Abstract
Objective
To provide estimates of the growth in out-of-pocket medical expenditures for persons with arthritis.
Methods
Medical and out-of-pocket expenditures were estimated for 1998–2004 based on seven panels of the Medical Expenditures Panel Survey (MEPS), which provides nationally representative data. A simple simulation then extrapolated the data through 2006, where the potential effects of the Medicare Part D drug coverage were computed.
Results
Median Out-of-Pocket expenditures for persons with arthritis show 52.5% growth in total OOP expenditures between 1998 and 2004 (7.3% annually beyond inflation). Median OOP expenditures for prescription medication show larger growth, at 72.1%. Medicare Part D was predicted to lower both total and prescription OOP expenditures and return them close to 2003 levels. Simulation limitations include simplified Medicare Part D rules and assumed stable prescription trends during this period.
Conclusions
High prescription drug expenditures are likely to continue to be an issue for both individuals faced with increasing OOP burden and for policy-makers faced with increasing budgetary shortfalls to fund increasing Medicare expenses.
Introduction
Individuals with arthritis have higher medical expenditures than persons without arthritis (1,2,3). Limited insurance coverage of prescription medicines, the aging of the population and growing reliance on expensive drugs have combined to increase in economic burden faced by individuals with arthritis. (4,5).
Economic burden on individuals is reflected in their overall expenditures for medical care, but is more closely tied to out-of-pocket (OOP) expenditures, how much an individual must pay for care through copayments and deductibles not covered by private or government insurance. The burden of prescription drug costs, in particular, has become a major policy issue due to growing utilization of prescription drugs (6), rising drug prices, and limited availability of good prescription drug coverage(7). Looking at all individuals with arthritis, Yelin et al (8) find the amount Americans spent on arthritis medications more than doubled between 1998 and 2003. For the elderly, greater medical expenses combined with limited income results in an increasing out-of-pocket burden for this population (9). The Medicare Part D drug benefit, implemented in 2006, was in response to these concerns. However, the large copayments associated with the Medicare plan led to questions as to its ability to meet increasing needs.
This paper addresses these concerns by examining the out-of-pocket (OOP) expenditures of persons with arthritis. We assess the recent OOP growth across the expenditure distribution for both total OOP expenditures and OOP expenditures for prescription medication. In addition we simulate the effect the new Medicare D drug program may have had on these expenditures.
Specifically, we use nationally representative medical expenditure data between 1998 and 2004 to address the following questions: 1) Did Medicare aged individuals over age 65 with arthritis experience a substantial growth in total out-of-pocket (OOP) expenses? and 2) what was the likely impact of Medicare Part D drug coverage on OOP expenditures?
DATA AND METHODS
Data and Study Population
This study uses seven sequential panels from 1998–2004 (second to eighth) of the Medical Expenditure Panel Survey (MEPS). MEPS is a probability sample of the U.S. civilian non-institutionalized population. The MEPS Household Component (MEPS-HC) uses an overlapping panel design in which data are collected by a series of five interviews over a 30 month period (10). Person level data are collected on medical expenditures with detailed information regarding payment source (OOP, Medicare, Medicaid, etc.). This study focuses on total OOP payments and OOP for prescription medications. Our analysis sample includes 3, 758 individuals with arthritis aged 65 and older at their baseline interview who participated in all five interviews of one of the seven 1998–2004 MEPS panels. (We exclude 2 observation due to lack of self-reported health status information).
Identification of Arthritis
Arthritis and other chronic conditions were ascertained from systematic medical interviews from the first year of each panel. Specific conditions were assigned three digit diagnosis ICD-9 codes and are maintained in a MEPS condition file. The identification of arthritis is based on the ICD9 codes used by the National Arthritis Workgroup (11) using the MEPS truncated three-digit ICD-9 codes: 710-716, 719-721 and 725-728. Other chronic conditions are identified in a similar manner and include: hypertension, diabetes, cancer, pulmonary disease, heart disease, stroke, mental disorder and neurological disorder.
OOP Expenditures
MEPS-HC provides total and OOP expenditures for each individual for the following type of services: ambulatory care visits, physician office visits, emergency room visits, hospital inpatient stays, prescription medications, and other medical expenditures related to home health care, dental care, ambulance services, orthopedic items, hearing devices, prostheses, bathroom aids, medical equipment, disposable supplies, alterations/modifications, and miscellaneous items or services that were obtained, purchased or rented during the monitored year. We focus on total OOP expenditure and OOP for prescription medication because prescription costs represent on average more than 50% of all OOP expenditures. We use the first year of medical data to identify persons with arthritis-related diagnoses and the second year to ascertain medical expenses. MEPS provides expenditures for each individual from ambulatory care visits, physician office visits, emergency room visits, hospital inpatient stays, prescription medications, and other medical expenditures (home health care, dental care, ambulance services, orthopedic items, and miscellaneous items or services). Total OOP expenditures are the sum of ambulatory care, physician office visits, emergency room visits, hospital inpatient, prescription drugs and other medical OOP expenditures. All expenditures are adjusted for inflation using the annual Consumer Price Index not seasonally adjusted (CPI-U) and are in 2004 dollars.
Data Analysis
All analyses on total OOP and prescription OOP medication expenditures use a sample limited to those adults age 65 or older having a MEPS arthritis-designated ICD9 code with population weights to provide inferences regarding the older US adult population with arthritis. OOP expenditures for the median, 75th percentile and 90th percentile are estimated using quantile regression. Quantile regression, which models median (or 75th or 90th percentile) OOP expenditures, is analogous to least squares regression that models the mean outcome. Since quantile regression is robust to outliers and does not require assumptions regarding the underlining distribution of the outcome to obtain valid inference tests, the method is advantageous for modeling outcomes which are not normally distributed (12). The variance of the quantile regression estimates is estimated using bootstrapping to account for potential correlation among outcomes due to the complex sampling design (13).
The quantile regression estimates adjust for age, age squared, race/ethnicity, marital status, education, income,1 self-reported health insurance status2 and number of chronic conditions. Results of both total OOP and prescription medication expenditures are estimated in reference to a white, single female, 75 years old with up to 12 years of schooling, income of $23,585 in 2004 dollars in good health and one other chronic condition beside arthritis. The OOP difference between the adjusted 1998 and 2004 expenditure estimates, and the associated confidence interval (CI) are also estimated. A 95% CI that excludes zero indicates a statistically significant difference.
Simple Simulation of Medicare part D on OOP expenditures
Medicare part D can potentially change the OOP expenditures that individuals experience (14,15,16). To investigate the maximum possible effect of Medicare part D we use the 2004 MEPS sample of Medicare aged adults(≥65 years), the last year of data available from MEPS, to simulate OOP expenditure in the years 2005 and 2006. We projected total OOP and prescription medication OOP expenditures for the years 2005 to 2006 by assuming the average growth rates in OOP expenditures for prescription and non-prescription medical expenditures between 1998 and 2004 would continue from 2004 to 2006. To estimate the maximum likely benefit, the simulation of 2006 OOP expenditures makes two assumptions. First it assumes that individuals choose the standard drug benefit under Medicare part D rather than keep their existing drug insurance if and only if their OOP prescription medication expenditures under the standard Medicare plan would be lower than their projected 2006 OOP prescription medication expenditures, which are in turn based on extrapolated their 2004 out-of-pocket expenditures. Because we assume the trend in out-of-pocket prescription drug expenditures continues through 2006, we are implicitly assuming there was no sudden change in private drug insurance coverage given the implementation of Medicare Part D in 2006. Second, it assumes that all expenditures for medication are included in the Medicare formulary.
The standard Medicare part D plan assumes the following schedule of OOP payments: 1) the patient pays first $250 and then pays 25% of cost beyond $250 until total prescription drug payments reach $2,250, 2) the patient is responsible for all drug expenses between $2,250 and $5,850, and 3) the patient then also pays 5% OOP of any drug expenses beyond $5,850.
Results
Our sample from the MEPS of 3, 758 respondents age 65 or older represents 9.5 million older Americans with arthritis in 1998 and grows to 12.7 million in 2004. Table 1 shows the sample characteristics of the arthritis population in 1998 and 2004. This population is largely comprised of white females. Consistent with demographic trends, this older age group over time included more individuals with higher education (26.7% to 39.2%) (17). Also consistent with population trends, inflation adjusted median income dropped between 1998 and 2004 (18). Table 2 presents the adjusted median, upper quartile and the 90th percentile of OOP prescription medication expenditures (Panel A) and total OOP (Panel B) for persons with arthritis in 1998 and 2004. Panel A shows that the median adjusted expenditure for prescription medication rose significantly between 1998 and 2004, from $415 to $714 (in 2004 dollars). This increase represents a growth of 72.1 percent (about 9.5% annually) beyond inflation during a time when inflation-adjusted income was declining. High OOP prescription medication expenditures, represented by the 75th and 90th percentiles also significantly increased over this period with 64% growth for the 75th percentile and 77% growth for the 90th percentile, in 2004 dollars). Panel B shows similar results for total OOP. The adjusted median total OOP expenditure increased significantly by $397 between 1998 and 2004 (from $757 in 1998 to $1, 154 in 2004). This represents an annual average growth of 7.3% beyond inflation for persons 65 and older with arthritis. Similar analysis for diabetes and heart disease show average annual growth rates in total OOP of 5.8% and 8.5% respectively.
Table 1. Characteristics of Arthritis Populations in 1998 and 2004.
| Demographic Characteristics | 1998 | 2004 |
|---|---|---|
| (n=465) | (n=671) | |
| Age: Mean (Standard Deviation [SD]) | 74.9 (6.64) | 75.0 (6.31) |
| Individual Income in $2004: Mean (SD) | $27,454 ($36,602) |
$23,585 ($19,585) |
| More Than High School Education (%) | 26.7% | 39.2% |
| Male | 34.0% | 32.5% |
| Married | 51.4% | 46.9% |
| White | 90.4% | 90.1% |
| Number of Chronic Disease: Mean (SD) | 1.49 (1.10) | 1.68 (1.13) |
| Health: Excellent | 11.6% | 13.4% |
| Health: Very Good | 23.2% | 26.4% |
| Health: Good | 37.5% | 32.0% |
| Health: Fair | 18.0% | 20.2% |
| Health: Poor | 9.8% | 8.0% |
Table 2. Adjusted Total Out-of-Pocket and Out-of-Pocket Expenditures for Prescription Drugs 1998 Vs. 2004 for Adults with Arthritis Age 65 or Older.
(Expenditures in 2004 Dollars adjusted for age, gender, marital status education, income)
| 1998 | 2004 | Difference [95% CI] |
|
|---|---|---|---|
| Panel A: Out-of-Pocket Expenditures for Prescription Drugs | |||
| Median | 415 | 714 | 299 [200,435] |
| 75th Percentile | 906 | 1,482 | 576 [347,791] |
| 90th Percentile | 1,602 | 2,830 | 1,227 [523,1638] |
|
| |||
| Panel B: Total Out-of-Pocket Expenditures | |||
| Median | 757 | 1,154 | 397 [256,581] |
| 75th Percentile | 1,334 | 2,014 | 681 [419,1,080] |
| 90th Percentile | 2,452 | 4,196 | 1,743 [855,2,396] |
Note: Bootstrapped Confidence Interval in squared brackets. Reference group: white, female, age 75, not married, in good health, 12 years education, mean income ($23,585 in 2004 dollars) with one other chronic condition.
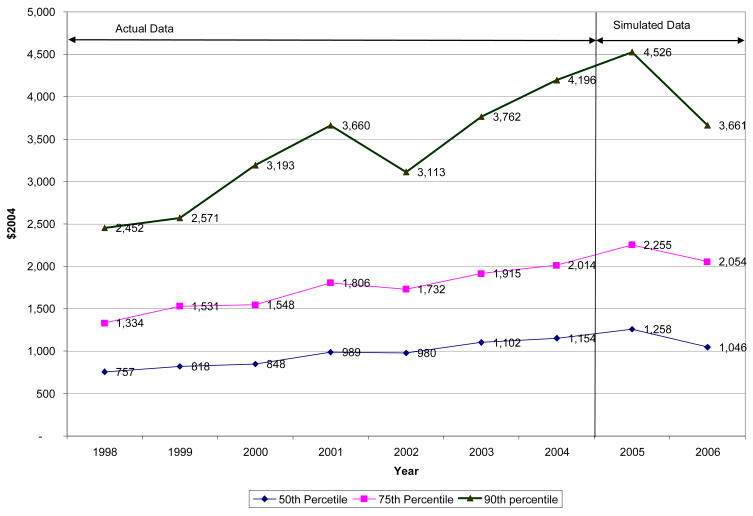
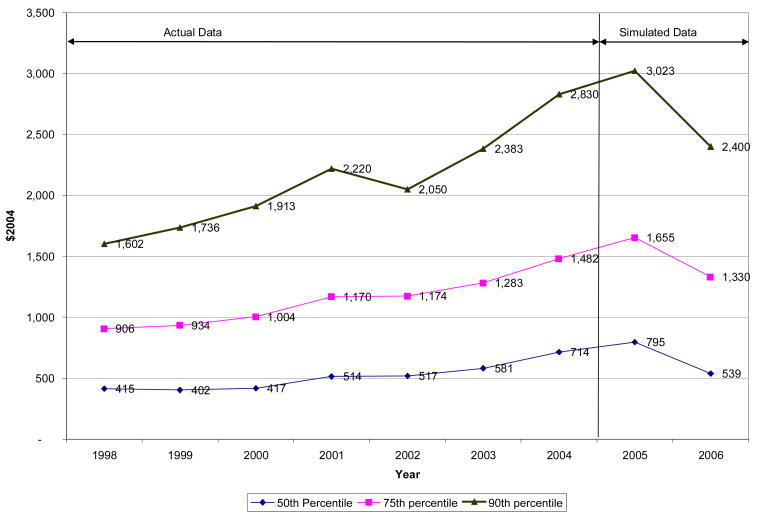
Figure 1 displays the distribution of adjusted total OOP expenditures for the years 1998 to 2004 and simulated projections OOP expenditures for the years 2005 and 2006, based on these inflation-adjusted growth rates observed from 1998 to 2004. The 2006 OOP expenditures simulate the implementation of Medicare part D. The simulation projects that median OOP expenditures could fall by as much as $211 (in 2004 dollars) from the 2005 level (from $1,258 in 2005 to $1,046 in 2006) after controlling for age, gender, marital status, education, health status and income. Individuals at the 75th percentile of total OOP expenditures show a projected decline of $200 and for the 90th percentile, the decline is about $865. Figure 2 shows the distribution of adjusted prescription medication OOP. Although prescription OOP expenditures consistently grow from 1998 to 2004, the simulated effect of Medicare part D indicates the maximum extent to which it could constrain those expenditures, if people make rationale Medicare part D decisions and their prescription drugs are included it the Medicare formulary. Medicare part D is projected to impede prescription medication OOP expenditures by 2006, and move them back towards 2003 levels, for each of the median, 75th and 90th percentile levels.
Figure 1.
Distribution of Total Out-of-Pocket Expenditures for Adults with Arthritis Age 65 or Older Adjusted for Age, Gender, Marital Status, Education, Income
Figure 2.
Distribution of Out-of-Pocket Expenditures of Prescription Drugs for Adults with Arthritis Age 65 or older Adjusted for Age, Gender, Marital Status, Education, Income
Discussion
Increased out-of-pocket medical expenses have substantially outpaced inflation for persons with arthritis aged 65 and older, a group that largely lives on fixed incomes. From 1998 to 2004, median OOP medical expenditures increased at an average annual rate of 7.3 percent after adjustment for general inflation. This increase is similar to the OOP rate of growth among persons with diabetes and heart disease. The OOP increase in median expenditures for prescription drugs increased even more, at an annual rate of approximately 9.5%, or 72% growth over the entire period as compared to 52.5% growth for all OOP medical expenditures. These increases in inflation adjusted median medical expenditures can be contrasted against inflation-adjusted median income, which did not increase over this period.
Given the increased OOP burden on the elderly and the major contribution of prescription drugs to this increase, the implementation of Medicare Part D drug coverage would be expected to impede this increasing burden. And, indeed, our simulation of its effects show a substantial decrease in total and prescription out-of-pocket expenditures due to the implementation of Medicare Part D, tending to move OOP expenditures back toward the 2003 levels of OOP expenditures.
Limitations inherent to the MEPS data and our simulation assumptions may limit the accuracy of these findings. It was not possible to reliably attribute specific rheumatic disorders (e.g., rheumatoid arthritis) to increased OOP expenditures. Simulated Medicare Part D estimates are based on some very simple but generous assumptions regarding the plan and who would switch from current to Part D insurance. We assume that all prescription medications would be included in Medicare Part D formulary, that people would be able to determine whether Medicare Part D would provide better coverage than their current plan, and that people are rational in their decisions. If current insurance coverage (extrapolated to 2006 from the observed years) pays more than Medicare Part D, we assume current coverage is maintained even though it is possible that drug coverage has deteriorated over time given that Medicare Part D has become a viable alternative. In addition we use the Standard Medicare Part D benefit structure described in the methods section when figuring out the out-of-pocket expenditures under the Medicare Plan. In actuality, there are a host of alternative Medicare plans offered that may provide coverage more tailored to individual circumstances, and thus the burden under the Medicare Plan could be lower than our simulation suggests (19,20). However, since the Standard Part D plan is the basis for payment of insurance intermediaries, these plans are not likely to be overly generous relative to the standard plan. For example, lower copayments are likely to be accompanied by more restrictions on which types of drugs are covered or to be directed at populations with lower prescription drug needs. Finally, we assumed that the growth in prescription expenditures was the same from 2004–2006 as in the prior period. This may not be the case. For example, a large part of the increase in cost of medications for OA was coxibs through 2004, but many older patients have converted to non-selective NSAIDs. It is also unlikely that the growth in expenditures on biologics has been constant over this period.
While the maximum impact of Medicare Part D coverage would clearly have a substantial effect on constraining overall OOP burden, it would not be sufficient to offset the increasing burden faced by individuals over time. The OOP expenses in 2006 are still estimated to be similar to 2003 levels, even under generous assumptions regarding the people who would use those benefits. As individual drug expenditures move into ranges where copayments drastically increase under Medicare plans, large increases in OOP expenditures can again be expected.
Medicare Part D coverage places a large responsibility on persons with arthritis to choose a plan that maximizes their benefits. The use of new expensive drugs by many persons with arthritis makes it important to make sure such drugs are on the formulary of the drug plan chosen and the use of expensive drugs such as biological agents also requires beneficiaries to calculate the relative merits of plans with different copayment structures. Because one may change drugs frequently over time in response to changes in medical condition, changes in our overall knowledge of drug effects, and the introduction of new drugs on the market, it may be necessary for many arthritis patients to reevaluate their coverage with their physician and pharmacist annually.
The rising effectiveness and costliness of drugs is likely to continue despite Part D coverage. The continuing growth of prescription medication expenditures coupled with the overall decline in income for persons over 65 will result in financial burden growing over time for the Medicare Population. The availability of data on actual expenditures for 2006 and beyond will provide further information on the growth of OOP burden, the impact of Medicare Part D, and potential improvements in medical care coverage and design they may be more effective in reducing out-of-pocket burden.
Acknowledgments
Grant Support: This study is supported in part by funding from NIH/National Institute for Arthritis and Musculoskeletal Diseases P60-AR48098, and NIH/ National Center for Medical Rehabilitation Research R01-HD45412.
Footnotes
We calculated income based on whether the person with arthritis is single or married. For single individuals we used their reported income. For an individual who is married we calculated the average income of his/hers income and his/hers spouse
Indicator variables were used to track each of the five self-reported health status categories (excellent, very good, good, fair and poor).
References
- 1.Yelin E, Herrndorf A, Trupin L, Sonneborn D. A national study of medical care expenditures for musculoskeletal conditions: the impact of health insurance and managed care. Arthritis Rheum. 2001;44:1160–1169. doi: 10.1002/1529-0131(200105)44:5<1160::AID-ANR199>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 2.Yelin E, Cisternas MG, Pasta DJ, Trupin L, Murphy L, Helmick CG. Medical care expenditures and earnings losses of persons with arthritis and other rheumatic conditions in the United States in 1997: total and incremental estimates. Arthritis Rheum. 2004;50:2317–2326. doi: 10.1002/art.20298. [DOI] [PubMed] [Google Scholar]
- 3.Dunlop DD, Manheim LM, Yelin EH, Song J, Chang RW. The costs of arthritis. Arth Rheum. 2003;49:101–113. doi: 10.1002/art.10913. [DOI] [PubMed] [Google Scholar]
- 4.Regenstir J. The prevalence and burden of arthritis. Rheumatology. 2002;41(suppl 1):3–6. [PubMed] [Google Scholar]
- 5.Michaud K, Messer J, Choi HK, Wolfe F. Direct medical costs and their predictors in patients with rheumatoid arthritis: a three year study of 7,527 patients. Arthritis Rheum. 2003;48:2750–2762. doi: 10.1002/art.11439. [DOI] [PubMed] [Google Scholar]
- 6.Dubois RW, Chawla AJ, Neslusan CA, Smith MW, Wade S. Explaining drug spending trends: does perception match reality? Health Affairs. 2000;19:231–239. doi: 10.1377/hlthaff.19.2.231. [DOI] [PubMed] [Google Scholar]
- 7.Crystal S, Johnson RW, Harman J, Sambamoorthi Kumar R. Out-of-pocket health care costs among older americans. J Gerontol: Social Sciences. 2000;55B:S51–S62. doi: 10.1093/geronb/55.1.s51. [DOI] [PubMed] [Google Scholar]
- 8.Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick G. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arth Rheum. 2007;56:1397–1407. doi: 10.1002/art.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sambamoorthi U, Shea D, Crystal S. Total and out-of-pocket expenditures for prescription drugs among older persons. The Gerontologist. 2003;43:345–359. doi: 10.1093/geront/43.3.345. [DOI] [PubMed] [Google Scholar]
- 10.Cohen S. MEPS Methodology Report No. 2. Rockville, Md: 1997. Sample design of the 1996 medical expenditure panel survey household component. AHCPR Pub. No 97–0027. [Google Scholar]
- 11.Helmick CG, Lawrence RC, Pollard RA, Lloyd E, Heyse SP. Arthritis and other rheumatic conditions: who is affected now, who will be affected later? National Arthritis Data Workgroup. Arth Care Res. 1995;8:203–211. doi: 10.1002/art.1790080403. [DOI] [PubMed] [Google Scholar]
- 12.Buchinsky M. Recent advances in quantile regression models. The Journal of Human Resources. 1996;33:88–116. [Google Scholar]
- 13.Korn FL, Graubard BI. Analysis of Health Surveys. New York: John Wiley & Sons; 1999. pp. 31–32. [Google Scholar]
- 14.Slaughter LM. Medicare Part D The Product of a Broken Process. NEJM. 2006;354:2314–2315. doi: 10.1056/NEJMp068116. [DOI] [PubMed] [Google Scholar]
- 15.Bach PB, McClellan MB. The first months of the prescription-drug benefit--a CMS update. NEJM. 2006;354:2312–4. doi: 10.1056/NEJMp068108. [DOI] [PubMed] [Google Scholar]
- 16.Nancy E, Morden NE, Garrison LP., Jr Implications of Part D For Mentally Ill Dual Eligibles: A Challenge For Medicare. Health Affairs. 2006;25:491–500. doi: 10.1377/hlthaff.25.2.491. [DOI] [PubMed] [Google Scholar]
- 17.US Department of Commerce Educational Attainment in the United States. Population Characteristics. Current Population Reports. 2003:P20–550. [Google Scholar]
- 18.McDonnell Kenneth J. Income of the Elderly Population, Age 65 and Over, 2004. EBRI Notes. 2006 January;27(1) [Google Scholar]
- 19.Cubanski J, Neuman P. Status Report On Medicare Part D Enrollment In 2006: Analysis Of Plan-Specific Market Share And Coverage. Health Affairs. 2007;26:w1–w12. doi: 10.1377/hlthaff.26.1.w1. [DOI] [PubMed] [Google Scholar]
- 20.Donohue JM, Frank RG. Estimating Medicare Part D's Impact on Medication Access Among Dually Eligible Beneficiaries With Mental Disorders. Psychiatr Serv. 2007;58:1285–1291. doi: 10.1176/ps.2007.58.10.1285. [DOI] [PubMed] [Google Scholar]