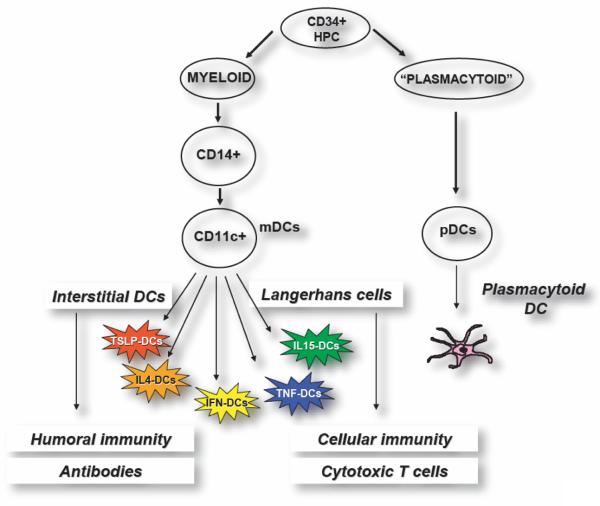
Figure 1. Subsets of human dendritic cells.
Blood DCs, mobilized by FLT3 ligand, contain both CD11c+ myeloid DCs (mDCs) and plasmacytoid DCs (pDCs). mDCs can be generated by culturing CD34+ HPCs with GM-CSF and TNF. In this way, two DC subsets can be obtained: Langerhans cells (LCs) that are specialized in the induction of cellular immunity including generation of cytotoxic T cells, and interstitial DCs that are specialized in launching humoral immunity and antibody response. Most studies of DCs so far have been carried out with DCs made by culturing monocytes with GM-CSF and IL-4, a simple procedure that yields a homogenous population of DCs. These preparations contain cells that resemble interstitial DCs and are devoid of LCs due to transcriptional regulation of Langerin expression by IL-4. These DCs are immature and require exogenous factors for maturation. Replacement of IL-4 with other cytokines leads to generation of a “Rainbow” of mDCs whose composition and function is determined by cytokine to which monocytes are exposed. Thus, in combination with GM-CSF, thymic stroma lymphopoietin (TSLP) generates mDCs promoting type 2 immunity while TNF and IL-15 generate mDCs containing LCs. The role of pDCs in vaccination against cancer remains to be determined. However, in the human these cells are likely to be the target of CpG since they uniquely express TLR9. Their capacity to rapidly secrete high amounts of type I IFN might contribute to anti-tumor activity of CpG.