Abstract
Improved treatment makes it easier for individuals with mental illness to participate in mainstream society, including the labor force. Nevertheless, a diagnosis of a severe and persistent mental illness or a substance use disorder often coincides with reduced work activity and lower earnings. The Social Security Disability Insurance Program and the Supplemental Security Income program provide income support for increasing numbers of individuals with mental illness. A growing share of a third program, Temporary Assistance for Needy Families, which offers cash support to low-income single caregivers, is composed of individuals with mental illness, as new work requirements result in faster exits of those without mental health conditions. These programs have come under increasing scrutiny as the shares of recipients with mental illness increase. Some question whether these programs serve many individuals capable of working and supporting themselves. However, evidence on whether eligibility criteria for these income support programs are too stringent or too lax regarding individuals with mental illness is mixed. Appropriate income support policy for those with mental illness will differ dramatically depending on the source of the recent rise in individuals with mental illness using income support.
Introduction
Disability awards due to mental illness are on the rise. Between 1987 and 2005, the share of Supplemental Security Income’s adult caseload disabled due to a mental disorder rose from 24.1% to 35.9%. Since the 1984 Disability Benefits Reform Act, the number of Social Security Disability Insurance awards due to mental illness has also increased substantially: in 1978, awards for mental illness were less than 2% of new awards; in 2005 (1), people with mental illness represented almost 30% of all beneficiaries.
Income support programs can create a disincentive to work, called moral hazard, which presents a challenge to setting eligibility criteria (2). Some analysts contend that rising disability awards for mental illness reflect a “broken” system that provides benefits to those who should not receive them (3); others point out that income support makes it easier for persons with mental illness to live in the community (4). These conflicting conclusions reflect an ongoing debate over whether increasing awards for mental illness represent a policy success because they reach needy individuals or failure because the increased awards reflect moral hazard (5). In this paper we review evidence on the issue of moral hazard and demonstrate that it is insufficient to conclude whether rising awards for mental illness represent a policy failure or success.
Background
U.S. policy toward the 26.2% of persons who meet diagnostic criteria for a mental or substance use disorder in a year (6) has shifted toward inclusion in mainstream society. Improved treatment of mental illness makes it possible for individuals to participate in society, including the labor force. Nevertheless, diagnosis of a severe and persistent mental illness is often associated with downward economic mobility. For example, the estimated reduction in annual earnings related to mental disorders ranges from 9.5% to 25% for males and from 12% to 29% for females (for a review, see Frank and Koss (7)).
Given the functional limitations associated with these disorders, affected individuals frequently apply for public income support. The Social Security Disability Insurance and the Supplemental Security Income programs provide monthly cash payments and medical benefits for individuals with who meet the program requirements for mental illness. In addition, an increasing share of adult recipients of the cash welfare program, Temporary Assistance for Needy Families, have mental health problems, in part because welfare exits for recipients without mental health problems have been more extensive since the 1996 welfare reform (8).
Supplemental Security Income is for low-income individuals who are over 65 years of age, blind, or disabled due to a disorder that prevents them from engaging in “substantial” work for at least 12 months or until death. To establish disability, there is a multi-stage screening process, requiring judgment calls about impairment and functioning. A minority of applicants are approved for disability benefits (9). In 2007, the monthly benefit for a single disabled person with no other income was $623.
The Social Security Disability Insurance program is a traditional social insurance program that replaces a portion of earnings when disability prevents “substantial gainful activity,” defined in 2007 as monthly earnings over $900. Only individuals who have contributed sufficiently to this program via payroll taxes can qualify for benefits. Given the early onset and inconsistent work history that accompany serious mental illness, few with mental illness qualify for full benefits. Social Security Disability Insurance and Supplemental Security Income have the same criteria for a disability and the same disability determination process. In 2006, the average monthly benefit was $978.
Changes in the late 1970s tightened eligibility criteria and made continuing disability reviews under both systems more rigorous. This policy was halted in 1984 following the removal of large numbers of recipients with mental disorders (one quarter of whom lost benefits due to these reviews), based on claims that the disability criteria had become too restrictive (4, 10). The criteria were restructured in the late 1980s to better address conditions such as mental disorders and chronic pain.
Many individuals with symptoms of mental disorders use Temporary Assistance for Needy Families. Historically, policymakers and researchers assumed that welfare recipients were “able and expected to work” and that disability programs would serve those unable to work. As a result, the 1996 welfare reform that instituted new work requirements did not anticipate an emerging policy problem—that caseloads include impaired welfare recipients who have difficulty working steadily. Because their impairments often do not meet Supplemental Security Income’s disability criteria, many find themselves without either work or cash assistance.
Mental Illness and Income Support
An ongoing difficulty with determining impairment for those with mental disorders is that mental disorders are heterogeneous. Some individuals may meet diagnostic criteria for a severe disorder without having significant impairments in functioning (4, 11), and other individuals with “mild” diagnoses suffer functional limitations that impede their ability to work. Impairments can be temporary or persistent, and can improve and recur. Supplemental Security Income, Social Security Disability Insurance, and Temporary Assistance to Needy Families were not designed with this heterogeneity in mind. In addition, because no simple test can fully assess illness, impairment, and disability, the nature of mental disorders complicates eligibility determination.
Income support programs protect people against health and injury risks that threaten the ability to work and earn a living. To reduce moral hazard, these programs have stringent eligibility requirements, time-limited benefits, and relatively low benefit levels. To qualify for benefits, individuals must show that they are unable to undertake substantial gainful activity. However, recent changes in program rules that are intended to encourage work ignore characteristics of mentally ill participants. As a result, some who are mentally disabled, but only partially able to work, may lose benefits and find themselves with inadequate earnings if they do work.
The work requirements of Temporary Assistance for Needy Families also do not recognize the unique needs of recipients with mental illness. The 2006 reauthorization of the program increased the hours of work required, effectively increased the share of recipients expected to work in each state, and ended states’ ability to count mental health treatment activity toward work requirements.
Moral Hazard in Mental Disorder Disability Awards
As the share of recipients with mental disorders has increased, program eligibility rules and the disability determination process have been questioned. Because determining disability due to mental disorders requires professional judgment rather than formulaic assessments, the potential for false negative and false positive eligibility errors increases.
Federal programs attempt to minimize moral hazard, or false positive errors. Applicants must supply ample documentation of disability. Only one third of initial applications are accepted; even after appeals, most applicants are not awarded benefits (12). The continuing disability review process, even after the 1984 liberalization, terminates benefits for 8% to 12% of Supplemental Security Income and Social Security Disability Insurance beneficiaries each year (13).
Rejected applicants in the labor force
Several studies document that 20% to 40% of rejected applicants for SSDI later work (14–16). This has been interpreted by Autor and Duggan (2006) as clear evidence of moral hazard. We conclude, in contrast, that an equally compelling statistic is the 60% to 80% of rejected applicants who do not subsequently work. Of course, some of these individuals may choose not to work while they appeal their disability eligibility, and others may fail to work due to low skill rather than a health-related disability. However, existing evidence is no more likely to show that moral hazard exists than it is to document that most rejected applicants needed them.
Increasing awards
Some analysts contend that increased disability awards based on mental illness is an indicator of moral hazard or a problem with the disability determination process. Specifically, Stapleton and colleagues (17) analyzed Supplemental Security Income caseload growth during the 1990s. They found that demographic and labor market factors could explain most of the rise in applications for most medical conditions, but far less of the increased applications based on mental disorders. They conclude that the Supplemental Security Income criteria for mental disorders had been expanded.
We do not accept this conclusion because the authors compare the 1990s growth in applications with application rates during the 1980s, when the Reagan administration disproportionately terminated people with mental illnesses from the rolls. A reduction in applications at that time could be expected independent of other factors, so it is not an appropriate baseline for comparison.
Application rates and unemployment
Some analysts suggest that the relationship between applications and unemployment rates indicate that many workers seek public benefits not because of a disabling mental illness, but because they have been laid off (3). An increase in applications does not equal a rise in awards.
Social Security Disability Insurance
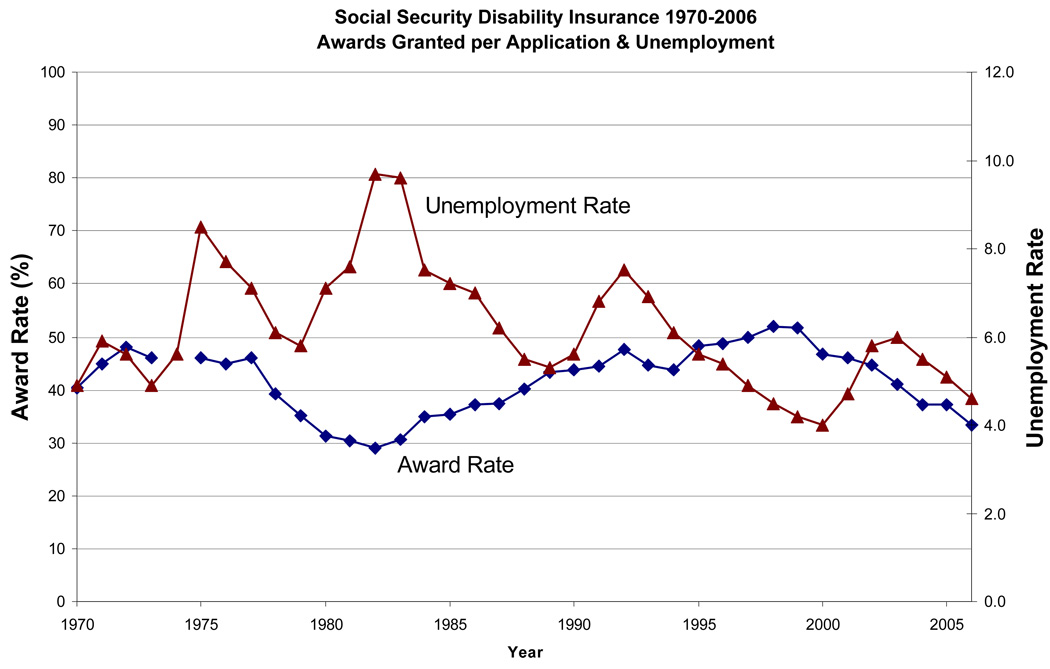
Social Security Disability Insurance awards have increased due to both mental illnesses and musculoskeletal disorders (3, 17). A 2003 study found that Social Security Disability Insurance applications increased more with employment crises in the 1990s than in the mid-1980s (18). In concluding that abuse of Social Security Disability Insurance has “reached unsustainable levels so that the Social Security Disability Insurance screening process is broken,” Autor and Duggan (2006) invoke the cyclicality of Social Security Disability Insurance applications, the fall in application rejection rates, and the rise in awards for disabilities with low mortality rates, such as mental impairment and musculoskeletal disorders. Although Social Security Disability Insurance applications moved closely with unemployment rates over the 1990s, the award rate for applications is counter-cyclical over the entire 1970–2006 period (Figure 1). In other words, stringent eligibility criteria limit the cyclicality in award rates.
Figure 1. Social Security Disability Insurance 1970–2006: Awards Granted per Application & Unemployment Rates.
Sources: Unemployment data refer to the population 16 and older and come from the Bureau of Labor Statistics. Award numbers are from Social Security Administration annual statistical supplement to the Social Security Bulletin, various years. Population estimates come from the U.S. census and refer to ages 25–64
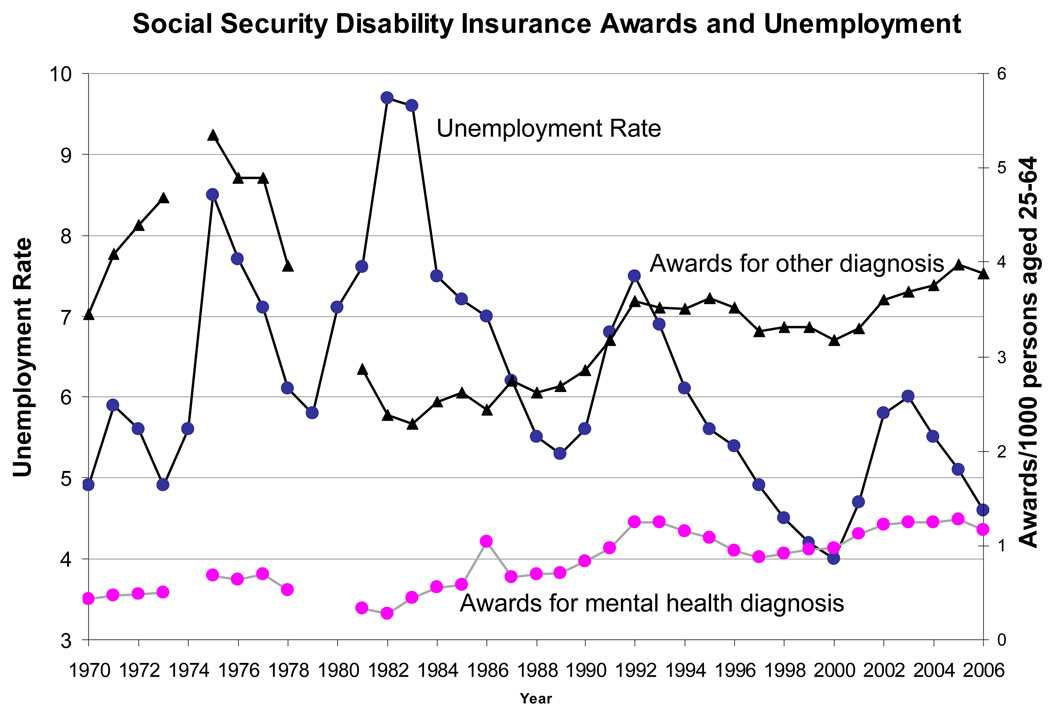
In addition, the trends in Social Security Disability Insurance awards per population (vs. application) do not show any clear relationship to the unemployment rate, especially after the 1970s. This is true for both mental and non-mental disorders which drift upward slowly after the mid-1980s (Figure 2). On the basis of these trends, we find no evidence for the contention that moral hazard is somehow more serious for disability awards related to mental illness.
Figure 2. Social Security Disability Insurance 1970–2006: Awards Granted per Population & Unemployment Rates.
Sources: Unemployment data refer to the population 16 and older and come from the Bureau of Labor Statistics. Award numbers are from Social Security Administration Annual Statistical Supplement to the Social Security Bulletin, various years. Population estimates come from the U.S. census and refer to ages 25–64
Supplemental Security Income
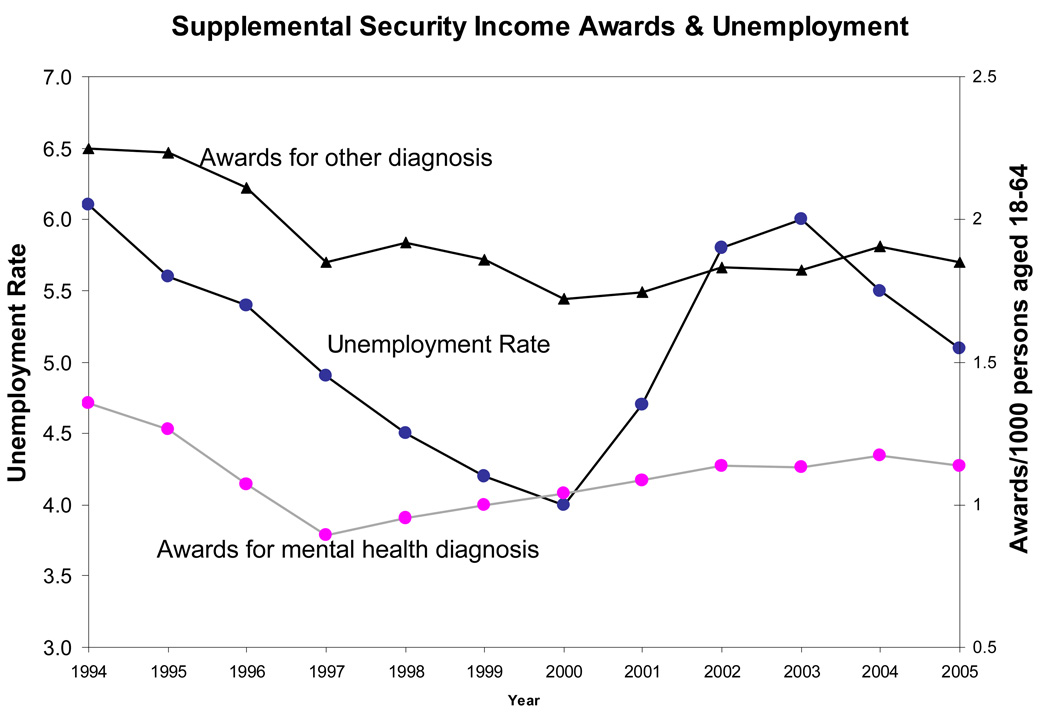
The recent relationship between Supplemental Security Income award rates for adults with mental disorders and the unemployment rate is not consistent with a moral hazard explanation that posits that disability awards for mental illness are counter-cyclical, as they are for unemployment insurance. From 1992 to 2006, unemployment fluctuated widely, falling from 7 to 4 percent before rising and falling dramatically again. However, Figure 3 shows no consistent trend in Supplemental Security Income award rate for mental disorders in relation to unemployment. Awards for non-mental disorders follow a similar trend.
Figure 3. Supplemental Security Income 1994–2005: Awards Granted per Population & Unemployment Rates.
Sources: Unemployment data refer to the population 16 and older and come from the Bureau of Labor Statistics. Award numbers are from Social Security Administration annual statistical supplement to the Social Security Bulletin, various years. Population estimates come from the U.S. census and refer to ages 18–64. Exact awards for mental disorders prior to 1994 are not currently available.
Fate of rejected applicants
The challenge of determining disability due to mental illness means that some truly needy applicants are denied benefits. If this is the case, rejected applicants will have worse outcomes than those determined to be disabled. We gain some insight into the extent of moral hazard vs. false negatives using data from about 500 women surveyed by the Women’s Employment Study (19). We contrast the housing stability, work activity, and welfare experiences of WES respondents who applied for and received Supplemental Security Income benefits to women who applied for but did not receive these benefits (data not shown).
In 1997, 36% of respondents met the diagnostic screening criteria for major depression, post-traumatic stress disorder or generalized anxiety disorder. We did not have the statistical power to analyze the 36% of the sample with identified mental illness, but among the 12% of the overall WES sample who received disability benefits at any time between 1997 and 2003, 30% had been evicted or experienced homelessness at some point during the study, similar to the 28% for those who had never applied for nor received benefits. By contrast, among the 26% of respondents whose Supplemental Security Income applications were not approved by the 2003 interview, 43% experienced housing instability, suggesting that they were in need of benefits. The rejected applicants were only half as likely to be working in 2003 as those who never applied for disability—43% vs. 79%. They also worked much less over the six-year period—in 26% of the 72 months vs. 63%. These data are inconsistent with the basic moral hazard hypothesis.
Discussion
Why are disability awards for mental disorders increasing, if not moral hazard or a loosening of eligibility criteria? The current focus on moral hazard is misplaced if, for example, the mental disorder caseload reflects shifting labor markets from manufacturing toward services, where jobs may require different emotional and mental skills.
Our analyses of the unemployment, application, and award rates cast doubt on prior claims that public income support programs are being used as a form of unemployment insurance. Our evidence does not permit definitive conclusions either supporting or refuting the role of moral hazard as a determinant of recent caseload increases for mental disorders, but it does highlight the need for additional information on the role of moral hazard in the these programs.
People with mental illnesses disproportionately rely on public income support programs. It remains unsettled whether eligibility polices appropriately match people and programs, and whether program policies can be redesigned to help those with mental illness engage in work when possible. Given the increasing share of mentally ill people among Supplemental Security Income, Social Security Disability Insurance and Temporary Assistance to Needy Families recipients, it is important to understand how these programs might be modified to better serve those with mental disorders.
Acknowledgments
This paper was prepared for and presented at the John D. and Catherine T. MacArthur Foundation Network on Mental Health Policy Research Conference in Miami Beach, FL (May 9–10, 2007). The authors gratefully acknowledge funding from the John D. and Catherine T. MacArthur Foundation Network on Mental Health Policy Research. Drs. Frank and Meara also acknowledge research support from NIDA grants DA10233 and DA019485.
References
- 1.Social Security Administration: Annual Statistical Report on the Social Security Disability Insurance Program, 2007. 2008. [Google Scholar]
- 2.Barr N. Economic Theory and the Welfare State: A Survey and Interpretation. Journal of Economic Literature. 1992;30(2):741–803. [Google Scholar]
- 3.Autor DH, Duggan MG. The growth in the social security disability rolls: a fiscal crisis unfolding. The Journal of Economic Perspectives. 2006;20:71–96. doi: 10.1257/jep.20.3.71. [DOI] [PubMed] [Google Scholar]
- 4.Frank RG, Glied S. Better But Not Well: Mental Health Policy in the United States Since 1950. Baltimore, MD: The Johns Hopkins University Press; 2006. [Google Scholar]
- 5.Burkhauser RV. In: Summing Up: Reflections on the Past and Future of Disability Policy, in Growth in Disability Benefits. Rupp K, Stapleton DC, editors. Kalamazoo, MI: Upjohn Institute for Employment Research; 1998. [Google Scholar]
- 6.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frank RG, Koss C. Mental Health and Labor Markets Productivity Loss and Restoration, in Disease Control Priorities Project. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 8.Meara E, Frank RG. NBER Working Paper Series. Cambridge, MA: 2006. Welfare Reform, Work Requirements, and Employment Barriers. [Google Scholar]
- 9.Daley MC, Burkhauser RV. In: The Supplemental Security Income Program, in Means Tested Transfer Programs in the United States. Moffitt R, editor. Chicago, IL: University of Chicago Press for the NBER; 2003. pp. 79–140. [Google Scholar]
- 10.Grob GN, Goldman HH. The Dilemma of Federal Mental Health Policy. Piscataway: Rutgers University Press; 2006. [Google Scholar]
- 11.Regier, Narrow: 2002. [Google Scholar]
- 12.Social Security Administration: Annual Statistical Supplement, 2007. 2007. [Google Scholar]
- 13.U.S. Social Security Administration: Trends in the Social Security and Supplemental Security Income Disability Programs, 2004. [Google Scholar]
- 14.Bound J. The health and earnings of rejected disability insurance applicants. American Economic Review. 1991;81:1427–1434. [PubMed] [Google Scholar]
- 15.Bound J, Burkhauser RV, Nichols A. Tracking of household income of SSDI and SSI applicants. Ann Arbor: University of Michigan Retirement Research Center; 2001. [Google Scholar]
- 16.Chen S, van der Klauuw W. The work disincentive effects of the disability insurance program in the 19902. Journal of Econometrics. 2008;142:757–784. [Google Scholar]
- 17.Stapleton D, Coleman K, Dietrich K, Livermore G. In: Empirical analyses of Social Security Disability Insurance and Supplemental Security Income application and award growth, in Growth in Disability Benefits: Explanations and Policy Implications. Rupp K, Stapleton DC, editors. Kalamazoo, MI: Upjohn Institute for Employment Research; 1998. pp. 31–80. [Google Scholar]
- 18.Autor DH, Duggan MG. The Rise in the Disability Rolls and the Decline in Unemployment. The Quarterly Journal of Economics. 2003;118(1):157–206. [Google Scholar]
- 19.Danziger S, Corcoran M, Danziger S. In: Barriers to the Employment of Welfare Recipients, in Prosperity for All? The Economic Boom and African Americans. Cherry R, Rodgers W, editors. New York: Russell Sage Foundation; 2000. pp. 245–278. [Google Scholar]