons with alcohol problems. BMC Health Serv Res. 2006;6:19. doi: 10.1186/1472-6963-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kertesz SG, Larson MJ, Cheng DM, et al. Need and non-need factors associated with addiction treatment utilization in a cohort of homeless and housed urban poor. Med Care. 2006;44:225–233. doi: 10.1097/01.mlr.0000199649.19464.8f. [DOI] [PubMed] [Google Scholar]
- 36.Desai MM, Rosenheck RA, Kasprow WJ. Determinants of receipt of ambulatory medical care in a national sample of mentally Ill homeless veterans. Med Care. 2003;41:275–287. doi: 10.1097/00005650-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Bird CE, Jinnett KJ, Burnam MA, et al. Predictors of contact with public service sectors among homeless adults with and without alcohol and other drug disorders. J Stud Alcohol. 2002;63:716–725. doi: 10.15288/jsa.2002.63.716. [DOI] [PubMed] [Google Scholar]
- 38.Wenzel SL, Audrey Burnam M, Koegel P, et al. Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Med Care. 2001;39:1158–1169. doi: 10.1097/00005650-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 39.LaGory M, Ritchey F, Fitzpatrick K. Homelessness and affiliation. Sociol Q. 1991;32:201–218. doi: 10.1111/j.1533-8525.1991.tb00353.x. [DOI] [Google Scholar]
- 40.Helping Patients Who Drink Too Much: A Clinician’s Guide. Rockville, MD: National Institutes of Health; 2005. [Google Scholar]
- 41.Kertesz SG, Pletcher MJ, Safford M, et al. Illicit drug use in young adults and subsequent decline in general health: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Drug Alcohol Depend. 2007;88:224–233. doi: 10.1016/j.drugalcdep.2006.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim TW, Alford DP, Malabanan A, Holick MF, Samet JH. Low bone density in patients receiving methadone maintenance treatment. Drug Alcohol Depend. 2006;85:258–262. doi: 10.1016/j.drugalcdep.2006.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gelberg L, Linn LS. Social and physical health of homeless adults previously treated for mental health problems. Hospital & Community Psychiatry. 1988;39:510–516. doi: 10.1176/ps.39.5.510. [DOI] [PubMed] [Google Scholar]
- 44.O’Connell JJ. Dying in the shadows: the challenge of providing health care for homeless people. Can Med Assoc J. 2004;170:1251–1252. doi: 10.1503/cmaj.1040008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hibbs JR, Benner L, Klugman L, et al. Mortality in a cohort of homeless adults in Philadelphia. N Engl J Med. 1994;331:304–309. doi: 10.1056/NEJM199408043310506. [DOI] [PubMed] [Google Scholar]
- 46.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. Can Med Assoc J. 2004;170:1243–1247. doi: 10.1503/cmaj.1031167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. doi: 10.1001/jama.274.4.305. [DOI] [PubMed] [Google Scholar]
- 48.Petersen LA, Burstin HR, O’Neil AC, Orav EJ, Brennan TA. Nonurgent emergency department visits: the effect of having a regular doctor. Med Care. 1998;36:1249–1255. doi: 10.1097/00005650-199808000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by Homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9:530–537. doi: 10.1097/00124784-200311000-00014. [DOI] [PubMed] [Google Scholar]
- 50.Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An update on safety-net hospitals: coping with the late 1990s and early 2000s. Health Aff (Millwood) 2005;24:1047–1056. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 51.Lipson DJ, Naierman N. Effects of health system changes on safety-net providers. Health Aff (Millwood) 1996;15:33–48. doi: 10.1377/hlthaff.15.2.33. [DOI] [PubMed] [Google Scholar]
- 52.Desai MM, Rosenheck RA. Unmet need for medical care among homeless adults with serious mental illness. Gen Hosp Psych. 2005;27:418–425. doi: 10.1016/j.genhosppsych.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 53.Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28:805–821. doi: 10.1097/00005650-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 54.Cunningham PJ, Bazzoli GJ, Katz A. Caught in the competitive crossfire: safety-net providers balance margin and mission in a profit-driven health care market. Health Aff (Millwood) 2008;27:w374–382. doi: 10.1377/hlthaff.27.5.w374. [DOI] [PubMed] [Google Scholar]