Skin contact of breast prostheses is considered by many to be a significant cause of ongoing subclinical infection leading to subsequent symptomatic capsular contracture (1–5). Many surgeons employ a no-touch technique, aiming to lower capsular contracture rates by eliminating skin contamination. One approach requires several assistants to hold retractors so that the implant can be inserted into the pocket without touching the skin (6). This is somewhat awkward and imprecise, and adds the expense of an additional assistant. Others have adopted a no-touch approach that uses a sterile tube or a simple anoscope acting as a sterile sleeve, which works quite well with a single assistant (7).
The present paper describes a surgical instrument designed for the insertion of breast prostheses. The instrument can be used quite safely and efficiently by a surgeon with one nurse assistant. It has enhanced illumination, enabling good hemostasis, and is particularly easy to make at low cost.
The casing of a 60 mL Toomey syringe is cut with a fine saw on an approximate 45° angle, and is used in both a long (100 mm) and short (66 mm) version (Figure 1). The tip is heat burnished with a butane torch to smooth the cut edges, and more importantly, to convert the plastic from opaque to clear. When used with a headlight, the translucent wide end of the syringe casing absorbs the light, and the clear tip, which is now within the dissected pocket, transmits the light with enhanced intensity. The amount of illumination is quite significant and beneficial, particularly when viewing the corners of a pocket with the longer casing, to ensure that there is good hemostasis (Figure 2). The shorter version works well for the insertion of the prosthesis.
Figure 1).
A 66 mm (top) and 100 mm (bottom) section of a 60 mL Toomey syringe that has been cut on a 45° angle
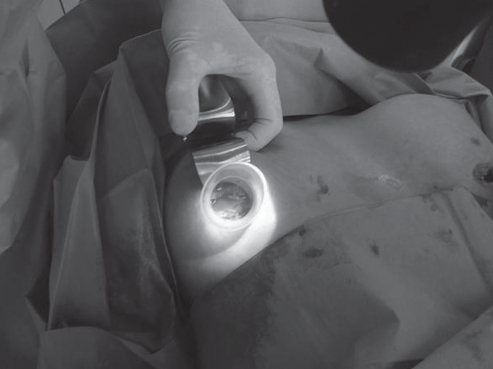
Figure 2).
After the tip has been heat burnished it becomes translucent, transmitting light with enhanced intensity
Once hemostasis is complete, the prosthesis, partially filled with 30 mL of normal saline, is simply folded and lubricated with Bacitracin (Pfizer Canada Inc) or saline (Figures 3 and 4). It is passed as a folded tube through the lumen of the shorter casing into the pocket. This is atraumatic for the prosthesis, and completely prevents any elements of contact between the prosthesis and the skin. We have used implants as large as 400 mL that, when filled with 30 mL of saline, can simply be folded and passed through without difficulty.
Figure 3).
The prosthesis is passed as a folded tube through the lumen of the shorter casing into the pocket, preventing any elements of contact between the prosthesis and the skin
Figure 4).
The prosthesis is completely within the pocket after passing through the lumen of the shorter casing
This device has many advantages over the anoscope because it transmits far more light, and its diameter fits into a 4.5 cm incision, which is quite acceptable for inframammary incisions. Its length can be determined by the surgeon’s preference. The author has not used this for axillary or periareolar incisions, but the principle to avoid the prosthesis skin contact should still exist.
A no-touch sleeve device’s ability to reduce the incidence of infection and subsequent capsule formation is a question that could only be resolved by a large randomized series, which has not been done to date. The advantage of this new device in ensuring hemostasis is a significant advantage in itself. It is low cost and reusable.
REFERENCES
- 1.Snell L, Brown M. Breast implant capsules and subclinical infection. Can J Plast Surg. 2008;16:125. (Abst) [Google Scholar]
- 2.Pajkos A, Deva AK, Vickery K, Cope C, Chang L, Cossart YE. Detection of subclinical infection in significant breast implant capsules. Plast Reconstr Surg. 2003;111:1605–11. doi: 10.1097/01.PRS.0000054768.14922.44. [DOI] [PubMed] [Google Scholar]
- 3.Netscher DT. Sublicinical infection as a possible cause of significant breast capsules. Plast Reconstr Surg. 2004;113:2229–30. doi: 10.1097/01.prs.0000123620.92330.bc. [DOI] [PubMed] [Google Scholar]
- 4.Pittet B, Montandon D, Pittet D. Infection in breast implants. Lancet Infect Dis. 2005;5:94–106. doi: 10.1016/S1473-3099(05)01281-8. [DOI] [PubMed] [Google Scholar]
- 5.Mladick R. Textured silicone breast implants. Plast Reconstr Surg. 2002;110:1201–2. doi: 10.1097/00006534-200209150-00053. [DOI] [PubMed] [Google Scholar]
- 6.Mladick R. “No-touch” submuscular saline breast augmentation technique. Aesth Plast Surg. 1993;17:183–92. doi: 10.1007/BF00636260. [DOI] [PubMed] [Google Scholar]
- 7.Dolsky RL. Inserting the Même prosthesis. Plast Reconstr Surg. 1984;73:466–8. doi: 10.1097/00006534-198403000-00026. [DOI] [PubMed] [Google Scholar]