Abstract
Background: The present status of outpatient treatment of depression in Germany was evaluated with respect to the adherence of general practitioners (GPs) and specialists of psychiatry to clinical practice guidelines.
Methods: In total, 488 depressed patients' psychopathology, diagnostic assessment, therapeutic measures and referral frequency were documented at inclusion into study by 43 general practitioners and 23 specialists of psychiatry in three regions of Germany. The investigation of change in depressive symptoms after six to eight weeks by means of self-assessment could be evaluated for 165 patients.
Results: The results of diagnostic assessment demonstrated that diagnoses of depression were not always based on the diagnostic criteria for depression (ICD-10): 33% of GPs' and 17% of specialists' patients were included as depressed patients into the study despite not fulfilling the ICD-10 criteria in the standardized documentation. Therapeutic undertreatment was more often found in the group of GPs. Referrals were found not to be oriented towards guidelines. After six to eight weeks, one half of patients reported a reduction in depressed symptoms, the other half of patients reported a stagnation or even a progression.
Conclusions: The study has shown that physicians in outpatient settings still fail to orient themselves towards guideline recommendations. This reflects the need for physicians to receive guideline training, with the aim of improving the quality of care for depression. A quality management intervention program consisting of guideline training and an interdisciplinary quality circle to improve depression treatment and networking was supported by the authors and is currently being evaluated.
Abstract
Hintergrund: Der aktuelle Status der ambulanten Depressionsversorgung in Deutschland wurde erhoben.
Methode: Insgesamt wurden bei 488 depressiven Patienten Psychopathologie, diagnostische und therapeutische Maßnahmen sowie das Überweisungsverhalten zum Zeitpunkt des Studieneinschlusses von 43 Haus- und 23 Fachärzten für Psychiatrie in drei Studienregionen Deutschlands dokumentiert. Die Veränderung der depressiven Symptomatik nach sechs bis acht Wochen im Rahmen einer Selbstbeurteilung konnte bei 165 Patienten erfasst werden.
Ergebnisse: Die Ergebnisse der diagnostischen Maßnahmen zeigten, dass die individuelle Diagnosestellung nicht immer auf den diagnostischen Kriterien einer Depression (ICD-10) basierte: 33% der Hausarzt- und 17% der Facharzt-Patienten wurden als depressive Patienten in die Studie eingeschlossen, obwohl sie die ICD-10 Kriterien laut der standardisierten Dokumentation nicht erfüllten. Eine ungenügende therapeutische Versorgung wurde häufiger bei den Hausärzten gefunden. Das Überweisungsverhalten orientierte sich nicht immer an verfügbaren, aktuellen Leitlinien. Nach sechs bis acht Wochen berichtete die Hälfte der Patienten eine Symptomverbesserung, während die andere Hälfte keine Veränderung oder sogar eine Verschlechterung angab.
Diskussion: Die Studie hat gezeigt, dass die Leitlinienorientierung im ambulanten Versorgungssegment optimierbar erscheint. Dies verdeutlicht einen hohen Bedarf an ärztlichen Leitlinienschulungen, um die Qualität in der ambulanten Depressionsbehandlung zu verbessern. Derzeit wird von den Autoren eine durchgeführte Qualitätsmanagement-Intervention aus Leitlinienschulung und interdisziplinären Qualitätszirkeln zur Verbesserung der Depressionsversorgung und Vernetzung evaluiert.
Introduction
Patients with a depressive disorder are treated in outpatient settings by general practitioners (GPs) or by specialists for psychiatry. GPs play a key role as they are often the first health care providers for the recognition, diagnosis, referral, and treatment of depression. Depression is rather common in primary care: it is estimated to effect about 10% of all primary care attendees [1], [2], [3]. Recent studies in Germany have shown that 11.5% of the adult population suffer from affective disorders, 8.3% of the population have experienced major depression during the past 12 months, and that every fourth patient in general practice fulfills the criteria for depression [4].
According to recent data of the U.S.A. and Canada [5], [6], [7], the German study of Wittchen and colleagues revealed that only one half of depressed patients have ever contacted a health care institution, and only one third of these patients have ever received intervention [8]. Another problem relates to delayed referrals to specialists or psychiatric hospitals [9], [10]. Reasons for this situation in primary care are various, and a range of patient, doctor and organizational factors contribute to this problem [11], [12], [13], [14].
In addition to GPs, specialists such as psychiatrists, psychotherapists or neuropsychiatrists have an important function in outpatient care. Depressive disorders are the most significant and frequent illnesses treated by these specialists [15]. However, there is empirical evidence of underdiagnosis and undertreatment, even by psychiatrists [16].
The fact that guideline-oriented treatment leads to distinct improvement in the treatment of depression was established in international studies [17]. Unfortunately, such guidelines [18], [19], [20] are still underused in practice. The adherence to a multi-level care model between general practitioners and specialists also brings about evident improvement in the treatment of depression [8], [21]. Moreover, the efficacy of specific quality management programs in reducing deficits in diagnostic and treatment of depression has been shown [21], [22].
Initial aims of the project are to explore the present status of outpatient treatment of depression in Germany. Further aims are to analyze the diagnostic assessment, treatment and referral behavior of GPs and specialists in respect to guideline adherence. Comparing current outpatient treatment of depression and the required guideline-oriented depression treatment should identify opportunities for improvement. The study should ascertain the requirement in guidelines education and in cooperation for GPs and specialists.
Methods
Design
The study was performed within the German Research Network on Depression [23]. At the start of the study in 2001, a total of over 400 physicians (GPs and specialists) were contacted by letter in three regions (Rhineland, South Baden and Bavaria). Of those contacted, 75 physicians expressed interest and received the study questionnaires and documentation tools. Ultimately, 66 participated in the study and began the recruitment and documentation in their practice from October 2001 until March 2002. The physicians had to include each patient suffering from depressed symptoms in the study on the basis of the practitioner's subjective assessment until ten patients were recruited. Furthermore, the following conditions had to be fulfilled: the presence of a newly identified depressive disorder or a new onset of a depressive episode, minimum age of 18 years and competence in the German language.
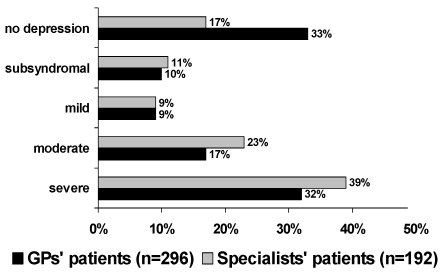
In total, the treatment of 488 patients was documented by 43 GPs and 23 specialists. The analysis of the level of severity of depression (Fig. 1) on the basis of the symptoms in line with ICD-10 criteria documented by the physicians showed that 33% of the GPs' patients and 17% of the specialists' patients who had been included into the study due to having a diagnosis of depression, did not meet the criteria for a depressive episode according to the ICD-10. Therefore the following findings have only been calculated using the sample of depressed patients who met ICD-10 criteria (194 GPs' and 156 specialists' patients, ntotal = 350).
Figure 1. Severity of depression (documented symptoms of ICD-10 criteria by physicians) at the time of inclusion into study in comparison GPs' and specialists' patients.
Assessment tools
Documentation form (physician). The developed documentation tool for the care of depressed patients included information on sociodemographics, case history, consultation reasons, stress factors (axis IV of DSM-IV), ICD-10 diagnosis and criteria, clinical global impression (CGI; [24]) scale, therapeutic treatment, referrals and physician-patient-relationship. Additional structure variables concerning the physicians were documented: medical specialty, further qualifications and practice structures [25].
Patient questionnaire. The patients' assessment of depression symptoms was investigated using the German version of the nine-item depression module Brief-PHQ [26] of the Patient Health Questionnaire (PHQ; sensitivity: 73%- 84%; specificity: 88% - 98%; [27]), which is designed for use in primary care. It was developed as a self-report version of the PRIME-MD (Primary Care Evaluation of Mental Disorders; [28]). Each item of the PHQ depression module evaluates the presence of one of nine DSM-IV criteria of major depression.
Statistical methods
The data were descriptively analyzed. Comparison of the two groups (GPs vs. specialists) were performed using Wilcoxon-tests for independent samples (mean differences) and χ2-tests (categorical measures); 95% confidence intervals (95% CI) were evaluated. Bivariate correlations between variables and severity of depression (classification of symptoms of ICD-10 criteria: subsyndromal, mild, moderate and severe) were tested using the Spearman's nonparametic correlation coefficient test. The extent to which antidepressants were prescribed in correct doses (low dosage: under minimum effective dosage; over dosage: above recommended dosage) was investigated by means of guidelines recommendations of APA [18] and Benkert and Hippius [29]. Alpha-adjustment of Bonferroni was applied for the analysis of the patients' psychopathology (CGI severity, ICD-10 severity), diagnostic assessment, therapeutic measures and referrals. The change in depressive symptoms (B-PHQ) was analyzed by the percentage of difference between the first survey at time of inclusion into the study and the second survey after six to eight weeks (progression: negative sign; no change: 0 - 19%; little remission: 20 - 49%; partial remission: 50 - 99%; full remission: 100%; [30]).
Sample
Physicians. The sample is divided into 43 GPs (73% family physicians, 27% medical specialists) and 23 specialists (70% specialists for psychiatry, 30% specialists for psychiatry and psychotherapy). The mean age of GPs is 47.5 years (SD = 6.9; range: 36 - 63; 95% CI: 45.4 - 49.6) and of specialists 49.3 years (SD = 8.8; range: 28 - 64; 95% CI: 45.7 - 53.0). A total of 12% of the GPs and 77% of the specialists have an additional postgraduate qualification in psychotherapy and 72% of GPs and 75% specialists in psychosomatic primary care. Concerning the duration of establishment in private practice, there is no difference between the group of GPs (M = 11.5 years, SD = 7.2; 95% CI: 9.5 - 13.7) and the group of specialists (M = 12.5 years, SD = 9.0; 95% CI: 8.8 - 16.2). The majority of both groups work in their own practice. Specialists treat more than twice as many depressed patients per week (M = 39.4, SD = 23.3; 95% CI: 29.9 - 48.9) than GPs (M = 14.0, SD = 8.7; 95% CI: 11.4 - 16.6; Wilcoxon-test = 936.0, z = -4.925, p < 0.0001) and identify three times as many new depressive disorders per week (M = 6.2, SD = 3.4; 95% CI: 4.8 - 7.6) than GPs (M = 2.0, SD = 1.2; 95% CI: 1.6 - 2.4; Wilcoxon-test = 892.0, z = -4.939, p < 0.0001).
The subsample of physicians (n = 26) who had documented the course of treatment within the comparable time frame did not differ significantly from the total physicians sample (n = 66) in regard to the selected physicians' characteristics (age, gender, specialization, additional qualification in psychotherapy, years in own practice).
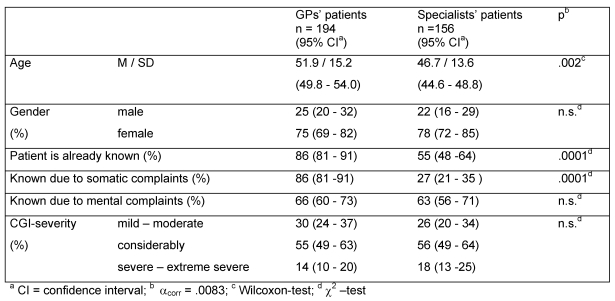
Patients. The patients in the GP sample (n = 194) have a higher mean age of 51.9 years (SD = 15.2; 95% CI: 49.8 - 54.0) than the specialists' patients (n =156) with 46.7 years (SD = 13.6; 44.6 - 48.8) ((Tab. 1); Wilcoxon-test = 18196.0, z = -2.745, p < 0.006). There is a similar distribution of gender in both groups, more than two thirds are female. In contrast to the patients in the specialists' sample, the GPs' patients were usually known before by their doctor (χ2 = 39.10, df = 1, p < 0.0001). 86% of the GPs' patients and only 27% of the specialists' patients were already known to the doctor due to previous somatic complaints (χ2 = 95.60, df = 1, p < 0.0001) and two thirds of the patients were known due to previous mental complaints. There are no differences on the severity scale of the CGI between both groups (Tab. 1): at time of inclusion into study more than half of the patients were considerably depressed. No differences were observed in regard to the average number of episodes (GPs' patients: M = 3.0, SD = 2.7; 95% CI: 2.6 - 3.4; specialists' patients: M = 4.2, SD = 10.6; 95% CI: 2.5 - 5.9). For both groups, the depressed patients in the study were separated into the diagnoses of a depressive disorder (F3x.xx: 95.9% GPs' and 94.1% specialists' patients) and adjustment disorder (F43.xx: 4.1% GPs' and 5.9% specialists' patients).
Table 1. Patients sample at inclusion into study .
The patient assessments in regard to the changes in depressive symptoms (B-PHQ) after six to eight weeks could be collected for about half of the depressed patients (subsample I: 73 GPs' and 92 specialists' patients, ntotal = 165). This group of patients did not differ significantly to the total sample (n = 350) in regard to patient characteristics (age, gender), severity of depression (CGI, symptoms of ICD-10-criteria) and treatment (antidepressant therapy, referrals to psychotherapy).
A medical judgement of the treatment outcome to be compared to one of the time points of the patients' ratings was available for 70 of the 165 depressed patients. This group of patients (subsample II: 37 GPs ' and 33 specialists' patients, ntotal = 70) did not significantly differ to the subsample I (ntotal = 165) as well as the origin sample (ntotal = 350) in regard to patient characteristics (age, gender), severity of depression (CGI, symptoms of ICD-10 criteria) and the treatment (antidepressant therapy, referrals to psychotherapy).
Results
Diagnostic assessment
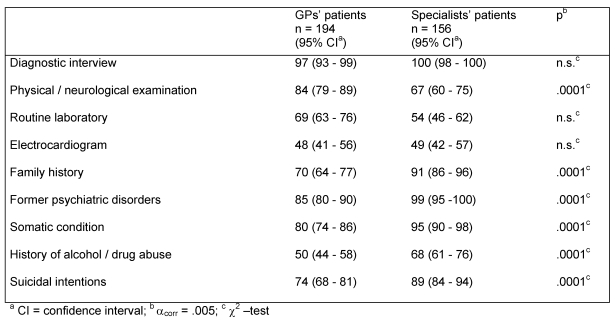
Nearly all physicians completed an assessment interview (Tab. 2) and 84% of GPs versus 67% of specialists had performed a physical/neurological examination (χ2 = 12.86, df = 1, p < 0.0001). Other diagnostic themes such as family history (70% of GPs vs. 91% of specialists; χ2 = 22.45, df = 1, p < 0.0001), former psychiatric disorder (85% of GPs vs. 99% of specialists; χ2 = 18.74, df = 1, p < 0.0001) and somatic condition (79% of GPs vs. 95% of specialists; χ2 = 17.27, df = 1, p < 0.0001) were more frequently investigated by the specialists. Only 50% of the GPs and 68% of the specialists had addressed the topic of comorbidity with alcohol or drug abuse (χ2 = 11.84, df = 1, p < 0.0001). Concerning suicidal intentions, distinct differences emerged: only 74% of the GPs vs. 89% of the specialists had explored suicidal intention of their patients (χ2 = 11.89, df = 1, p < 0.0001).
Table 2. Diagnostic assessments (in % "yes" and "already carried out / known") at inclusion into study .
A low correlation between the investigation of suicidal intention and the severity of depression (classification of symptoms of ICD-10 criteria: subsyndromal, mild, moderate and severe) was only found in the group of specialists (r = .28, p < 0.001): the more ill a patient was judged to be, the sooner the doctor was likely to address the subject of suicide with his patient.
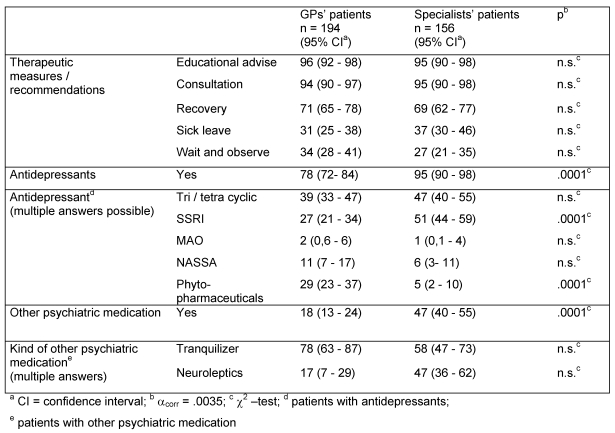
Therapeutic treatment
Nearly all physicians conducted therapeutic measures such as providing educational advice or general consultation (Tab. 3). One third of physicians had certified their patients' inability to work. Significant differences between both groups were found for the indication of psychopharmacological measures: 95% of specialists and 78% of GPs had treated their patients with antidepressants (χ2 = 18.25, df = 1, p < 0.0001). Further analysis of the type of medication prescribed showed that the specialists' patients were significantly more likely to be treated with SSRIs (51% specialists' patients vs. 27% of GPs' patients; χ2 = 17.31, df = 1, p < 0.0001) while the patients of GPs were more likely to have been treated with phytopharmaceuticals (29% of GPs vs. 5% of specialists; χ2 = 29.07, df = 1, p < 0.0001). Moreover, the GPs' treated 28% of cases of moderate as well as 16% of severe depression with phytopharmaceuticals.
Table 3. Therapeutic treatments (in %) at inclusion into study .
The use of antidepressants with regard to the severity of depression (classification of symptoms of ICD-10 criteria) demonstrate that the specialists were more likely to have prescribed antidepressants for severe depression (97%) than moderate (93%) or mild depression (88%). In contrast, the GPs' patients with severe depression (77%) received less antidepressants than patients with moderate (83%) or mild depression (81%).
The evaluation regarding dosages revealed no differences between the both groups of physicians: SSRIs (77% of the GPs' and 87% of the specialists' patients) as well as the modern antidepressants (91% of the GPs' and 89% of the specialists' patients) were prescribed in most cases in correct doses according to current guideline recommendations [18]. On the other hand, it has been showed that both groups frequently prescribed tri- and tetracyclic antidepressants in too low dosages (86% of GPs' and 75% of specialists' patients). Phytopharmaceutical antidepressants were only prescribed by the GPs in the recommended dosage in 4% of cases and in too low dosages in 78% of cases.
Nearly half of all specialists prescribed additional psychopharmacological medication, which is twice as many than in the group of GPs (47% of specialists' patients vs. 18% of GPs' patients; χ2 = 22.54, df = 1, p < 0.0001).
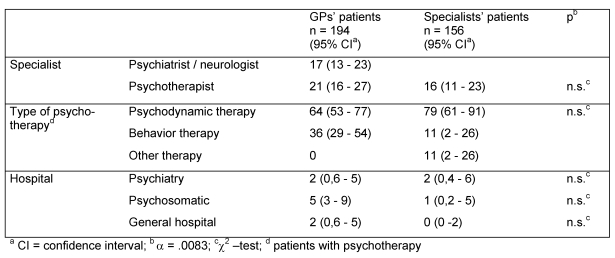
Referrals
At the time of inclusion into the study (Tab. 4), 17% of the GPs' patients were referred to specialists such as psychiatrists or neurologists. There was no difference in the number of referrals to psychotherapy between GPs' (21%) and specialists' patients (16%). Concerning type of psychotherapy, it was shown that the GPs' (n = 25) and specialists' patients (n = 19) were more likely to be referred to psychodynamic psychotherapy (64% of GPs' vs. 79% of specialists' patients) than to behavior therapy (36% of GPs' vs. 11% of specialists' patients).
Table 4. Ordering of referrals (in %) at inclusion into study.
Only a small number of physicians considered inpatient treatment to be necessary: 2% of patients per group were referred to a psychiatric hospital, 5% of the GPs' patients in comparison to 1% of specialists' patients were referred to a hospital of psychosomatic-psychotherapeutic medicine and 2% of the GPs' patients and none of the specialists' patients were referred to a general hospital.
In both groups no correlation between referrals to specialist, psychotherapist or psychiatric clinic and severity of depression (symptoms of ICD-10 criteria) was found: both mildly depressed patients and severely depressed patients were referred in the same manner.
Duration of visit and subsequent visit
In regard to the average duration of visit with patients, there is a small difference between both groups: GPs meet with patients for an average of 25.4 minutes (SD = 14.5, range: 5 - 85; 95% CI: 23.4 - 27.4) a little less than the specialists with 30.3 minutes (SD = 15.1, range: 10 - 90; 95% CI: 27.9 - 32.7; Wilcoxon-test = 27787.5, z = -3.432, p < 0.001). A correlation between the duration of visit and the severity of depression (symptoms of ICD-10 criteria) was only observed for specialists (r = .31, p < 0.0001): the more ill the patient was, the longer the treatment was indicated.
Almost all of the patients were requested to make further contact (96% of the GPs' and 99% of the specialists' patients). The time before the subsequent contact was on average 10.6 days for the GPs (SD = 7.4, Range: 1- 62; 95% CI: 9.6 - 11.4) and 14.3 days for the specialists (SD = 9.7, range: 1 - 60; 95% CI: 12.8 - 15.8; Wilcoxon-test = 22266.0, z = -3.865, p < 0.0001). In both groups the subsequent visit was dependent on the severity of depression (symptoms of ICD-10-criteria): severely depressed patients received an appointment sooner than mildly depressed. This correlation is only significant for the group of specialists (r = .40, p < 0.0001).
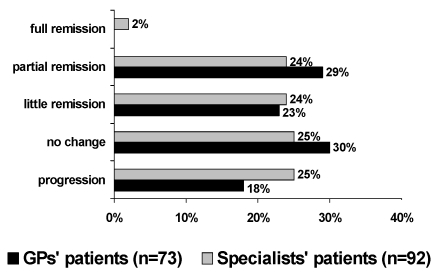
Treatment outcome
Patients. The investigation of depressive symptoms (B-PHQ) after six to eight weeks shows no statistical significant difference between the two groups any more (Fig. 2): the symptoms for 25% of GPs' patients and 18% of specialists' patients even progressed. A partial to full remission (50 - 100%) demonstrated 29% of GPs' and 26% of specialists' patients. No change in depressive symptoms was reported by 25% of GPs' and 30% of specialists' patients. The change of depressive symptoms after six to eight weeks did not depend on the severity of depression (symptoms of ICD-10 criteria) at time of inclusion into study: there was partial to full remission for 28% of severe vs. 30% of mildly depressed patients. A progression of symptoms was described by 21% of severely and 30% of mildly depressed patients. Moreover, there was no correlation between the change of depressive symptoms and average duration of depression, antidepressant therapy or referral to psychotherapists.
Figure 2. Change of depressive symptoms after six to eight weeks using patients' self-assessment (Brief-PHQ).
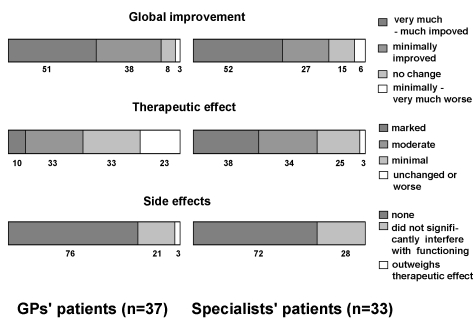
Physicians. The global improvement (CGI) revealed no significant differences between both groups (Fig. 3): 89% of the GPs and 79% of the specialists regarded the condition of the patients to have improved. In regard to the rating of the therapeutic effect of previous medication (CGI), a significant difference between GPs and specialists was found (χ2 = 10.12, df = 3, p < 0.018): 66% of the GPs vs. 72% of the specialists stated that the medication was only a minimally or moderately effective, and 10% of the GPs vs. 38% of specialists stated the mediation was being markedly effective. In regard to the side effects of medication, the two groups of physicians did not differ to one another (Fig. 3): more than two thirds of the patients were not specified by the physicians to have experienced side-effects (76% of GS and 72% of specialists).
Figure 3. Success of therapy from the viewpoint of physicians after six to eight weeks.
(CGI: global improvement, therapeutic effect, side effects)
Discussion
The results demonstrate that diagnostic assessment, therapeutic measures and referral behavior in depression treatment are still rarely orientated towards guidelines, in particular by general practitioners, but also by specialists. This appears to be reflected in inadequate treatment outcome from the view of the patients: whilst half of both the GPs' and specialist patients reported a reduction in depressed symptoms after six to eight weeks the other half demonstrated a stagnation or even a progression of symptoms. Means for general practitioners and specialists to improve outpatient treatment of depression were identified.
Results indicate a low routine use of diagnostic criteria for depression (ICD-10) by GPs and specialists. For 33% of GPs and 17% of specialists, no correspondence was found between the clinical diagnosis of patients in the study and the documented ICD-10 criteria for a depressive episode at inclusion into the study. This outcome has also been demonstrated in other studies which report that unstructured and less formal diagnostic assessment is determined by the frequently insufficient use of diagnostic criteria [4], [31]. It seems that diagnoses of depression still result from the subjective assessments of physicians [32]. Further means of improving diagnostic strategies were identified with regard to the investigation of differential diagnosis, suicidal risk and comorbidity. GPs in particular only inquired about suicidal intentions in about 74% of cases. These deficits in diagnostic assessment, in addition to others, could result in fewer and delayed referrals to specialists, psychotherapists or psychiatric hospitals [9], [33]. According to guidelines for depression treatment [18], [19], the referral of patients with moderate to severe depression, high suicidal risk or comorbidity is particularly recommended. The influence of suicide risk on referral behavior was not investigated. The results in regard to referral behavior suggest that identified opportunities to improve depression care are especially related to the pathway of care between GPs, psychiatrists, psychotherapists and psychiatric-psychotherapeutic hospitals. The high extent of referrals of GPs to psychosomatic/psychotherapeutic clinics or of referrals of both groups to psychodynamic-oriented therapists seems to be influenced more by local circumstances than by guideline recommendations.
Regarding therapeutic measures, most of the physicians acted according to the indication and current treatment guidelines. Therefore the intervention usually consists of educational advice or consultation and psychopharmacological treatment with antidepressants. However, the specialists prescribed statistically significantly more antidepressants than the GPs and the indication of antidepressants depended on severity of depression: according to the guideline recommendations for depression, the specialists were more likely to treat a patient with moderate or severe depression with antidepressants. In contrast to the specialists, the psychopharmacological treatment by GPs was not constantly orientated to guidelines: they prescribed antidepressants independent of the severity of depression and often treated moderate or severe depression with phytopharmaceuticals. Obviously, GPs generally preferred to prescribe phytopharmaceuticals more than the specialists. By way of contrast, the specialists were more likely to treat a patient with additional psychiatric medication, probably due to their greater experience in psychopharmacology or patient's comorbidity . In total, the assessment of antidepressant treatment highlights the fact that dosages in both groups were not always prescribed to an optimal level [18], [29]. However, the therapeutical effectiveness of previous medication was rated by physicians in both groups to be very positive, only 23% of the GPS and 3% of the specialists did not believe the medication had been effective. Moreover, only few side-effects were documented by the physicians.
An important finding is that the treatment outcome was differently rated by physicians and their patients and no relevant association between the physicians' and patients' ratings could be established. While about a half of the patients (52% of the GPs' and 50% of the specialists' patients) reported a subjective improvement in their symptoms and the other half no improvement or even a progression, the physicians regarded the outcomes to be more positive: An improvement in symptoms was documented by 89% of the GPs and 79% of the specialists. The patients' personal evaluation of the success of the therapy sometimes differed to the clinical assessment of their physicians. Furthermore, probably because of general negative thoughts of the depressed patients discrepancies between self-ratings and expert ratings concerning severity of depression were obvious. A further methodological explanation for this discrepancy is being sought in the use of different instruments for patients (B-PHQ) and physicians (CGI).
A correlation between treatment outcome from the view of the physicians and patients and the severity of depression (symptoms of ICD-10 criteria) could not be proved. Moreover, the treatment outcome was not dependent on therapeutic measures such as applied antidepressant therapy, the type of antidepressant or referral to a psychotherapist.
When interpreting the data, it must be considered that the documentation of physicians at the first visit is not always carried out in a complete manner and may to an extent have been insufficiently completed. Further limitations relate to results regarding the course of therapy (therapy resistance, chronification) and conclusions made about therapeutic measures and treatment outcome related to the total sample, since the patients assessment regarding treatment outcome was only available for half of the total sample. Concerning the main conclusion of the present study, the risk of possible biases (e.g. selection bias) due to the high rate of missing data as well as the small sample should be pointed out. Due to the design of an intervention study, the physicians were not selected randomly. The evaluation of the representativeness of participating physicians shows that the sample was representative of outpatient care in Germany in 2001 [34] in regard to selected structure variables (age, gender, medical specialization, single practice).
The problem of underdiagnosis and undertreatment has already been described in other studies [4], [16], [35], [36], [37], [38]. Moreover, the study identified opportunities to improve the treatment of depression in outpatient settings which are not only related to diagnostic and therapeutic measures but also to the pathway of care between GPs, specialists, psychotherapists, and psychiatric hospitals. In practice it became apparent that the development and extension of recommendations for treatment were not sufficient, rather specific and supporting programs for implementation and establishment of guidelines are required [10], [39].
The implications of these results underline the need for training in current guidelines of depression care and more consistent multidisciplinary networking between GPs, specialists, psychotherapists and psychiatric hospitals. The use of suitable and economical screening instruments for depressive disorders (e.g. B-PHQ) in practice could improve the diagnostic accuracy. A quality management intervention program with guideline-oriented training and interdisciplinary quality circles for improvement of the outpatient treatment in depression care is currently being evaluated by the authors [23], [40]. Preliminary results have shown positive effects on quality of diagnostic assessment and therapeutic treatment as well as on the assessment of the intervention by the participating GPs and specialists.
Acknowledgements
The present study was supported by the German Ministry for Education and Research (BMBF; FKZ 01 GI 9922) within the promotional emphasis "German Research Network on Depression": Subproject 3.1 "Comprehensive Quality Management in Outpatient Care" and was realized in co-operation with medical practices in North Rhine Westfalia, South Baden and Bavaria. We thank Dr. Frank Bergmann, Dr. Wilhelm Niebling, Dr. Rolf Peters, and Dr. Rolf-Dieter Stieglitz for support.
References
- 1.Goldberg D. Epidemiology of mental disorders in primary care settings. Epidemiol Rev. 1995;17(1):182–190. doi: 10.1093/oxfordjournals.epirev.a036174. [DOI] [PubMed] [Google Scholar]
- 2.Simon GE, von Korff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med. 1995;4(2):99–105. doi: 10.1001/archfami.4.2.99. [DOI] [PubMed] [Google Scholar]
- 3.Üstun TB, Sartorius N, editors. Mental illness in general health care: an international study. Chichester: Wiley; 1995. [Google Scholar]
- 4.Wittchen HU, Pittrow D. Prevalence, recognition and management of depression in primary care in Germany: the Depression 2000 study. Hum Psychopharmacol. 2002;17 Suppl 1:S1–11. doi: 10.1002/hup.398. [DOI] [PubMed] [Google Scholar]
- 5.WHO International Consortium in Psychiatric Epidemiology. Cross-national comparisons of prevalences and correlates of mental disorders. Bull World Health Organ. 2000;78(4):413–426. [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatients services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156:115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- 7.Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. J Gen Intern Med. 2000;15(5):284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Von Korff M, Tiemen B. Individualized stepped care of chronic illness. West J Med. 2000;172(2):133–137. doi: 10.1136/ewjm.172.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paykel ES, Tylee A, Wright A, Priest RG, Rix S, Hart D. The Defeat Depression Campaign: psychiatry in the public area. Am J Psychiatry. 1997;154(6 Suppl):59–65. doi: 10.1176/ajp.154.6.59. [DOI] [PubMed] [Google Scholar]
- 10.Siriwardena AN. Clinical guidelines in primary care: a survey of general practitioners’ attitudes and behavior. Br J Gen Pract. 1995;45(401):643–647. [PMC free article] [PubMed] [Google Scholar]
- 11.Hickie IB. An approach to managing depression in general practice. Med J Aust. 2000;173(2):106–110. doi: 10.5694/j.1326-5377.2000.tb139255.x. [DOI] [PubMed] [Google Scholar]
- 12.Kratz S, Härter M, Bermejo I, Berger M, Gaebel W, Schneider F. Beratungsanlass und Diagnosestellung bei depressiven Patienten in der hausärztlichen Praxis. Z Ärztl Fortbild Qualitätssich. 2003;97 Suppl 4:50–56. [PubMed] [Google Scholar]
- 13.Simon GE, vonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341(18):1329–1335. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 14.Thompson C, Kinmonth AL, Stevens L, Peveler RC, Stevens A, Ostler KJ, Pickering RM, Baker NG, Henson A, Preece J, Cooper D, Campbell MJ. Effects of clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trail. Lancet. 2000;355(9199):185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 15.Linden M. Depressive Erkrankungen und antidepressive Therapie. Ein Vergleich von Nervenarztpraxis und psychiatrischer Klinik. Nervenarzt. 2001;72(7):521–528. doi: 10.1007/s001150170076. [DOI] [PubMed] [Google Scholar]
- 16.Keller MB. The difficult depressed patient in perspective. J Clin Psychiatry. 1993;54 Suppl:4–8. [PubMed] [Google Scholar]
- 17.Lave JR, Frank RG, Schulberg HC, Kamlet MS. Cost-effectiveness of treatments for major depression in primary care practice. Arch Gen Psychiatry. 1998;55(7):645–651. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association (APA) Practice guideline for the treatment of patients with major depressive disorder. 2nd ed. Washington, DC: American Psychiatric Association; 2000. [PubMed] [Google Scholar]
- 19.Gaebel W, Falkai P, editors. Behandlungsleitlinie Affektive Erkrankungen. Darmstadt: Steinkopff; 2000. (Praxisleitlinien in Psychiatrie und Psychotherapie; Bd. 5). [Google Scholar]
- 20.Institute for Clinical Systems Improvement (ICSI) Health Care Guideline: major depression in specialty care in adults. Bloomington (MN): Institute for Clinical Systems Improvement; 2000. [Google Scholar]
- 21.Katon W, Robinson P, von Korff M, Lin E, Bush G, Ludman E, Simon G, Walker W. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiatr. 1996;53(10):924–932. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 22.Kerrek-Bodden H, Koch H, Brenner G, Flatten G. Diagnosespektrum und Behandlungsaufwand des allgemeinärztlichen Patientenklientels. Ergebnisse des ADT-Panels des Zentralinstituts für die Kassenärztliche Versorgung. Z Ärztl Fortbild Qualitätssich. 2000;94(1):21–30. [PubMed] [Google Scholar]
- 23.Härter M, Bermejo I, Schneider F, Gaebel W, Niebling W, Berger M. Umfassendes ambulantes Qualitätsmanagement in der Versorgung depressiver Störungen. Z Ärztl Fortbild Qualitätssich. 2003;97 Suppl 4:9–15. [PubMed] [Google Scholar]
- 24.Guy W, editor. ECDEU Assessment Manual for Psychopharmacology. Rev. ed. Rockville, MD: National Institute of Mental Health; 1976. Clinical Global Impressions. [Google Scholar]
- 25.Bermejo I, Schneider F, Kratz S, Härter M. Entwicklung und Evaluation einer Basisdokumentation zur ambulanten Versorgung depressiver Patienten. Z Ärztl Fortbild Qualitätssich. 2003;97 Suppl 4:36–43. [PubMed] [Google Scholar]
- 26.Löwe B, Zipfel S, Herzog W. Gesundheitsfragebogen für Patienten (PHQ-D) Karlsruhe: Pfizer; 2002. [Google Scholar]
- 27.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 28.Spitzer RL, Williams JB, Kroenke K, Linzer M, de Gruy III FN, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 29.Benkert O, Hippius H. Kompendium der psychiatrischen Pharmakotherapie. 2., überarb. Aufl. Berlin: Springer; 2000. [Google Scholar]
- 30.Crismon ML, Trivedi M, Pigott TA, Rush AJ, Hirschfeld RM, Kahn DA, DeBattista C, Nelson JC, Nierenberg AA, Sackeim HA, Thase ME. The Texas Medication Algorithm Project: report of the Texas Consensus Conference Panel on Medication Treatment of Major Depressive Disorder. J Clin Psychiatry. 1999;60(3):142–156. [PubMed] [Google Scholar]
- 31.Höfler M, Wittchen HU. Why do primary care doctors diagnose depression when diagnostic criteria are not met? Int J Methods Psychiatr Res. 2000;9(3):110–120. [Google Scholar]
- 32.Williams JW, Jr, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J. Primary care physicians` approach to depressive disorders. Effects of physician speciality and practice structure. Arch Fam Med. 1999;8(1):58–67. doi: 10.1001/archfami.8.1.58. [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, de Gruy III FN, Brody D, Davies M. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA. 1995;274(19):1511–1517. [PubMed] [Google Scholar]
- 34.Die ärztliche Versorgung in der Bundesrepublik Deutschland zum 31. Dezember 2001. Ergebnisse der Ärztestatistik der Bundesärztekammer und der Kassenärztlichen Bundesvereinigung. Köln: Deutscher Ärzte-Verlag; 2002. [Google Scholar]
- 35.Goldman LS, Nielsen NH, Champion HC. Awareness, diagnosis, and treatment of depression. J Gen Intern Med. 1999;14(9):569–580. doi: 10.1046/j.1525-1497.1999.03478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schneider F, Dausend S, Gaebel W, Bermejo I, Berger M, Härter M. Ambulantes Qualitätsmanagement in der hausärztlichen Depressionsbehandlung. Hausarzt-Kolleg Neurologie Psychiatrie. 2003;1:70–73. [Google Scholar]
- 37.Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry. 1998;55(12):1121–1127. doi: 10.1001/archpsyc.55.12.1121. [DOI] [PubMed] [Google Scholar]
- 38.Simon GE, Lin EHB, Katon W, Saunders K, Von Korff M, Walker E, Bush T, Robinson P. Outcomes of "inadequate" antidepressant treatment. J Gen Intern Med. 1995;10(12):663–670. doi: 10.1007/BF02602759. [DOI] [PubMed] [Google Scholar]
- 39.Davis D, O’Brian MA, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282(9):867–874. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 40.Härter M, Bermejo I, Kratz S, Schneider F. Fortbildungs- und Qualitätsmanagement-Maßnahmen zur Implementierung von Versorgungsleitlinien. Z Ärztl Fortbild Qualitätssich. 2003;97 Suppl 4:67–73. [PubMed] [Google Scholar]