Abstract
The purpose of this case study was twofold: 1) to illustrate the use of a treatment-based classification (TBC) system to direct the early intervention of a patient with mechanical neck pain, and 2) to show the progression of this patient with multimodal-modal intervention. The patient exhibited axial neck pain with referral into her upper extremity. Her pain peripheralized with cervical range of motion and centralized with joint mobilization placing her primarily in the centralization category. Her poor posture and associated muscle weakness along with the chronicity of symptoms placed her secondarily into the exercise and conditioning group resulting in a multi-modal treatment as the patient progressed. Although the design of this case report prevents wide applicability, this study does illustrate the effective use of the TBC system for the cervical spine as captured by accepted outcomes measures.
KEYWORDS: Multi-Modal Intervention, Neck Pain, Treatment-Based Classification
Mechanical neck pain commonly arises insidiously1 and is generally multifactorial in origin, including one or more of the following: poor posture, anxiety, depression, neck strain, and sporting or occupational activities2,3. In an estimated 50–80% of cases involving back or neck pain, an underlying pathology cannot be definitively determined4. Regardless of the primary source of pain, the prognosis for individuals experiencing chronic neck pain is poor, as many patients continue to suffer from persistent pain and disability following conservative physical therapy intervention5,6. Chronic neck pain appears to be more persistent than low back pain7, and it is second only to lumbar pain as the causal factor for time missed from work.
Despite the prevalence, less-than optimal prognosis, associated risk of disability, and economic consequences of individuals suffering from mechanical neck pain, there remains a significant gap in the literature, which fails to provide sufficient, high-quality evidence to effectively guide the conservative treatment of this patient population8. This lack of quality evidence largely stems from the poorly understood clinical course of neck pain in conjunction with the inconclusive results related to the efficacy of commonly used interventions2,9,10. Left with poorer quality trials as a guide, Physical Therapists approach the management of this pathology with a plethora of interventions such as manual therapy (MT), therapeutic exercises, manual/mechanical traction, modalities, massage, and functional training5,10–12.
One reason the outcomes in the PT literature may be less than impressive is that many of the studies looking at conservative treatments for the management of neck pain use a heterogeneous subject population13. Many studies also combine some or all of the following clinical manifestations into the same case mix during clinical trials: acute whiplash, subacute and chronic mechanical disorders, and chronic cervical headache. The identification of a homogeneous patient population would likely enhance the potential to initiate targeted interventions and to specifically assess treatment responses14. One solution to acquiring more homogeneous patient populations is the use of treatment-based classification (TBC) systems.
Classification systems are developed with the intent of both directing treatment and improving clinical outcomes by identifying detailed combinations of treatments that specifically benefit a subgroup of patients presenting with certain characteristics5,15. The principle supporting classification systems centers around the following notion: a decrease in uncertainty concerning appropriate, effective treatments could be observed via the linkage of an impairment diagnosis to a treatment choice16. Classification systems can also serve to improve clinical research by identifying evidence-based practice patterns for specified subgroups of patients5. The goal of this model is to heighten decision-making abilities of clinicians in relation to intervention strategy and prognosis16.
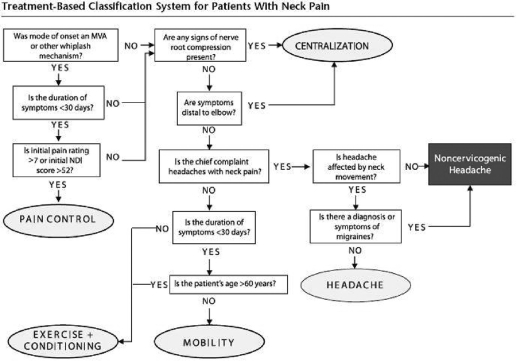
While the classification-based strategy has been shown to yield optimal outcomes for the lumbar spine17–20, comparatively nominal research has been performed to investigate patient outcomes using a similar classification-based approach for the cervical spine5,16. Despite this preliminary work, research has not served to confirm the validity of such a system5. One recent study reported a 98% between-raters percentage agreement with the use of a proposed treatment-based classification (TBC) system (Figure 1)5. This indicates that the algorithm could be applied consistently by different examiners who are considering the same patient data. With intent to assist in the validation of the outcomes using the aforementioned strategy, the purpose of this case study is to describe the use of a TBC system approach in the management of a single patient with mechanical neck pain and referred pain into the arm.
FIGURE 1.
Proposed classification decision-making algorithm.5 MVA= motor vehicle accident, NDI = Neck Disability Index. Used with permission.
Patient Characteristics
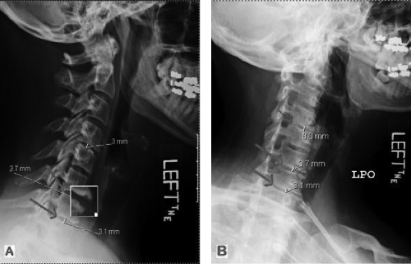
The patient was a 51-year-old female software business analyst entering the Physical therapy (PT) clinic with a chief complaint of left-sided neck pain that radiated into her ipsilateral shoulder and arm, descending to her elbow. She had consulted an orthopedic surgeon approximately 1 month prior to the initial physical therapy examination. At that time, plain radiographs of the cervical spine were ordered and were judged to be abnormal. The lateral view x-rays revealed cervical degenerative changes primarily at C6–C7 as well as at C7–T1 and secondarily at C4–C5 (Figure 2). A copy of these films was obtained by the physical therapist for observation and verification. The patient was then placed on a 1-week trial of oral steroids. The steroids temporarily provided relief of her symptoms, but after discontinuing the steroids, the patient returned to her previous level of pain the following week followed by a steady worsening of symptoms. Approximately 3 weeks following the failed steroid trial, the patient was seen by a second orthopedic surgeon who referred her to physical therapy for 3–4 weeks with the diagnosis of degenerative disc disease (DDD) of the cervical spine. She had not received any previous trials of PT for her cervical spine. The patient's past medical history was negative for disease and for medical red flags indicative of a systemic pathology.
FIGURE 2.
(A) Conventional radiograph (lateral view) portraying an increased lordotic curvature and (B) with cervical spine positioned in neutral, revealing disc degeneration primarily at C6–C7 and C7–T1 (large arrows) and secondarily at C4–C5 (small arrows). The presence of osteophytes at C6–C7 are magnified in (A) and demarcated by the arrow in (B).
Examination
At the time of her first visit, the pain, present for 7 weeks, was constant and was more predominant in her shoulder and along the posterior aspect of her upper arm. Her pain, described as sharp or pinching, varied in intensity from 4/10 to 10/10 (10 representing worst imaginable pain) in a 24–hour period and was activity-dependent as well as position-dependent. Specifically, the intensity of the pain was nominal in the mornings and steadily worsened with prolonged sitting or standing. Her symptoms were only relieved completely by lying supine or on her side. The patient's symptoms were exacerbated by almost any task performed in a sitting or standing position. This was unfortunate since her job required her to sit for the majority of the day and even driving to work caused debilitating pain. She reported functional limitations with movements requiring her to elevate her left arm. She was able to continue her regular exercise program consisting of walking on the treadmill for 2–3 miles, approximately 5 times per week, but did experience pain and discomfort.
The Neck Disability Index (NDI), the Short Form 12 (SF-12), and Single Alphanumeric Estimate (SANE)21 are self-reported measures administered at baseline and regularly thereafter to objectively measure the patient's progress. The NDI is a condition—as well as a region-specific self-report instrument for the measurement of neck pain and disability, which has been found to be both valid and reliable in patients with neck pain5,22–24. Consisting of 10 items, 7 pertaining to ADLs, 2 related to pain, and 1 related to concentration, the NDI has been shown to have a high degree of test-retest reliability and strong construct validity25 as well as internal consistency23,24,26,27. Research has found the test-retest reliability of the NDI to be moderate (ICC of 0.68)22,23 and the internal consistency to be high (alpha = 0.80–0.92)28. With reported minimal detectable changes (MDC) of 5.029, 8.05,30, and 10.222, and minimally clinically important differences (MCID) of 7.022,26 and 5.018, the NDI is calculated as a percentage with higher scores corresponding to greater disability22. Scores of 10–28% constitute mild disability, 30–48% indicate moderate disability, 50–68% indicate severe disability, and 72% or greater signify complete disability. On initial examination, the patient's NDI score was 52%.
The SF-12 is a 12-item self-administered questionnaire that yields scores for the following 8 areas associated with quality of life, including physical functioning, physical problems, social functioning, bodily pain, general mental health, emotional problems, vitality, and general health perceptions25. Two summary scores (each ranging from 0 to 100) are obtained: a mental component score (MCS) and a physical component score (PCS). In the general population, the mean score is approximately 50. Scores of 40–49 indicate mild disability, 30–39 are indicative of moderate disability, and scores below 30 indicate severe disability in quality of life25,31.
The SANE is an outcome measure used to record the patient's self-reported function on a scale from 0–100 and has been shown to correlate well with established outcomes measures in the knee21 and the shoulder32. The MDC and MCID have not been established for the SANE. The patient was asked to rate her function on a 0–100% scale, with 100% representing her level of function prior to the onset of neck pain and 0% being indicative of no functioning. At initial evaluation, the patient reported she was 60% of her normal functioning, which seemed to correlate well with the NDI in this patient at baseline.
The physical examination consisted of postural assessment, neurological screening, cervical/thoracic/shoulder joint active range of motion (AROM), segmental mobility testing of cervical/thoracic spine, and examination of scapulothoracic muscle strength.
Observation/Posture
Posture was analyzed in sitting from frontal and sagittal plane views, as described by Kendall et al33. From a sagittal view, the patient was found to exhibit excessive rounded shoulders (shoulder protraction) defined as an anteriorly deviated acromion compared to the lumbar spine. Forward head posture was also noted by the identification of the external auditory meatus located anteriorly to the lumbar spine34. In addition, the patient presented with thoracic kyphosis (Figure 3). There was no notable scapular winging or atrophy of the posterior scapular musculature.
FIGURE 3.
(A) Postural assessment at initial visit reveals patient's excessive rounded shoulders and forward head posture. (B) Depicts the patient's improved cervical and thoracic posture at 10 weeks following initial evaluation.
Shoulder Screen
The use of overpressure serves to rule out potential joints that do not contribute to the patient's impairment and is also useful in isolating specific impairments35,36. Shoulder active range of motion (AROM) with overpressure into all directions failed to elicit any of the patient's symptoms. Therefore, the shoulder was cleared as a possible source of the patient's referred symptoms.
Cervical ROM
Cervical AROM was measured with the patient in sitting, using a universal goniometer. Good to high reliability has been reported with AROM measurements, when taken by the same therapist, regardless of the use of a goniometer versus a cervical range-of-motion (CROM) instrument37. On first visit, the patient was limited by 3–4 finger widths into cervical flexion. Active movements into cervical extension (34°), bilateral side flexion (16° right and 20° left), and bilateral rotation (35° right and 37° left) were all limited. Active movements into cervical flexion, extension, side flexion bilaterally, and rotation bilaterally reproduced the patient's neck and left arm pain.
MMT
The clinical decision to defer formal manual muscle testing of the cervical spine in this case was influenced by the patient's rising pain level. Assessment of scapulothoracic musculature yielded the following: 3−/5 bilateral lower traps, 3−/5 bilateral middle traps, and 3+/5 bilateral rhomboids. Muscle weakness of the deep neck flexors was assumed since the patient had a forward head posture (Figure 3). According to theory, with this posture, the following muscles are placed in a lengthened position and thus develop weakness: cervical spine flexors, thoracic spine extensors, middle trapezius, and lower trapezius6,33.
Neurological Screening
All upper extremity sensation (dermatomes) was found to be grossly intact. Biceps, brachioradialis, and triceps reflexes were all found to be equal and unremarkable bilaterally. Testing of cervical spine myotomes was unremarkable.
Joint Segmental Mobility (Passive Accessory Movements)
The use of accessory movements, when used with intention to isolate the concordant sign, have been shown to be reliable and clinically useful38. Such assessment strategies have demonstrated 100% accuracy in isolating the guilty segmental level of pathology38. Accessory joint motions in the form of central posterior-anterior (CPAs) and unilateral posterior-anterior (UPAs) as described by Maitland and colleagues39 were performed at levels C2–T1 with patient in prone position. During these mobilizations, C6–C7 elicited the patient's chief complaint, and repeated UPAs to C4–C7 on the left side reduced symptoms slightly.
Special Tests
We attempted to rule in cervical radiculopathy with the use of the clinical prediction rule (CPR) developed by Wainner et al40 This CPR consists of 4 tests: cervical rotation less than 60°, upper-limb tension testing, distraction, and Spurling's test. Our patient demonstrated a positive test of rotation less than 60°, a positive Spurling's test, and a negative upper limb tension test, whereas the distraction test producing an equivocal result. Since at least 3 of 4 of these findings must be present for cervical radiculopathy to be strongly suspected16, we took the findings of a negative-upper limb tension test as sufficient to rule out cervical radiculopathy16.
Clinical Impression
Based on the examination, we hypothesized that the patient's DDD and subsequent impaired cervical spine mobility were primary contributors to her symptoms. Her poor posture and ergonomics further exacerbated her symptoms. The examination results were consistent with the imaging, indicating that the C6–C7 levels were most affected. The presentation of symptoms was suggestive of a referred pattern of pain from her lower cervical spine. The working diagnosis was cervical spine somatic referred pain. This subtype of referred pain typically presents as a deep, dull, aching pain with a proximal to distal distribution41 and may be generated from a variety of structures including ligaments, capsule, and annulus42. Specifically, Slipman et al43 have shown with discography that the C6–7 intervetebral disc refers pain into the upper extremity. The variety of potential sources of pain in addition to the concept of interneuronal convergence41, (i.e., that one interneuron in the spinal cord receives input from numerous motor and sensory nerves), can yield pain patterns that do not follow a predictive dermatomal pattern42,44.
More importantly, the peripheralization of symptoms with motion testing, the age of the patient, and the duration of symptoms place this patient primarily into the centralization classification16. The associated muscle weakness due to chronic postural impairments, deconditioned state of the patient in general, and the longer duration of symptoms placed this patient secondarily into the conditioning group, provided we could further centralize her symptoms first. Placement into a specific category is not mutually exclusive, rather, patients are expected to shift from one classification to another during an episode of care as their clinical presentation changes and they progress through a course of treatment16.
Intervention
The patient was seen in physical therapy approximately once a week for 10 visits over the course of 13 weeks with session durations of 30–60 minutes. Each physical therapy session involved obtaining relevant subjective information, re-assessing significant impairments, treatment, and post-treatment re-evaluation to assess the patient's response to treatment. The patient was educated regarding the diagnosis, resulting primary and secondary impairments, intended interventions, and plan of care. Functional goals were also established and discussed. Progression of exercises was based on the continual re-assessments including reports of pain, and the patient's reported ease or difficulty in performing her home exercise program.
Phase I interventions were consistent with those established in the TBC system and consisted predominantly of manual cervical traction and cervical retraction exercises. Additionally, the patient was thoroughly educated regarding both posture and activity modifications. Postural education is frequently implemented in an attempt to decrease abnormal mechanical stressors placed on the cervical spine45. Given the patient's occupation, a considerable amount of time was dedicated to discussing the importance of the maintenance of proper spinal alignment while typing at a computer for 8 hours/day. Research has associated positive outcomes when postural advice is provided to patients with the treatment goal of centralization16. Individuals experiencing chronic, non-severe neck pain have a diminished ability to maintain an upright, neutral posture when distracted by a 10-minute computer task46. Given this fact, the implementation of regularly scheduled rest breaks throughout the day was strongly recommended. UPAs to the left of C4–C7 were also performed due to the demonstrated ability (in the initial exam) to decrease the patient's symptoms. Following the administration of both cervical traction and UPAs, the patient typically reported a decrease in her pain to as little as 0/10. Past publications have advocated that PA mobilizations are effective in pain reduction42,47. Finally, the patient received suboccipital release for approximately 5 minutes while in the supine position. This form of soft tissue mobilization serves to decrease the tightness and hyperactivation in the shortened deep neck extensor musculature as a result of the patient's characteristic forward head posture6.
As the patient's pain became more centralized and lessened to 0/10, Phase II commenced with a greater emphasis on therapeutic exercises as indicated in the exercise and conditioning classification. Strengthening exercises for the neck consisted of deep cervical flexor strengthening5,16. The deep cervical flexors include the longus coli, longus capitus, rectus capitis anterior, and rectus capitis lateralis, which function in a dynamic fashion to support the neck when it is in neutral or mid-range postures that commonly occur during functional daily activities48. These exercises are low-load, therapeutic exercises focusing on motor control rather than muscle overload49. In addition to neck strengthening, exercises for the upper quarter were initiated with emphasis placed on strengthening the middle and lower trapezius as well as the rhomboids as indicated by Kendall et al33. Finally, prolonged (at least 1 minute), low-load cervical and upper quarter stretching was incorporated into the Phase II program. The incorporation of stretching exercises into an home exercise program was found to considerably decrease neck pain and disability in women suffering from non-specific neck pain12.
Outcomes
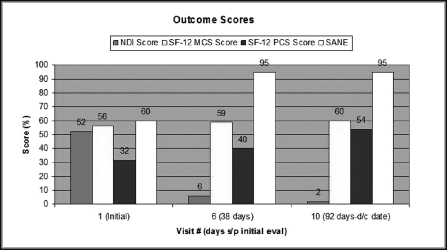
The patient's progress with regard to impairments (Table 1) and function (Figure 4) is obvious. By Week 3, the patient reported no (0/10) pain during the day, but she still experienced increased pain in the evenings. At 6 weeks (38 days) status post-initial evaluation, the patient remained pain-free throughout the entire day and was off all pain medication. Her referred pain symptoms extending into her left arm distally to the elbow were no longer present by Week 6. She also demonstrated improvements in cervical ROM concurrent with the reduction of symptoms. The patient's NDI score dramatically improved from 52% (severe disability) to 6% (no disability) over the course of 6 weekly physical therapy sessions. At roughly the same time, the patient also presented with clinically significant changes in her perceived level of function (SANE), and both subscales of the SF-12. The SANE, initially reported at 60%, drastically improved to 95% at 6 weeks post-initial evaluation.
TABLE 1.
Impairment measurements taken at visits 1, 6, and 10.
| Visit # | Active Movement | ROM | Associated Complaints |
|---|---|---|---|
| 1 | Flexion | 3–4 finger widths | Pain rating 4/10 to 10/10 |
| Extension | 34° | All motions reproduce sharp neck and L arm pain | |
| Side flexion right | 16° | ||
| Side flexion left | 20° | ||
| Rotation right | 35° | ||
| 6 | Rotation left | 37° | |
| Flexion | 1–2 finger widths | Pain rating 0/10 | |
| Extension | 41° | Complaints of stiffness and fatigue in cervical spine | |
| Side flexion right | 22° | ||
| Side flexion left | 24° | ||
| Rotation right | 50° | ||
| Rotation left | 56° | ||
| 10 | Flexion | 1–2 finger widths | Pain rating 0/10 |
| Extension | 54° | Cervical spine tightness at end-range | |
| Side flexion right | 29° | ||
| Side flexion left | 27° | ||
| Rotation right | 38° | ||
| Rotation left | 31° |
FIGURE 4.
Results of outcome scores administered at initial visit followed by visit 6 and visit 10. The Neck Disability Index (NDI) score represents improved function as the score lessens. The Single Alphanumeric Estimate (SANE) and the Short Form 12 (SF-12) mental component score (MCS) and physical component score (PCS) represent improved function as the score increases. All scores are in percentages.
Discussion
The favorable outcomes observed in this case are consistent with the preliminary results of Fritz and Brennan5, and Childs and colleagues16. The recently proposed TBC system for the management of neck pain classifies patients based on the integration of subjective history and physical examination into 1 of 5 categories5. The placement of the patient into the appropriate classification(s) dictates the treatment strategies by providing a set of matched interventions. Fritz and Brennan5 revealed that those receiving matched interventions demonstrated greater changes in both the NDI and pain rating scores. This was also the case with our single subject.
Despite the prevalence of mechanical neck pain, a large gap exists in the literature, which has failed to provide sufficient, conclusive evidence favoring one specific intervention over another in the conservative treatment of this pathology. The inconsistencies that currently exist among therapists regarding treatment techniques can be largely attributed to this lack of conclusive evidence. The current trends in research support the use of manual therapy in combination with exercise16,20,50. Based on the literature and current practice patterns, there appears to be a cohort of individuals with neck pain who respond favorably to the combination of mobilization/manipulation, exercise, and possibly traction interventions16. A recent study performed by Cleland and colleagues, which included patients with cervical radiculopathy34 reported drastic reductions in disability following a conservative management strategy that included intermittent cervical traction, manual therapy, and deep neck flexor muscle strengthening. Although there is a role for therapeutic exercises in the treatment of chronic mechanical neck disorder, the relative benefit of individual exercises has not been clearly established20.
Research has suggested benefits from the use of CPAs/UPAs as treatment techniques when centralization is observed16. In addition, the literature has established a strong association between deep neck flexor weakness and neck pain, warranting strengthening of these muscles for those with neck pain and poor posture48,49. However, further research is needed on many interventions such as repeated movements and traction, which have not been proven to be effective but which are frequently used with the intent of symptom centralization16.
The available trials on neck pain further complicate the issue as they are highly variable in methodological quality, study populations, interventions, reference treatments, dosage parameters, and outcome measures15,51,52. All of these inconsistencies further contribute to the conclusion that no one treatment type can be favored over another51. These inconclusive results also indicate that patients with neck pain consist of a variety of subgroups, each of which may demonstrate better outcomes if treated via specific interventions that have been matched to the individual's signs and symptoms16. Thus, there is a significant need for high-quality research using consistent treatment approaches on well-defined, homogeneous samples of patients26.
This patient appeared to benefit from matched interventions specific to the centralization and exercise and conditioning categories, which included segmental mobilization in the form of CPAs and UPAs, intermittent manual cervical traction, soft tissue mobilization to the suboccipital region, deep neck flexor strengthening, stretching of the shortened pectoralis musculature, and upper quarter strengthening. Throughout Phase I of her treatment, the patient remained primarily within the centralization category, with greater emphasis placed on the exercise and conditioning classification as she progressed with decreased pain, increased ROM, increased functional mobility, improved posture, and less substantial centralization effects.
Our results seem to support the notion that outcomes are better when patients are treated by receiving interventions matched to their appropriate category. The results of this single case report reveal an association between receiving matched interventions and experiencing clinically meaningful reductions in pain and disability. Although a cause-and-effect relationship cannot be inferred from a case report, our results seem to suggest that this particular treatment approach may be beneficial in improving outcomes and restoring functional mobility in patients with mechanical neck pain.
This study is not without limitations that are worth mentioning. First, no formal measurements were taken to document the patient's improved deep neck flexor strength. Although no such formal measurements were recorded, we believe this outcome was portrayed by her dramatic postural improvements and increased ability to perform desk-related work activities. Second, given the scarce availability of literature regarding optimal treatment parameters for commonly used interventions in the management of neck pain, it was difficult to determine dosage parameters throughout the patient's care, lending towards a trial-and-error approach based on patient response.
Additional research is necessary to establish a single, refined, reliable, and valid classification system for the conservative treatment of neck pain. This optimal model may lead to a revolution within the field of physical therapy by increasing the power of clinical research and increasing the effectiveness and efficient management of this population. An effective algorithm would help to eliminate the unexplainable, unwarranted variation in treatment strategies in the cervical spine. Further research is also warranted within each classification of the TBC system to standardize parameters and thus more specifically guide the application of selected interventions.
The purpose of this case report was to provide results following a TBC approach for the management of a patient with cervical spine pain and disability. The positive results obtained in this case with the use of the TBC for the cervical spine seem to suggest that this algorithm may play a pivotal role in leading to improved outcomes as well as increased efficiency and increased cost-effectiveness of care in this population53.
REFERENCES
- 1.Clair DA, Edmondston SJ, Allison GT. Physical therapy treatment dose for nontraumatic neck pain: A comparison between 2 patient groups. J Orthop Sports Phys Ther. 2006;36:867–875. doi: 10.2519/jospt.2006.2299. [DOI] [PubMed] [Google Scholar]
- 2.Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334:527–531. doi: 10.1136/bmj.39127.608299.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther. 2003;8:10–20. doi: 10.1054/math.2002.0480. [DOI] [PubMed] [Google Scholar]
- 4.Hush JM, Maher CG, Refshauge KM. Risk factors for neck pain in office workers: A prospective study. BMC Musculoskelet Disord. 2006;7:81. doi: 10.1186/1471-2474-7-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87:513–524. doi: 10.2522/ptj.20060192. [DOI] [PubMed] [Google Scholar]
- 6.Wang WT, Olson SL, Campbell AH, Hanten WP, Gleeson PB. Effectiveness of physical therapy for patients with neck pain: An individualized approach using a clinical decision-making algorithm. Am J Phys Med Rehabil. 2003;82:203–218. doi: 10.1097/01.PHM.0000052700.48757.CF. quiz 219–221. [DOI] [PubMed] [Google Scholar]
- 7.Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: A randomized clinical trial. Man Ther. 2005;10:127–135. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Hoving JL, de Vet HC, Koes BW, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: Long-term results from a pragmatic randomized clinical trial. Clin J Pain. 2006;22:370–377. doi: 10.1097/01.ajp.0000180185.79382.3f. [DOI] [PubMed] [Google Scholar]
- 9.Vernon H, Humphreys BK. Manual therapy for neck pain: An overview of randomized clinical trials and systematic reviews. Eura Medicophys. 2007;43:91–118. [PubMed] [Google Scholar]
- 10.Vernon HT, Humphreys BK, Hagino CA. A systematic review of conservative treatments for acute neck pain not due to whiplash. J Manipulative Physiol Ther. 2005;28:443–448. doi: 10.1016/j.jmpt.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Philadelphia Panel Evidence-based clinical practice guidelines on selected rehabilitation interventions for neck pain. Phys Ther. 2001;81:1701–1717. [PubMed] [Google Scholar]
- 12.Ylinen J, Kautiainen H, Wiren K, Hakkinen A. Stretching exercises vs. Manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. J Rehabil Med. 2007;39:126–132. doi: 10.2340/16501977-0015. [DOI] [PubMed] [Google Scholar]
- 13.Lewis M, James M, Stokes E, et al. An economic evaluation of three physiotherapy treatments for non-specific neck disorders alongside a randomized trial. Rheumatology (Oxford) 2007;46:1701–1708. doi: 10.1093/rheumatology/kem245. [DOI] [PubMed] [Google Scholar]
- 14.Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine. 2001;26:788–797. doi: 10.1097/00007632-200104010-00020. discussion 798–799. [DOI] [PubMed] [Google Scholar]
- 15.Hoving JL, Gross AR, Gasner D, et al. A critical appraisal of review articles on the effectiveness of conservative treatment for neck pain. Spine. 2001;26:196–205. doi: 10.1097/00007632-200101150-00015. [DOI] [PubMed] [Google Scholar]
- 16.Childs JD, Fritz JM, Piva SR, Whitman JM. Proposal of a classification system for patients with neck pain. J Orthop Sports Phys Ther. 2004;34:686–696. doi: 10.2519/jospt.2004.34.11.686. discussion 697–700. [DOI] [PubMed] [Google Scholar]
- 17.Aker PD, Gross AR, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: Systematic overview and meta-analysis. BMJ. 1996;313:1291–1296. [PMC free article] [PubMed] [Google Scholar]
- 18.Gross AR, Hoving JL, Haines TA, et al. A Cochrane review of manipulation and mobilization for mechanical neck disorders. Spine. 2004;29:1541–1548. doi: 10.1097/01.brs.0000131218.35875.ed. [DOI] [PubMed] [Google Scholar]
- 19.Gross AR, Kay T, Hondras M, et al. Manual therapy for mechanical neck disorders: A systematic review. Man Ther. 2002;7:131–149. doi: 10.1054/math.2002.0465. [DOI] [PubMed] [Google Scholar]
- 20.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2005:CD004250. doi: 10.1002/14651858.CD004250.pub3. [DOI] [PubMed] [Google Scholar]
- 21.Williams GN, Taylor DC, Gangel TJ, Uhorchak JM, Arciero RA. Comparison of the single assessment numeric evaluation method and the Lysholm score. Clin Orthop Relat Res. 2000:184–192. doi: 10.1097/00003086-200004000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine. 2006;31:598–602. doi: 10.1097/01.brs.0000201241.90914.22. [DOI] [PubMed] [Google Scholar]
- 23.Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: A systematic review. Spine. 2002;27:515–522. doi: 10.1097/00007632-200203010-00012. [DOI] [PubMed] [Google Scholar]
- 24.Vernon H, Mior S. The Neck Disability Index: A study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 25.Riddle DL, Stratford PW. Use of generic versus region-specific functional status measures on patients with cervical spine disorders. Phys Ther. 1998;78:951–963. doi: 10.1093/ptj/78.9.951. [DOI] [PubMed] [Google Scholar]
- 26.Cleland JA, Whitman JM, Fritz JM, Palmer JA. Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: A case series. J Orthop Sports Phys Ther. 2005;35:802–811. doi: 10.2519/jospt.2005.35.12.802. [DOI] [PubMed] [Google Scholar]
- 27.Moeti P, Marchetti G. Clinical outcome from mechanical intermittent cervical traction for the treatment of cervical radiculopathy: A case series. J Orthop Sports Phys Ther. 2001;31:207–213. doi: 10.2519/jospt.2001.31.4.207. [DOI] [PubMed] [Google Scholar]
- 28.Hains F, Waalen J, Mior S. Psychometric properties of the neck disability index. J Manipulative Physiol Ther. 1998;21:75–80. [PubMed] [Google Scholar]
- 29.Stratford PW, Binkley JM. Applying the results of self-report measures to individual patients: An example using the Roland Morris Questionnaire. J Orthop Sports Phys Ther. 1999;29:232–239. doi: 10.2519/jospt.1999.29.4.232. [DOI] [PubMed] [Google Scholar]
- 30.Westaway MD, Stratford PW, Binkley JM. The patient-specific functional scale: Validation of its use in persons with neck dysfunction. J Orthop Sports Phys Ther. 1998;27:331–338. doi: 10.2519/jospt.1998.27.5.331. [DOI] [PubMed] [Google Scholar]
- 31.Mystakidou K, Parpa E, Tsilika E, et al. The relationship of subjective sleep quality, pain, and quality of life in advanced cancer patients. Sleep. 2007;30:737–742. doi: 10.1093/sleep/30.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales: Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214–221. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 33.Kendall FP, Kendall EM, Provance PG. Muscles, Testing and Function: With Posture and Pain, 4th ed. Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 34.Cleland JA, Fritz JM, Whitman JM, Heath R. Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87:1619–1632. doi: 10.2522/ptj.20060287. [DOI] [PubMed] [Google Scholar]
- 35.Niere KR, Torney SK. Clinicians' perceptions of minor cervical instability. Man Ther. 2004;9:144–150. doi: 10.1016/S1356-689X(03)00100-0. [DOI] [PubMed] [Google Scholar]
- 36.Yelland MJ. Back, chest and abdominal pain: How good are spinal signs at identifying musculoskeletal causes of back, chest or abdominal pain? Aust Fam Physician. 2001;30:908–912. [PubMed] [Google Scholar]
- 37.Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion: Comparison of three methods. Phys Ther. 1991;71:98–104. doi: 10.1093/ptj/71.2.98. discussion 105–106. [DOI] [PubMed] [Google Scholar]
- 38.Jull G, Bogduk N, Marsland A. The accuracy of manual diagnosis for cervical zygapophysial joint pain syndromes. Med J Aust. 1988;148:233–236. doi: 10.5694/j.1326-5377.1988.tb99431.x. [DOI] [PubMed] [Google Scholar]
- 39.Maitland GD, Hengeveld E, Banks K, English K. Maitland's Vertebral Manipulation, 6th ed. Boston, MA: Butterworth, Heinemannn, Oxford; 2001. [Google Scholar]
- 40.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 41.Govind J. Lumbar radicular pain. Aust Fam Physician. 2004;33:409–412. [PubMed] [Google Scholar]
- 42.Cook C. Orthopedic Manual Therapy: An Evidence-Based Approach. Upper Saddle River, NJ: Prentice Hall; 2007. [Google Scholar]
- 43.Slipman CW, Plastaras C, Patel R, et al. Provocative cervical discography symptom mapping. Spine J. 2005;5:381–388. doi: 10.1016/j.spinee.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 44.Rao R. Neck pain, cervical radiculopathy, and cervical myelopathy: Pathophysiology, natural history, and clinical evaluation. J Bone Joint Surg Am. 2002;84–A:1872–1881. doi: 10.2106/00004623-200210000-00021. [DOI] [PubMed] [Google Scholar]
- 45.Waldrop MA. Diagnosis and treatment of cervical radiculopathy using a clinical prediction rule and a multimodal intervention approach: A case series. J Orthop Sports Phys Ther. 2006;36:152–159. doi: 10.2519/jospt.2006.36.3.152. [DOI] [PubMed] [Google Scholar]
- 46.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–417. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 47.Solly S. Cervical postero-anterior mobilization: A brief review of evidence of physiological and pain relieving effects. Physical Therapy Reviews. 2004;9:182–187. [Google Scholar]
- 48.Falla D. Unraveling the complexity of muscle impairment in chronic neck pain. Man Ther. 2004;9:125–133. doi: 10.1016/j.math.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Chiu TT, Law EY, Chiu TH. Performance of the craniocervical Thexion test in subjects with and without chronic neck pain. J Orthop Sports Phys Ther. 2005;35:567–571. doi: 10.2519/jospt.2005.35.9.567. [DOI] [PubMed] [Google Scholar]
- 50.Vernon H, Humphreys K, Hagino C. Chronic mechanical neck pain in adults treated by manual therapy: A systematic review of change scores in randomized clinical trials. J Manipulative Physiol Ther. 2007;30:215–227. doi: 10.1016/j.jmpt.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 51.Korthals-de Bos IB, Hoving JL, van Tulder MW, et al. Cost-effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: Economic evaluation alongside a randomized controlled trial. BMJ. 2003;326:911. doi: 10.1136/bmj.326.7395.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sran MM. To treat or not to treat: New evidence for the effectiveness of manual therapy. Br J Sports Med. 2004;38:521–525. doi: 10.1136/bjsm.2003.010876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fritz JM, Delitto A, Erhard RE. Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain: A randomized clinical trial. Spine. 2003;28:1363–1371. doi: 10.1097/01.BRS.0000067115.61673.FF. discussion 1372. [DOI] [PubMed] [Google Scholar]