Abstract
The skin lesion of herpes zoster is classically limited to a single dermatome, and most cases of multi-dermatomal herpes zoster have contiguous skin lesions. Noncontigous multi-dermatomal herpes zoster is very rare in both immunocompetent and immunosuppressed persons. The phenomenon of zoster occurring in two non-contiguous dermatomes has been referred to as zoster duplex unilateralis or bilateralis. We report here on a case of herpes zoster duplex bilateralis in a 49-year-old woman who had previously received chemotherapy for breast cancer treatment.
Keywords: Herpes zoster, Breast neoplasms
Introduction
Herpes zoster is a relatively common disease and it is characterized by several groups of painful vesicles with a characteristic distribution on unilateral dermatomes (1). Cases of bilateral involvement are rare, and moreover, synchronous zosters involving two widely separated regions are even rarer (2). The phenomenon of zoster occurring on two non-contiguous, widely separated dermatomes has been referred to as zoster duplex unilateralis or bilateralis, depending on whether one half or both halves of the body are involved (3). Herein, we report on a case of herpes zoster duplex bilateralis that occurred in an immunosuppressed patient who had previously received chemotherapy for breast cancer treatment.
Case Report
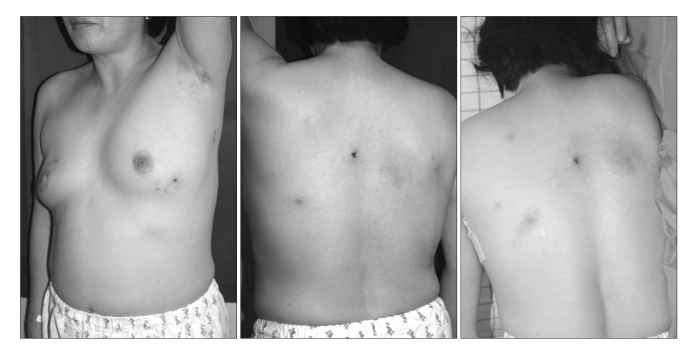
A 49-year-old female visited the authors' hospital for an evaluation of the painful grouped erythematous vesicles on her left anterior chest and upper back, and this had developed about five days earlier and then rapidly spread. The lesions showed a band-like arrangement, and they were noted in the right T4 and left T4 non-contiguous dermatomes (Fig. 1). The associated features of her current illness included difficulty sleeping at night because of the painful rash and a feeling of lethargy during the day.
Fig. 1.
The grouped erythematous vesicles on the left anterior chest (Lt. T4) and both upper back areas (Rt. T4).
She was diagnosed with right breast cancer (Stage II) four years previously and was treated at that time with breast excision and lymphnode dissection followed by six cycles of chemotherapy. Her chemotherapy regimen included 5-fluorouracil, methotrexate and adriamycin. She had recently visited the Department of General Surgery for a follow-up evaluation for the breast cancer. There was no sign of recurrence or metastasis.
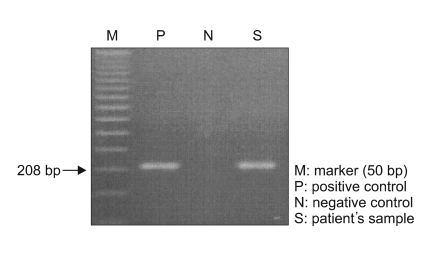
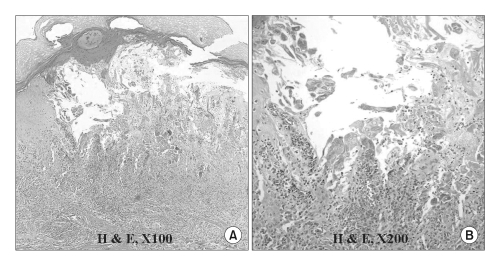
The results of her complete blood count, serum chemistry, urinalysis and VDRL and chest PA tests were normal except for a decreased level of helper/inducer T-cells (CD4, 643/mm3) and suppressor/cytotoxic T-cells (CD8: 552/mm3). The Tzanck smear on her left anterior chest showed multinucleated giant cells with intranuclear inclusion bodies. Histologic examination of the vesicle lesions on her left anterior chest and upper back displayed intraepidermal blisters with ballooning degeneration, reticular degeneration, characteristic intranuclear inclusion bodies and acantholytic multinucleated giant cells (Fig. 2). For further evaluation and diagnostic confirmation, polymerase chain reaction (PCR) was performed for the varicella-zoster virus, and this consisted of a positive band of 208 bp (Fig. 3).
Fig. 3.
PCR (Polymerase chain reaction) for varicella-zoster virus showing a positive band of 208 bp.
Under the impression that herpes zoster duplex bilateralis had occurred in a breast cancer patient who had previously received chemotherapy and she had not suffered tumor recurrence, she was treated with oral administration of famciclovir 750 mg/day for seven days, and the skin lesions and pain subsided without complications.
Discussion
Herpes zoster is caused by the varicella zoster virus. Following a patient's natural infection or immunization, the virus remains latent in his/her sensory dorsal root ganglion cells and it replicates later, traveling down the sensory nerve into the skin (1). The clinical manifestations are characterized by several groups of painful vesicles situated unilaterally within the distribution of the cranial or spinal sensory nerve. Bilateral involvement and recurrence are rare, and zosters involving two widely separated regions at one time are even rarer (2). The phenomenon of zoster occurring in two non-contiguous, widely separated dermatomes has been referred to as zoster duplex unilateralis or bilateralis, depending on whether one half or both halves of the body are involved (3). The incidence of herpes zoster duplex bilateralis is below 0.5% (4). In a review of the medical English literature over the last three decades, only seven cases have been reported, two in immunocompetent persons, three in older persons on oral steroids for treating chronic illnesses and two in children with cancer (one with lymphoma and the other with leukemia) (4). Yet there is no previously reported case that occurred in an immunosuppressed patient who had previously received chemotherapy for breast cancer, as in the current case.
Patients with malignancy, and especially patients with Hodgkin's disease and leukemia, are five times more likely to develop zoster than others of the same age (5). The other patients who have a higher incidence of zoster include those with deficient immune systems, such as the individuals who are immunosuppressed for organ transplantation, the individuals with connective tissue disease and those who take agents such as corticosteroids (6). The patient reported on in this paper had a history of breast cancer and she had been previously treated with chemotherapy that included 5-fluorouracil, methotrexate and adriamycinskin. We can speculate that she was under an immunosuppressed state because of her previous chemotherapy and not because of tumor recurrence, and the previous chemotherapy led to her defective cellular immune response and the development of zoster duplex bilateralis.
The clinical appearance of these patients is usually identical to that of typical zoster, but the lesions may be more ulcerative and necrotic and they may scar more severely (7). Our patient, however, revealed typical zoster lesions and she healed without complications such as scars and pain.
This is the first case reported in the English medical literature in which herpes zoster duplex bilateralis occurred in an immunosuppressed patient who had previously received chemotherapy for breast cancer treatment. Our case illustrates that herpes zoster can present with bilateral involvement, which is referred to as zoster duplex bilateralis, in an immunosuppressed patient.
Fig. 2.
Intraepidermal blisters with ballooning degeneration, reticular degeneration, characteristic intranuclear inclusion bodies and acantholytic multinucleated giant cells (H&E, A:×100, B:×200).
References
- 1.Straus SE, Schmader KE, Oxman MN. Varicella and herpes zoster. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Dermatology in general medicine. 6th ed. New York: McGrow-Hill; 2003. pp. 2070–2085. [Google Scholar]
- 2.Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic complications of the reactivation of varicella-zoster virus. N Engl J Med. 2000;342:635–645. doi: 10.1056/NEJM200003023420906. [DOI] [PubMed] [Google Scholar]
- 3.Odom RB, James WD, Berger TG. Andrews' diseases of the skin. 9th ed. Philadelphia: W.B. Saunders Co.; 2000. Viral diseases; pp. 486–491. [Google Scholar]
- 4.Vu AQ, Radonich MA, Heald PW. Herpes zoster in seven disparate dermatomes (zoster multiplex): Report of a case and review of the literature. J Am Acad Dermatol. 1999;40:868–869. doi: 10.1053/jd.1999.v40.a96944. [DOI] [PubMed] [Google Scholar]
- 5.Arvin AM. Varicella-zoster virus. Clin Microbiol Rev. 1996;9:361–381. doi: 10.1128/cmr.9.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Takayama N, Yamada H, Kaku H, Minamitami M. Herpes zoster in immunocompetent and immunocompromised Japanese children. Pediatr Int. 2000;42:275–279. doi: 10.1046/j.1442-200x.2000.01227.x. [DOI] [PubMed] [Google Scholar]
- 7.Peretz A, Nowatzky J, Steiner I. Neurological picture: Herpes zoster duplex bilateralis. J Neurol Neurosurg Psychiatry. 2007;78:818. doi: 10.1136/jnnp.2006.114116. [DOI] [PMC free article] [PubMed] [Google Scholar]