Abstract
Context
Lack of data on the lifetime prevalence and age at onset of suicide ideation, plans, and attempts among blacks in the United States limits the creation and evaluation of interventions to reduce suicide among black Americans.
Objective
To examine the prevalence and correlates of suicide ideation, planning, and attempts across 2 ethnic classifications of blacks in a nationally representative sample.
Design, Setting, and Participants
Data are from the National Survey of American Life, a national household probability sample of 5181 black respondents aged 18 years and older, conducted between February 2001 and June 2003, using a slightly modified adaptation of the World Health Organization World Mental Health version of the Composite International Diagnostic Interview. Bivariate and survival analyses were used to delineate patterns and correlates of nonfatal suicidal behavior.
Main Outcome Measures
Self-reports of lifetime suicide ideation, planning, and attempts.
Results
Survey respondents, categorized as African Americans and Caribbean Americans, reported lifetime prevalence of 11.7% for suicide ideation and 4.1% for attempts. Among the respondents who reported ideation, 34.6% transitioned to making a plan and only 21% made an unplanned attempt. Among 4 ethnic-sex groups, the 7.5% lifetime prevalence for attempts among Caribbean black men was the highest among black Americans. The greatest risk of progressing to suicide planning or attempt among ideators occurred within the first year after ideation onset. Blacks at higher risk for suicide attempts were in younger birth cohorts, less educated, Midwest residents, and had 1 or more Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition disorders.
Conclusions
This study documents the burden of nonfatal suicidality among US blacks, notably Caribbean black men, and individuals making planned attempts. Advancing research on the transition from suicide planning to attempt is vital to the efficacy of health care professionals’ ability to screen blacks at risk for suicide.
Suicide accounts for 1.5% OF the global burden of disease, which represents 20 million years of healthy life lost due to premature death or disability.1 Among all Americans, suicide is the 11th leading cause of death and the rates range across specific demographic subgroups (eg, it is the 8th leading cause of death among Native Americans, Asian/Pacific Islanders, and men).2 Across race and sex, the elderly, particularly white men aged 85 years and older have the highest suicide rate (51.6/year per 100 000 population). 3 The risk of dying from suicide in 2003 was more than double for whites (13.0/100 000) than for blacks (5.3/100 000).4 In recent years, suicide and nonfatal suicidal behavior have emerged as crucial health issues for blacks, particularly among older adolescents and young adults.5–7 According to a recent Centers for Disease Control and Prevention report, the prevalences of attempted suicide for white and black high school students (7.3% and 7.6%, respectively) were roughly equal.8 Although suicide has traditionally been viewed as a problem that affects more whites, the rates of suicide among blacks have increased significantly since the mid 1980s.9 A precipitous increase in the rate of suicide10,11 and nonfatal suicidal behavior12 among younger blacks has reduced US racial disparities in suicidal behaviors. The difference in suicide rates between whites and blacks aged 15 to 24 years narrowed from a ratio of 1.7 in 1980 to 1.4 in 2003.3
Despite increasing recognition of the public health significance of these trends, more comprehensive data on the occurrence of suicidal ideation and attempts are needed to further the understanding of whether the prevention and treatment of antecedents to suicide are effective in reducing risk among this population. Given that the US black population is projected to double by 2050,13 and that suicidal thoughts and behaviors are among the strongest predictors of suicide,14 obtaining national estimates of nonfatal suicidal behavior among this population is an important public health objective. Generating more reliable and more extensive scientific data on nonfatal suicidal behaviors is a critical first step in developing and testing preventive interventions aimed at reducing both suicide morbidity and mortality.
Reports from the Institute of Medicine and US surgeon general have highlighted the need for nationally representative epidemiological data on the occurrence of suicidal thoughts and attempts. 5,7,15 There is no single primary data source for nationally representative information on nonfatal suicidal behavior. 5 Reliable population estimates of such behaviors are hampered by the absence of centralized data registries and consistent definitions of suicide across regions.16–18 Current estimates of nonfatal suicidal behavior in the United States are derived from either ongoing surveillance systems or epidemiological surveys reporting population-based prevalence estimates for suicidal thoughts and attempts.19,20 These systems provide valuable information, but they are limited because they provide little to no race-specific information.5 The most recent epidemiologic studies, the National Comorbidity Survey and the National Comorbidity Survey Replication,19,20 provide national prevalence estimates of suicide ideation, planning, and attempts, but not by race or ethnicity. The most recent data on black adult nonfatal suicidal behaviors are from the National Institute of Mental Health’s Epidemiologic Catchment Area study for 1980–1984, which found a 2.3% lifetime estimate of attempted suicide among US blacks.21 These studies lack information on the onset of suicide ideation, prevalence of suicide planning, and data on the correlates of suicide-related behaviors among blacks. National estimates of the lifetime prevalence and correlates of suicide ideation, planning, and attempts among blacks of African American and Caribbean ethnicity in the United States are reported herein for the first time using the recently collected National Survey of American Life (NSAL).
METHODS
Population and Data Collection
The NSAL is part of the National Institute of Mental Health Collaborative Psychiatric Epidemiology Surveys initiative that includes 3 nationally representative surveys: the NSAL, the National Comorbidity Survey Replication, and the National Latino and Asian American Study.22 The NSAL is a nationally representative household survey of 3570 African Americans, 1621 blacks of Caribbean descent (Caribbean blacks), and 891 non-Hispanic whites, aged 18 years and older.23 The non-Hispanic whites, however, were not administered the full interview and were not asked the suicidality questions. Thus, this report focuses on the African American and Caribbean black samples. The African American sample, the largest segment of the NSAL core sample, is nationally representative of households located in the 48 contiguous states with at least 1 black adult aged 18 years or older who did not identify ancestral ties in the Caribbean. The Caribbean black sample was selected from 2 area probability sample frames: 265 were selected from the house-holds in the core sample, while 1356 were selected from an area probability sample of housing units from geographic areas with a relatively high density of persons of Caribbean descent (more than 10% of the population).24 The NSAL analysis weights for the African American and Caribbean black samples were designed to provide population representation for these populations in the continental US states.
In this study, African American is used to describe individuals who self-identified as black but did not identify ancestral ties to the Caribbean. Caribbean blacks are individuals who self-identified as black and indicated that they were from a country included on a list of Caribbean-area countries presented by the interviewers, or who specified that at least 1 of their parents or grandparents was born in a Caribbean-area country. Most (86%) interviews were conducted face-to-face using a computer-assisted instrument and lasted an average of 2 hours 20 minutes. The remaining interviews (14%) were conducted partially or entirely by telephone. Respondents interviewed by telephone tended to be slightly more educated. No other significant differences in the main outcomes and other variables of interest were found between the 2 interview modes. Data were collected between February 2001 and June 2003. The overall response rate was 71.5%: 70.0% for whites, 70.9% for African Americans, and 79.3% for Caribbean blacks. These rates were calculated using the American Association for Public Opinion Research response rate 3 method,25 which includes in the numerator the number of completed interviews, the number of originally sampled households in the denominator, excludes known ineligible households, and is adjusted for the estimated proportion of eligible households that interviewers were unable to contact. The weighting class method was used to adjust the data for nonresponse bias.26 For all race/ethnic samples, additional NSAL weights were designed to correct for disproportionate sampling and for population representation across various sociodemographic characteristics.24 Descriptive analyses applying these weights yield statistics nationally representative of the populations and subpopulations of interest.
Recruitment and Consent
After introductory letters and study brochures were mailed to sample households, a trained interviewer contacted each sample housing unit in person to further explain the study and asked an adult household informant additional questions (eg, age, sex, race, and Hispanic and Caribbean ancestry status of each household member) to identify a subset of household members eligible to be selected as the NSAL respondent. The Kish27 procedure for objective respondent selection was used to randomly designate 1 of the eligible adults as the NSAL respondent. The interviewers then obtained oral consent and completed the interview, or scheduled it for a later time. Oral instead of written consent was obtained consistent with the National Comorbidity population surveys.19,20 For their participation, each respondent was given $50. The institutional review board of the University of Michigan approved the recruitment, consent, and data collection procedures.
Suicidal Behavior
Suicidality is assessed in its own section of the World Mental Health Composite International Diagnostic Interview (WMH-CIDI) by a series of questions about lifetime suicidal behaviors including ideation, planning, and attempts.28 Respondents were screened into the suicidality section of the WMH-CIDI if they answered affirmatively to the question “Have you ever seriously thought about committing suicide?” These respondents are said to have engaged in suicidal ideation and will be referred to as ideators in this report, while those answering negatively will be referred to as non-ideators. Only the ideators went on to answer questions to determine if they ever made plans to commit suicide (“Have you ever made a plan for committing suicide?”) and if they ever attempted suicide (“Have you ever attempted suicide?”). Respondents answering affirmatively to any of these 3 questions were asked to provide the age when they first experienced the given outcome. To gain a better understanding of the progression from ideation to attempt, we also examined 3 conditional associations corresponding to different pathways individuals may follow from suicidal ideation to attempted suicide: plan given ideation, attempt given ideation but no plan, and finally attempt given ideation and a plan.20 The suicide intent of the respondents was assessed by reading 3 statements and asking the attempters to select 1 of the 3 to describe their first attempt. They were read the 3 statements in order: (1) “I made a serious attempt to kill myself and it was only luck that I did not succeed,” (2) “I tried to kill myself, but knew that the method was not fool proof,” and (3)“My attempt was a cry for help. I did not intend to die.”
Psychiatric Diagnosis and Treatment Experience
The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition29 (DSM-IV) World Mental Health Composite International Diagnostic Interview (WMH-CIDI), a fully structured diagnostic interview, was used to assess a wide range of serious mental disorders and conditions, including suicidality. The psychiatric disorders in the NSAL are slightly modified versions of those developed for the World Mental Health project initiated in 200030 and used in the National Comorbidity Survey Replication.31 We present and discuss risks for various suicidal behaviors associated with the mental disorders assessed in the NSAL: (1) mood (major depressive disorder, dysthymia, bipolar I & II disorders); (2) anxiety (panic disorder, agoraphobia, social phobia, generalized anxiety disorder, probable obsessive compulsive disorder, posttraumatic stress disorder); (3) substance (alcohol abuse, alcohol dependence, drug abuse, drug dependence); (4) disorders usually diagnosed in childhood (separation anxiety, oppositional defiant disorder, conduct disorder, attention deficit/hyperactivity disorder); and (5) eating (anorexia, bulimia, binge-eating).
We also examined suicidal respondents’ treatment experiences for mental disorders assessed in the NSAL. All respondents were asked if they had contact with anyone from an extensive list of treatment providers for problems with their emotions, nerves, mental health, or use of alcohol or drugs in their lifetime. Health care treatment providers were categorized into a mental health sector (psychiatrists, psychologists, counselors and social workers seen in mental health settings, other mental health professionals, mental health hotlines) and a general medical sector (general practitioners, family physicians, nurses, occupational therapists, and other health professionals). A non–health care sector included the use of human services (religious and spiritual advisors, counselors and social workers seen in non–mental health settings) and complementary-alternative treatments (herbalists, chiropractors, spiritualists, self-help groups, Internet support groups). Life-time service use was defined as making at least 1 visit to a service provider prior to the respondent’s interview.
Sociodemographic Correlates
We investigated sociodemographic factors to ascertain groups potentially at elevated risk of suicidal behaviors. Sociodemographic correlates included ethnicity (African American and Caribbean black), sex, highest level of education (less than high school, high school graduate, some college, college graduate), marital status (married, previously married, never married), birth year cohort (1939 or before, 1940–1954, 1955–1964, 1965–1974, 1975 or after), and region (Northeast, Midwest, South, and West Census regions).32
Statistical Analysis
All analyses were weighted to be nationally representative of the populations and subgroups of interest and were conducted usingSAS9.1.3(SAS Institute Inc, Cary, NC).33 Bivariate cross-tabulations were used to calculate the nationally representative prevalences of the suicidal behaviors by sociodemographic characteristics and use of services. Life-table methods were used to derive the age at onset distributions. Cox proportional hazards regression was used to assess risk factors associated with each of the 5 risk pathways to suicidal thought and behaviors (ie, ideation, attempt, planning, attempt given ideation but no plan, and attempt given ideation and a plan).34 Graphical and statistical techniques were used to assess each of the risk factors for proportionality of hazards. The ages at onset, as well as a time-varying marital status risk factor, were determined from the respondents’ retrospective reports.
Procedures were used in all of the analyses to properly adjust SEs, confidence intervals (CIs), and significance tests for the complex sample design of the NSAL. The χ2 and corresponding P values (set at a < .05 level of significance) from these cross-tabulations are based on the Rao-Scott χ2 test, a complex design-adjusted version of the Pearson χ2 test.33 A modified version of balanced repeated replications35 was implemented in an SAS macro to estimate the SEs and CIs of the Cox proportional hazards regression coefficients. These risk coefficients and their 95% CIs were exponentiated and are reported as odds ratios (ORs) for ease of interpretation. The multivariate χ2 tests and corresponding P values associated with these regression models were calculated using the design-based variance-covariance matrices of the coefficients.
RESULTS
Prevalence
TABLE 1 shows the characteristics of the survey participants with the weighted distributions of the sociodemographic characteristics. TABLE 2 presents the estimated lifetime prevalences of the suicidal behaviors. The estimated lifetime prevalence of suicidal ideation and attempts among blacks in the United States was 11.7% and 4.1%, respectively. Among the ideators, 34.6% made a suicide plan. Statistically significant differences (P≤.05) were found between men and women, with attempts being more prevalent for women, 4.9%, than for men, 3.1%. An ethnicity-by-sex analysis revealed the prevalence of suicide attempts was highest for Caribbean black men (7.5%), followed by African American women (5.0%). Caribbean black women had the lowest prevalence of attempts (2.7%), while attempts were only slightly more prevalent for African American men (2.74%).
Table 1.
Sociodemographic Characteristics of the National Survey of American Life Sample by Ethnicity*
| No. (%) [SE]† | ||||||
|---|---|---|---|---|---|---|
| African American (n = 3570) |
Caribbean Black (n = 1621) |
Statistics | ||||
| Sex | ||||||
| Men | 1271 (35.6) [0.8] | 643 (39.7) [1.2] | ||||
| Women | 2299 (64.4) [0.8] | 978 (60.3) [1.2] | ||||
| Marital status‡ | ||||||
| Never married | 1337 (37.6) [1.5] | 639 (39.5) [1.5] | ||||
| Previously married | 1256 (35.4) [0.8] | 418 (25.9) [1.5] | ||||
| Married | 960 (27.0) [1.3] | 559 (34.6) [1.4] | ||||
| Birth year cohort | ||||||
| 1939 or before | 528 (14.8) [0.8] | 182 (11.2) [2.1] | ||||
| 1940–1954 | 738 (20.7) [0.8] | 304 (18.8) [0.6] | ||||
| 1955–1964 | 843 (23.6) [0.7] | 387 (23.9) [1.5] | ||||
| 1965–1974 | 799 (22.4) [0.8] | 401 (24.7) [1.6] | ||||
| 1975 or after | 662 (18.5) [1.2] | 347 (21.4) [1.1] | ||||
| Education status‡ | ||||||
| Less than high school | 916 (25.9) [1.4] | 304 (18.9) [1.7] | ||||
| High school graduate | 1344 (38.1) [1.0] | 477 (29.7) [1.2] | ||||
| Some college | 799 (22.6) [0.9] | 438 (27.3) [1.6] | ||||
| College graduate | 471 (13.3) [1.0] | 388 (24.1) [1.3] | ||||
| Region§ | ||||||
| Northeast | 411 (11.5) [0.8] | 1135 (70.0) [2.4] | ||||
| Midwest | 595 (16.7) [1.6] | 12 (0.8) [0.4] | ||||
| South | 2330 (65.3) [2.1] | 456 (28.1) [2.4] | ||||
| West | 234 (6.5) [0.7] | 18 (1.1) [0.5] | ||||
All estimates in this field represent raw frequencies and percentages; they are not weighted to be nationally representative of the given population and subpopulations in the contiguous 48 US states.
Standard errors and χ2 statistics are adjusted for the sampling stratification and clustering, but not weighting of the data.
There were 17 African American and 5 Caribbean black respondents with missing data for marital status, forty African American and 14 Caribbean black respondents with missing data for education status. Due to this, the variables do not add up to the total.
Northeast denotes Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont; Midwest denotes Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South denotes Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennes-see, Texas, Virginia, and West Virginia; West denotes Arizona, California, Colorado, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, and Wyoming (Alaska and Hawaii are not included in this study).
Table 2.
Estimated Weighted Prevalances of Suicidal Behaviors by Sociodemographic Characteristics, and Disaggregated Through Pathways Involving Ideation, Plans, and Attempts*
| % (SE)† | |||||
|---|---|---|---|---|---|
| Attempt (n = 189)‡ |
Ideation (n = 542)‡ |
Plan Among Ideators (n = 190)§ |
Impulsive Attempt Among Ideators Without a Plan (n = 72)§ |
Planned Attempt Among Ideators With a Plan (n = 117)§ |
|
| Overall 12-month ∥ | 0.18 (0.1) | 2.1 (0.3) | 25.3 (4.9) | 4.7 (2.5) | 20.5 (6.8) |
| Overall | 4.1 (0.5) | 11.7 (0.8) | 34.6 (3.3) | 20.8 (2.7) | 62.1 (3.7) |
| Ethnicity | |||||
| African American | 4.0 (0.5) | 11.7 (0.8) | 33.6 (3.5) | 21.2 (2.8) | 61.0 (3.7) |
| Caribbean black | 5.1 (2.0) | 12.3 (1.8) | 47.9 (12.3) | 14.5 (6.0) | 71.1 (14.7) |
| 0.3 | 0.1 | 1.4 | 0.8 | 0.4 | |
| P value | .57 | .74 | .24 | .36 | .53 |
| Sex | |||||
| Men | 3.1 (0.7) | 10.4 (1.2) | 27.0 (5.4) | 17.0 (3.9) | 64.8 (8.8) |
| Women | 4.9 (0.5) | 12.7 (0.8) | 39.7 (2.9) | 23.8 (3.3) | 60.8 (3.1) |
| 4.3 | 2.7 | 5.6 | 1.9 | 0.2 | |
| P value | .04 | .10 | .02 | .17 | .66 |
| Ethnicity and sex | |||||
| African American men | 2.7 (0.7) | 10.2 (1.3) | 24.3 (5.3) | 17.0 (4.1) | 58.0 (9.9) |
| African American women | 5.0 (0.5) | 12.8 (0.8) | 39.3 (3.0) | 24.5 (3.4) | 62.2 (3.1) |
| Caribbean black men | 7.5 (3.8) | 13.6 (3.8) | 49.9 (21.6) | 16.8 (10.6) | 93.3 (4.5) |
| Caribbean black women | 2.7 (0.7) | 10.9 (1.9) | 45.5 (6.4) | 11.8 (4.9) | 40.2 (13.0) |
| 10.0 | 4.9 | 7.7 | 4.0 | 9.1 | |
| P value | .02 | .18 | .06 | .27 | .03 |
| Marital status | |||||
| Never married | 5.8 (0.8) | 13.3 (1) | 37.3 (4.7) | 29.8 (4.9) | 68.1 (5.8) |
| Previously married | 3.3 (0.5) | 12.9 (1.3) | 35.2 (4.7) | 10.9 (2.9) | 51.6 (5.9) |
| Married | 2.9 (0.8) | 8.9 (1.1) | 29.1 (4.9) | 18.9 (5.2) | 66.3 (10.8) |
| , P value | 11.7 | 12.1 | 1.9 | 10.2 | 2.9 |
| P value | .004 | .003 | .39 | .008 | .24 |
| Birth year cohort | |||||
| 1939 or before | 0.9 (0.5) | 3.5 (0.7) | 25.1 (11.9) | 5.4 (1.0) | 83.7 (16.1) |
| 1940–1954 | 4.9 (1.1) | 13.0 (1.5) | 35.7 (5.0) | 21.1 (6.6) | 68.3 (8.4) |
| 1955–1964 | 3.8 (0.7) | 13.22 (1.6) | 27.6 (5.1) | 16.4 (4.2) | 60.4 (9.9) |
| 1965–1974 | 3.8 (0.8) | 12.3 (1.1) | 37.1 (4.4) | 20.0 (6.7) | 50.0 (6.8) |
| 1975 or after | 5.9 (1.1) | 13.2 (1.4) | 40.7 (5.9) | 30.3 (6.3) | 66.5 (5.0) |
| 16.2 | 32.7 | 5.2 | 5.7 | 4.7 | |
| P value | .003 | <.001 | .27 | .23 | .33 |
| Education status | |||||
| Less than high school | 6.1 (1.0) | 13.9 (1.3) | 36.2 (6.4) | 29.8 (5.6) | 68.9 (7.4) |
| High school graduate | 3.4 (0.7) | 11.8 (1.4) | 32.0 (3.6) | 14.5 (3.6) | 60.3 (7.1) |
| Some college | 4.2 (0.8) | 10.8 (1.1) | 45.0 (7.0) | 22.6 (5.6) | 59.5 (7.9) |
| College graduate | 2.4 (0.8) | 9.2 (1.7) | 20.5 (5.9) | 19.3 (7.4) | 55.2 (13.5) |
| 11.8 | 5.7 | 7.3 | 5.8 | 1.2 | |
| P value | .01 | .13 | .07 | .13 | .75 |
| Region | |||||
| Northeast | 5.6 (1.8) | 14.6 (1.6) | 40.6 (7.1) | 22.6 (8.5) | 60.9 (8.0) |
| Midwest | 5.8 (0.9) | 14.6 (1.7) | 42.7 (7.3) | 16.7 (2.8) | 69.7 (6.60) |
| South | 3.0 (0.4) | 9.7 (0.9) | 25.5 (3.4) | 19.1 (2.0) | 65.7 (5.2) |
| West | 4.6 (1.9) | 12.3 (4.4) | 44.8 (7.5) | 35.0 (14.0) | 40.4 (14.8) |
| 6.2 | 6.3 | 9.6 | 2.9 | 4.6 | |
| P value | .11 | .10 | .02 | .41 | .21 |
All prevalence estimates are weighted to be nationally representative of the given population and subpopulations in the 48 US states.
Standard errors and χ2 statistics are adjusted for the sampling stratification, clustering, and weighting of the data.
The behavioral categories of “attempt” and ideation” present the risks for the unconditional behaviors.
The behavioral categories of plan among ideators, impulsive attempt among ideators without a plan, and planned attempt among ideators with a plan present the risks for the conditional behaviors.
The 12-month frequencies of the 5 behaviors were, in order from left to right, n = 15, n = 98, n = 30, n = 5, and n = 10.
Of attempters, 63.6% reported attempting only once, 18.3% reported 2 attempts, 11.6% reported 3 attempts, and 6.5% reported 4 or more suicide attempts. Attempters were asked to describe the nature of their intent. Among the attempters, 41.7% endorsed the item “I made a serious attempt to kill myself and it was only luck that I did not succeed.” Another 13.7% of attempters endorsed “I tried to kill myself, but knew that the method was not fool proof” while 44.6% endorsed “My attempt was a cry for help. I did not intend to die.”
Reported Age at Onset Distributions
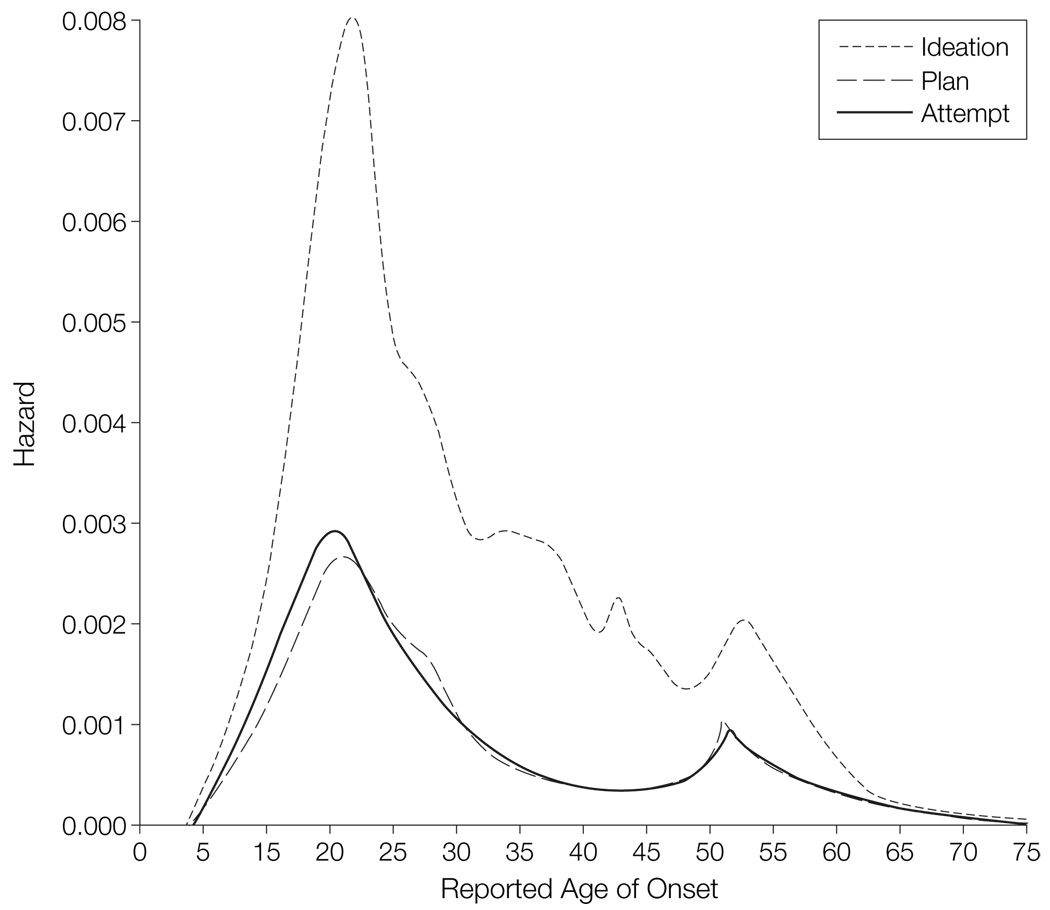
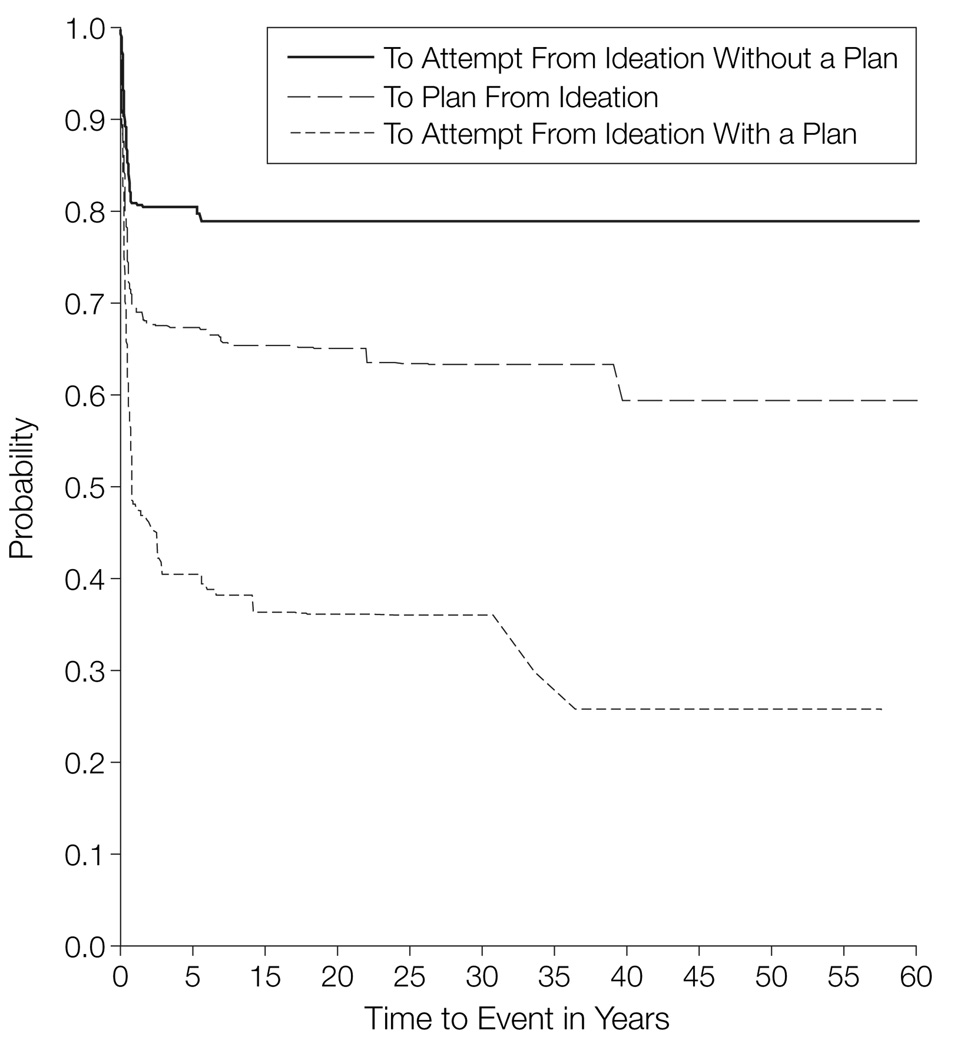
FIGURE 1 shows the smoothed hazard curves for the reported initial onset of suicide ideation, planning, and attempt for the entire sample. These curves indicate that the highest risk of initial onset of these behaviors occurs during the late teens and early 20s. Notably, the risk of making a suicide attempt is greater than the risk of making a suicide plan during this age period suggesting that nonplanned, impulsive attempts are more common than planned attempts until respondents reach their early 20s. FIGURE 2 shows how soon after initial ideation onset respondents progressed to more serious suicidal behaviors. The figure shows that the greatest risk of progressing to plan formation and to attempt among ideators occurred within the first year after ideation onset. Risk of attempt was substantially greater in the presence of a plan. While attempts were almost exclusively confined to the first year after ideation onset in the absence of a plan, individuals with a plan continued to make initial suicide attempts for up to 35 years after first onset of ideation. The mean time from initial ideation onset to first suicide attempt was 1.39 (SE, 0.47) years with a range of 0 to 35 years; however, 77.3% of attempters did so within the first year after ideation onset. Within 3 years of ideation onset, 90% of attempters had made an attempt, and 95% had made an attempt by the end of the sixth year after ideation onset.
Figure 1. Age of Onset of Lifetime Suicide Ideation, Plan, and Attempt Among Blacks (n=5002).
The smoothed hazard functions describe the ways in which the onset risks of the 3 suicidal behaviors change with time. For all behaviors, the highest risk occurs from the teenage years to the mid-twenties. From the mid-twenties, the risks generally decline gradually with the exception of a slight increase from the mid-forties to mid-fifties. Notice that the risk of attempting suicide is slightly higher than the risk of making a suicide plan until approximately age 19 years, when the 2 hazard curves cross. This suggests that nonplanned, impulsive attempts are more likely than planned attempts up to this point in young adulthood.
Figure 2. Conditional, Cumulative Speed of Onset From Ideation to Suicide Plan, Impulsive and Planned Attempt Onset (n=542).
The x-axis represents time in years from the first onset of suicidal ideation. The y-axis represents the event-free survival probability. For example, among ideators with a suicide plan, the probability of not attempting suicide decreases to less than 50% in the first 2 years after ideation onset. The probability of remaining attempt-free continues to decrease gradually until 35 years after ideation onset. At this point, only approximately 25% of individuals who made a suicide plan have not made an attempt, while 75% have attempted. Contrast this with the ideators who did not make suicide plans. After a sharp decrease in the first year after ideation onset, the respondents’ probability of remaining attempt-free stabilizes at about 80%.
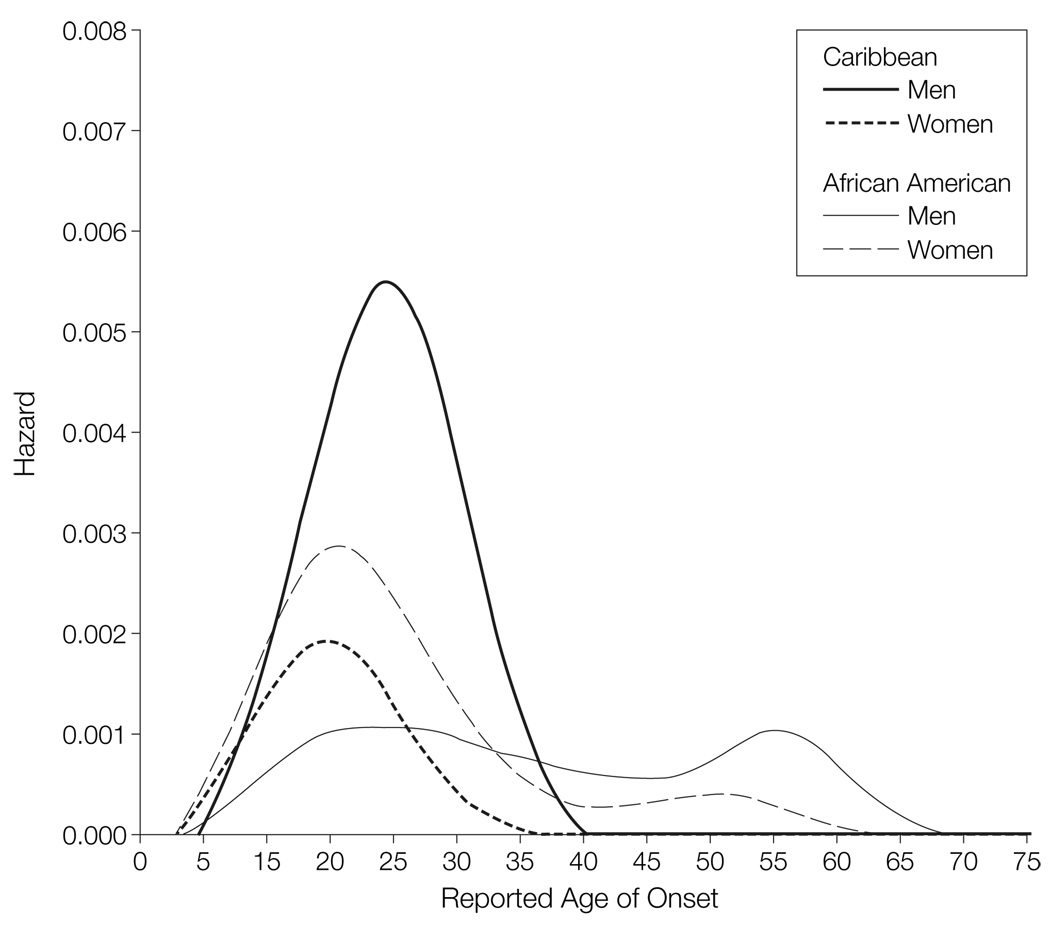
Based on the prevalence estimates, which suggested an interaction between ethnicity and sex, we examine the hazard curves for first attempts separately for each of 4 ethnicity-sex groups (FIGURE 3). These curves give a more complete understanding of the prevalence rates; specifically, 3 important findings are evident in Figure 3. First, Caribbean black males had the highest rates of attempt from ages 10 to 34 years, and the age at which they were most at risk of attempting, approximately 21 years, was almost 5 years older than the ages of highest risk for the 2 female groups. Second, African American men had a relatively constant low hazard of attempt, but were actually the group most at risk of attempting after age 34 years. Third, all groups had peaks of varying magnitude in their risks of attempting suicide during adolescence and early adulthood; however, the risk of attempt persisted into older adulthood only for the 2 African American groups.
Figure 3. Age of Onset of Lifetime Suicide Attempt Among Blacks by Ethnicity and Sex (n=5002).
These smoothed hazard functions describe the ways in which the risk of first suicide attempt changes with time for the 4 sex-by-ethnicity groups. As in Figure 1, the greatest risk generally occurs during the teenage years to the mid-twenties. African American men are at notably lower risk of making an attempt than the other 3 groups until their mid-20s and actually become the group most at risk after approximately age 34 years. Caribbean black men are most at risk up to this age.
Sociodemographic Risk Factors
Risk of a suicide attempt and risk of suicidal ideation were significantly associated with being born in a recent cohort, having a low education level, and residing in the Midwest region of the United States (TABLE 3). In addition, being previously married (eg, divorced or widowed) was significantly associated with increased odds of suicidal ideation compared with being married. Although Caribbean black men and African American women had a higher prevalence of suicide attempts, the 4-category ethnicity-by-sex variable was not significantly associated overall with attempted suicide at the P<.05 level . The results for birth-year cohort suggested the presence of a linear trend for all 5 of the outcomes. In particular, individuals born in recent cohorts were significantly more likely to develop a suicide plan and to attempt suicide . In contrast, the more recent birth-year cohorts were less likely to make a planned suicide attempt than were respondents in the earliest-born cohort ; however, this applies only to the overall cohort effect because none of the individual ORs reached statistical significance. This result supplements the finding from Figure 1 that suggested that non-planned, impulsive attempts are more common than planned attempts for respondents until their early 20s. Follow-up model-based trend tests confirmed the significant linear birth-year cohort trends for all of the outcomes; curvilinear trend terms were tested but none were significant. Respondents with fewer than 12 years of formal education were 3.64 (95% CI, 1.63–8.15) times more likely to attempt suicide than were individuals with 16 or more years of education. Respondents residing in the Southern region of the United States were less likely to attempt suicide and less likely to develop suicidal ideation than were respondents living in other regions of the nation. In particular, respondents residing in the Midwest were 2.04 times more likely to attempt suicide and 1.59 times more likely to develop suicidal ideation than those living in the South, while respondents residing in the Northeast were 1.62 times more likely to develop suicidal ideation than those living in the South.
Table 3.
Multivariate Sociodemographic Predictors of Suicidal Behaviors Disaggregated Through Pathways Involving Ideation, Plans, and Attempts
| Odds Ratio (95% Confidence Interval)* | |||||
|---|---|---|---|---|---|
| Attempt (n = 189)† |
Ideation (n = 542)† |
Plan Among Ideators (n = 190)‡ |
Impulsive Attempt Among Ideators Without a Plan (n = 72)‡ |
Planned Attempt Among Ideators With a Plan (n = 117)‡ |
|
| Ethnicity and sex | |||||
| African American man | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| African American woman | 1.77 (1.09–2.87)§ | 1.30 (0.995–1.71) | 2.08 (1.09–3.96)* | 1.54 (0.68–3.49) | 1.52 (0.84–2.78) |
| Caribbean black man | 2.46 (1.02–5.93)§ | 1.39 (0.77–2.50) | 2.35 (0.57–10.66) | 1.17 (0.15–9.03) | 2.78 (0.995–7.77) |
| Caribbean black woman | 0.85 (0.33–2.16) | 1.00 (0.07–1.38) | 2.47 (1.01–6.07)* | 0.78 (0.18–3.49) | 0.99 (0.22–4.43) |
| ∥ | 5.96 | 4.62 | 5.60 | 1.45 | 3.46 |
| P value | .11 | .20 | .13 | .69 | .33 |
| Marital status | |||||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Never married | 1.06 (0.55–2.05) | 1.19 (0.88–1.62) | 0.99 (0.56–1.75) | 0.98 (0.32–2.99) | 1.09 (0.50–2.36) |
| Previously married | 1.11 (0.38–3.19) | 3.09 (1.87–5.10)* | 0.99 (0.45–2.18) | 1.36 (0.32–5.77) | 0.27 (0.05–1.43) |
| ∥ | 0.05 | 10.30 | 0.57 | 0.23 | 2.78 |
| P value | .82 | <.004 | .45 | .63 | .10 |
| Birth year cohort | |||||
| 1939 or before | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1940–1954 | 4.28 (1.79–10.23)§ | 2.94 (1.89–4.58)* | 1.62 (0.27–9.94) | 1.84 (0.41–8.34) | 0.22 (0.05–1.08) |
| 1955–1964 | 3.96 (1.49–10.52)§ | 3.76 (2.58–5.48)* | 1.30 (0.20–8.34) | 1.29 (0.31–5.39) | 0.26 (0.05–1.33) |
| 1965–1974 | 4.78 (2.09–10.94)§ | 4.62 (3.20–6.67)* | 2.07 (0.28–15.35) | 1.83 (0.39–8.47) | 0.29 (0.06–1.52) |
| 1975 or after | 9.44 (4.33–20.62)§ | 7.41 (4.68–11.72)* | 3.69 (0.48–28.52) | 4.1 (0.99–17.37) | 0.94 (0.19–4.68) |
| ∥ | 17.92 | 41.55 | 9.66 | 8.16 | 13.22 |
| P value | <.001 | <.001 | .047 | .09 | .01 |
| Education status | |||||
| Less than high school | 3.64 (1.63–8.15)§ | 2.08 (1.39–3.11)* | 1.97 (0.73–5.30) | 1.70 (0.61–4.71) | 1.43 (0.51–3.99) |
| High school graduate | 1.94 (0.89–4.20) | 1.60 (1.04–2.47)* | 1.97 (0.83–4.65) | 0.78 (0.28–2.16) | 1.33 (0.47–3.77) |
| Some college | 2.23 (0.89–5.60) | 1.34 (0.86–2.08) | 3.06 (1.23–7.62)* | 1.30 (0.43–3.91) | 1.65 (0.57–4.79) |
| College graduate | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ∥ | 8.92 | 9.55 | 5.65 | 4.28 | 1.04 |
| P value | .001 | <.001 | .13 | .23 | .79 |
| Region | |||||
| Midwest | 2.04 (1.34–3.11)§ | 1.59 (1.11–2.29)* | 2.19 (1.10–4.35)* | 0.94 (0.38–2.30) | 1.14 (0.62–2.11) |
| Northeast | 1.88 (0.76–4.65) | 1.62 (1.13–2.32)* | 1.83 (1.06–3.16)* | 1.18 (0.53–2.63) | 1.04 (0.56–1.93) |
| West | 1.77 (0.73–4.30) | 1.50 (0.68–3.29) | 3.38 (1.33–8.57)* | 2.74 (1.04–7.20)* | 0.43 (0.16–1.16) |
| South | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ∥ | 9.29 | 12.73 | 12.51 | 4.68 | 3.89 |
| P value | .007 | <.001 | .06 | .20 | .26 |
Odds ratios were obtained by exponentiating the coefficients from Cox proportional hazards regression models. The 95% confidence intervals were obtained using a modified method of balanced repeated replications to adjust for stratification, clustering, and weighting of the data. A single model was estimated for each of the 6 outcomes that included all of the predictor variables.
The behavioral categories of attempt and ideation present the risks for the unconditional behaviors.
The behavioral categories of plan among ideators, impulsive attempt among ideators without a plan, and planned attempt among ideators with a plan present the risks for the conditional behaviors.
P< .05 by a 2-sided test.
Wald χ2 values were obtained from design-based variance-covariance matrices to adjust for the stratification, clustering, and weighting of the data.
Psychiatric Risk Factors
Multivariate Cox proportional hazards models controlling for all of the sociodemographic variables included in Table 3 were used to assess the risks of engaging in the suicidal behaviors associated with the 20 DSM-IV disorders assessed in the NSAL.TABLE 4 presents the ORs and 95% CIs for these disorders, omitting the results for the control variables. Because 135 models (27 models for each of the 5 outcomes) were constructed for Table 4 with a total of 145 statistically tested comparisons, the P values of these statistics were adjusted to control for the false discovery rate.36 This method is preferable to controlling for the family-wise error rate when the multiple comparisons are not independent. 37 Although 95% CIs remain unadjusted, asterisks indicate which estimates in Table 4 are significant according to the more stringent adjusted P values. Respondents with any of the 20DSM-IV disorders assessed in the NSAL were 8.2 times (95% CI, 4.77–14.06) more likely to attempt suicide and almost 5 times more likely to develop suicidal ideation (OR, 4.96; 95% CI, 3.48–7.06) than were respondents with no disorder. Having any disorder was also associated with increased risk among ideators of proceeding to make a suicide plan. All 5 of the summary variables for the diagnostic classes (eg, any mood disorder, any anxiety disorder) were significantly associated with elevated risks of attempting suicide (OR range, 3.15 for any eating disorder to 6.03 for any anxiety disorder).
Table 4.
Multivariate Associations of NSAL/DSM-IV Disorders With Subsequent First Onset of Attempted Suicide in the Total Sample and Disaggregated Through Pathways Involving Ideation, Plans, and Attempts
| Odds Ratio (95% Confidence Interval)* | |||||
|---|---|---|---|---|---|
| Attempt (n = 189)† |
Ideation (n = 542)† |
Plan Among Ideators (n = 190)‡ |
Impulsive Attempt Among Ideators Without a Plan (n = 72)‡ |
Planned Attempt Among Ideators With a Plan (n = 117)‡ |
|
| Any disorder | 8.19 (4.77–14.06)§ | 4.96 (3.48–7.06)§ | 2.37 (1.34–4.19)§ | 1.59 (0.66–3.82) | 2.16 (0.54–8.62) |
| Mood disorders | |||||
| Any mood disorder | 3.83 (2.77–5.30)§ | 4.11 (3.23–5.24)§ | 1.35 (0.88–2.06) | 0.97 (0.49–1.93) | 0.87 (0.45–1.67) |
| Major depressive disorder | 3.80 (2.80–5.16)§ | 3.83 (3.09–4.74)§ | 1.31 (0.93–1.83) | 0.98 (0.48–1.99) | 0.92 (0.55–1.54) |
| Dysthymia | 6.24 (3.70–10.52)§ | 4.84 (3.41–6.89)§ | 1.17 (0.71–1.92) | 2.79 (1.26–6.17)* | 1.11 (0.56–2.21) |
| Bipolar I–II disorder (Includes sub-threshold) | 3.59 (2.12–6.09)§ | 3.07 (1.96–4.81)§ | 1.69 (0.66–4.36) | 1.15 (0.39–3.38) | 1.61 (0.79–36.28) |
| Anxiety disorders | |||||
| Any anxiety disorder | 6.03 (3.77–9.64)§ | 4.02 (3.24–4.99)§ | 1.69 (1.04–2.74)§ | 1.70 (0.91–3.17) | 1.76 (1.02–3.03) |
| Panic disorder | 5.34 (3.11–9.17)§ | 4.15 (2.78–6.21)§ | 1.38 (0.62–3.07) | 1.24 (0.47–3.31) | 1.49 (0.74–3.00) |
| Agoraphobia without panic | 2.67 (1.26–5.66)§ | 2.08 (1.24–3.50)§ | 0.94 (0.27–3.31) | 1.28 (0.34–4.82) | 2.14 (0.69–6.62) |
| Social phobia | 2.43 (1.25–4.70)§ | 2.27 (1.55–3.32)§ | 1.08 (0.46–2.54) | 1.30 (0.58–2.91) | 1.03 (0.54–1.94) |
| Generalized anxiety disorder | 4.16 (2.41–7.20)§ | 3.84 (2.68–5.50)§ | 1.33 (0.73–2.44) | 1.05 (0.43–2.54) | 1.40 (0.73–2.70) |
| Obsessive-compulsive disorder∥ | 5.30 (2.01–13.99)§ | 5.03 (3.32–7.61)§ | 1.06 (0.44–2.58) | 1.19 (0.34–4.16) | 1.08 (0.41–2.83) |
| Posttraumatic stress disorder | 5.89 (3.81–9.08)§ | 4.02 (3.18–5.08)§ | 1.78 (1.08–2.94)§ | 2.05 (1.06–3.99) | 1.66 (1.01–2.74) |
| Substance disorders | |||||
| Any substance disorder | 4.53 (3.02–6.80)§ | 3.11 (2.38–4.08)§ | 1.14 (0.70–1.87) | 1.56 (0.77–3.17) | 1.51 (0.83–2.76) |
| Alcohol abuse | 4.75 (3.10–7.29)§ | 3.26 (2.47–4.31)§ | 1.01 (0.66–1.57) | 1.46 (0.71–3.01) | 1.47 (0.79–2.73) |
| Alcohol dependence | 5.65 (3.45–9.26)§ | 3.97 (2.78–5.66)§ | 0.67 (0.30–1.49) | 2.29 (1.05–4.97) | 1.68 (0.71–4.00) |
| Drug abuse | 5.18 (3.37–7.97)§ | 2.99 (2.10–4.26)§ | 1.18 (0.68–2.05) | 1.30 (0.58–2.92) | 2.05 (1.06–3.98) |
| Drug dependence | 6.34 (3.17–12.69)§ | 3.15 (1.83–5.44)§ | 1.03 (0.18–5.96) | 2.19 (0.86–5.53) | 1.92 (0.81–4.56) |
| Childhood disorders | |||||
| Any childhood disorder | 4.25 (3.02–5.99)§ | 3.14 (2.44–4.03)§ | 1.42 (0.89–2.27) | 2.49 (1.06–5.82)* | 1.47 (0.69–3.10) |
| Separation anxiety disorder | 3.59 (1.90–6.82)§ | 3.09 (2.25–4.26)§ | 1.38 (0.67–2.81) | 1.47 (0.59–3.69) | 1.63 (0.81–3.29) |
| Oppositional-defiant disorder | 2.48 (1.42–4.32)§ | 2.05 (1.51–2.78)§ | 1.76 (0.99–3.12) | 1.28 (0.47–3.46) | 1.94 (0.87–4.31) |
| Conduct disorder | 4.98 (3.28–7.57)§ | 3.18 (2.28–4.44)§ | 1.64 (0.99–2.72) | 2.87 (1.35–6.11)* | 1.90 (0.98–3.69) |
| Attention-deficit/hyperactivity disorder | 6.20 (3.75–10.26)§ | 3.78 (2.65–5.39)§ | 1.55 (0.80–3.02) | 2.25 (0.86–5.87) | 3.06 (1.52–6.19)* |
| Eating disorders | |||||
| Any eating disorder | 3.15 (1.83–5.45)§ | 2.87 (2.06–4.00)§ | 1.71 (0.75–3.91) | 1.79 (0.29–10.94) | 1.30 (0.65–2.59) |
| Anorexia¶ | 10.29 (1.96–54.18)§ | 3.88 (0.86–17.59) | Unestimable | 15.30 (2.41–97.08)* | Unestimable |
| Bulimia | 2.71 (0.84–8.72) | 2.84 (1.40–5.77)* | 2.42 (0.50–11.78) | 3.71 (1.01–13.60) | 0.77 (0.17–3.50) |
| Binge-eating | 3.23 (1.88–5.54)§ | 2.93 (2.06–4.17)§ | 1.72 (0.71–4.19) | 1.83 (0.77–4.35) | 1.30 (0.65–2.59) |
| No. of comorbid disorders | |||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 3.95 (2.12–7.37)§ | 2.62 (1.67–4.12)§ | 2.41 (1.48–3.94)§ | 1.21 (0.31–4.66) | 1.73 (0.66–4.58) |
| 2 | 4.94 (2.22–10.99)§ | 3.98 (2.93–5.42)§ | 1.97 (0.99–3.92) | 1.15 (0.16–8.44) | 1.37 (0.46–4.07) |
| ≥3 | 17.13 (9.32–31.47)§ | 9.74 (6.80–13.95)§ | 2.51 (1.25–5.05)§ | 2.05 (0.77–5.49) | 2.68 (1.12–6.40) |
Abbreviations: DSM–IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; NSAL, National Survey of American Life.
Odds ratios were obtained by exponentiating the coefficients from Cox proportional hazards regression models. The 95% confidence intervals were obtained using a modified method of balanced repeated replications to adjust for stratification, clustering, and weighting of the data. Each column presents the results from 27 models. Each of these models controlled for the sociodemographic variables presented in Table 2. In addition, each model contained exactly 1 of the 20 individual disorders, exactly 1 of the 6 summary measures (any disorder, any mood disorder, etc.), or the set of dummy variables representing the number of comorbid disorders. All disorders were defined without diagnostic hierarchy rules.
The behavioral categories of attempt and ideation present the risks for the unconditional behaviors.
The behavioral categories of plan among ideators, impulsive attempt among ideators without a plan, and planned attempt among ideators with a plan present the risks for the conditional behaviors.
Indicates odds ratio estimates that are significantly different from 1.00 using the false discovery rate method of adjusting for multiple comparisons. For the 145 tests in this table, this significance criterion was P<.0231. Confidence intervals remain unadjusted. As a result, it is possible for an odds ratio to be nonsignificant by this criterion even though 1.00 lies outside of the corresponding 95% confidence interval.
This obsessive compulsive diagnosis is based on the World Mental Health Composite International Diagnostic Interview Short Form and should be considered a probable diagnosis.
Only a small number of respondents met criteria for anorexia. As such, these risk coefficients tend to be artificially high, low, or unestimable.
The effects of comorbidity are presented at the bottom of Table 4. Having 3 or more disorders was strongly associated with all of the pathways except for impulsive attempts. Persons with 3 or more disorders were 17 times more likely (17.13; 95% CI, 9.32–31.47) to attempt suicide and about 10 times more likely (9.74; 95% CI, 6.80–13.95) to develop suicidal ideation than respondents with no psychiatric disorder. Ideators with 3 or more disorders were more than 2.5 times as likely to make a suicide plan. The risks of attempts and of ideation are greater for persons with 1 disorder than for persons with no disorder, and slightly greater for persons with 2 disorders than for persons with only 1 disorder.
Treatment for Mental Disorders
TABLE 5 shows on the lifetime history of receiving treatment for emotional problems among attempters and suicide ideators with no history of an attempt. The results show that approximately 1-in-4 attempters (24.3%) and almost half of ideators (43.6%) have never sought treatment for emotional problems. When attempters have sought treatment for their mental health problems many report contacting a mental health professional (58.5%; SE, 4.8%), namely a psychiatrist (45%; SE, 3.8%). Among attempters who sought treatment in any of the sectors, only39%did so before their first suicide attempt. There were 32% of attempters who also reported seeking treatment for their emotional problems in the general medical sector. Of the attempters who sought treatment for mental health problems in the general medical sector, 38.3% made their initial treatment contact before their first attempt. In addition, the treatment preferences of black American suicide attempters vary, with a quarter of them also reporting having gone to non–health service professionals, such as religious or spiritual advisors or massage therapists, for their emotional problems.
Table 5.
Prevalence of Lifetime Use of Services by Service Sector Among NSAL Respondents With and Without Reported Suicide-Related Behaviors
| Service Sector† | % (SE)* | ||
|---|---|---|---|
| Ideators With No Reported Attempt History (n = 353) |
Attempters (n = 189) |
NSAL Respondents With No Reported Ideation History (n = 4443) |
|
| Any treatment | 56.4 (4.1) | 75.7 (2.7) | 24.1 (0.9) |
| Health service | 50.2 (4.0) | 70.8 (3.5) | 21.3 (0.9) |
| General medical | 19.8 (3.0) | 32.0 (4.4) | 12.4 (0.8) |
| Mental health specialty | 40.9 (3.5) | 58.5 (4.8) | 12.2 (0.6) |
| Psychiatrist | 33.0 (3.4) | 45.0 (3.8) | 8.1 (0.6) |
| Nonpsychiatrist | 17.2 (2.7) | 35.5 (5.3) | 6.0 (0.5) |
| Non–health service | 25.0 (2.5) | 25.5 (4.3) | 7.3 (0.6) |
| Complementary-alternative | 13.3 (2.8) | 14.7 (2.8) | 2.9 (0.4) |
| Human service | 15.4 (2.1) | 15.9 (3.5) | 4.9 (0.5) |
Abbreviation: NSAL, National Survey of American Life.
All prevalence estimates are weighted to be nationally representative of the given subpopulations in the contiguous 48 US states. Standard errors are adjusted for the sampling stratification, clustering, and weighting of the data.
Within each service sector, χ2 statistics were statistically significant at the P<.0001 level, suggesting a strong association between use within each sector and the 3 groups. Any mental health treatment includes treatment by a psychiatrist, as well as by a nonphysician mental health specialist (eg, psychologist, social worker in a mental health specialty setting). General medical treatment includes treatment by any nonpsychiatrist physician or a worker in a general medical setting (eg, nurse in a primary care setting). In addition to including mental health and general medical treatment, the category of any treatment includes treatment in non–health care settings including human services professionals (eg, religious or spiritual advisors) and complementary-alternative treatments (eg, massage therapy, chiropractic treatment, or participation in a self-help group).
COMMENT
The 4.1% lifetime prevalence of attempted suicide among blacks is well above previous reports for this population, such as the 2.8% prevalence found in community surveys,21 but is near the 4.6% reported by the National Comorbidity Survey20 for the general population. The NSAL 12-month prevalence estimate of 0.2% is 2 to 3 times less than the report for the nation in the National Comorbidity Survey (0.4%)and National Comorbidity Survey Replication (0.6%), respectively.19 Similar to National Comorbidity Survey findings, NSAL data indicate that the greatest risk of progressing to plan formation and to attempt among ideators occurs within the first year after ideation onset. We found in this study, however, that ideators with a plan continued to make initial suicide attempts up to 35 years after the first onset of ideation. Thus, we report for the first time important ethnic differences among blacks in the lifetime prevalence of suicide ideation, planning, and attempts and the prevalence of mental health service use among black attempters and ideators. There are no similar data with which to compare the results obtained in the NSAL. The reported 4.9% prevalence of attempted suicide among Caribbean blacks, however, was at the high end of prevalence rates of attempted suicide reported in previous general population surveys.19–21
The notably higher prevalence of attempted suicide among black women is consistent with previous studies of suicidal behaviors. However, the 7.5% prevalence rate among Caribbean black men is different from previous findings for US-based populations that women uniformly have higher rates of attempted suicide than men.38 In fact, Caribbean black men reported the highest rate of attempted suicide for the US black population. The reasons for the unexpected higher risk for attempted suicide among Caribbean black men must be examined in future research. It is important to understand whether this unique finding is potentially an example in which ethnicity is per se more salient than nativity, race, and assimilation.
The findings that the risk for attempted suicide is highest in the age group of 15 to 24 years, and that younger generations of blacks are at significantly higher risk of attempted suicide, are consistent with independent evidence of marked increases in suicide among younger blacks.6,11,39 Recent research on reasons for higher suicide risk among younger blacks have suggested that younger blacks have increased access to lethal methods,40,41 have more psychiatric disorders, and may hold accepting attitudes toward suicide.42–44
The relationship between the risk for suicide attempts and other sociodemographic correlates is consistent with previous results based on cross-sectional surveys and clinical or community samples. For instance, previous research has established that there is an inverse relationship between education and attempted suicide.20 According to our analyses, blacks with less than a high school education were more likely to have attempted suicide. Blacks in the Midwest were at a significantly higher risk for attempted suicide than those residing in the South, consistent with research suggesting that Southern residence is a protective factor for this population.45 Analyses revealed that marital status, though often found to be an important correlate,46 was not a significant predictor of suicide planning or attempts in these populations.
Consistent with research on other populations, psychiatric disorders, including substance abuse diagnosis47 and comorbid psychiatric disorders,48,49 were significant predictors of attempted suicide among black ideators. Our analyses showed that ideators with any psychiatric disorder were 8 times more likely to attempt suicide. Individuals with any form of anxiety disorder had the highest risk of attempted suicide, followed by those with a childhood disorder, those with a mood disorder, and those with an eating disorder. The dose-response relationship between the number of psychiatric disorders and attempted suicide is consistent with other cross-sectional studies and community epidemiological surveys.20 The finding that anxiety disorder is the strongest predictor compared with other mental or substance abuse predictors is inconsistent with other studies, which found that depression is often the strongest psychiatric risk factor for suicide.14
Suicide often occurs in the context of a wide range of complex and interrelated underlying etiological factors. The NSAL finding that psychiatric comorbidity is a significant predictor of suicide attempts over and above the effects of individual disorders is consistent with previous research on adult suicidal behavior.20 The greater the number of psychiatric disorders an individual has, the higher the risk of attempted suicide. 49 According to NSAL data, ideators with 3 or more psychiatric disorders are 17 times more likely to attempt suicide and twice as likely to attempt after making a plan. In all instances, however, the ORs for individuals with only 1 disorder and for those with 2 disorders are similar. This suggests the presence of a threshold, rather than linear, effect for number of psychiatric disorders. That is, the suicide risks increase when 1 disorder is present, stay relatively constant in the presence of 2 disorders, and increase drastically again in the presence of 3 or more disorders.
Limitations
The NSAL findings must be considered in the context of several important limitations. The results reported here are limited by the fact that we do not know the extent to which cultural factors affected the willingness of our respondents to either admit or recall the presence of symptoms or suicide over their lifetime. The results may also be affected by recall bias associated with the respondents’ age and mental health status. Also for all analyses, the results are limited by the absence of respondents currently in institutional settings (not unusual for a household-based survey). The NSAL is cross-sectional, obtaining retrospective reports; thus the prevalence rates are likely to be lower-bound estimates.20 Research suggests that some DSM-IV diagnoses may be overestimated using lay-administered interviewing, particularly nonaffective psychoses,50,51 but studies have found that estimates of prevalence using the WMH-CIDI are generally conservative. 52 Finally, our sample of Caribbean blacks includes immigrants who have had varying lengths of stay in the United States, as well as persons of Caribbean ancestry who were born in the United States with no strong knowledge of or identification with Caribbean culture. Despite these constraints, the effect of most of the noted limitations is to make our estimates more conservative than might otherwise be the case. In view of current gaps in our understanding of the risk for suicidal behavior among blacks, these constraints seem acceptable in light of information about prevalence and correlates of suicide risk in this large and diverse sample of black Americans.
CONCLUSIONS
The NSAL provides the first nationally representative general population data on ethnic differences in lifetime suicide ideation, planning, and attempts among blacks. The NSAL results provide evidence that black Americans have levels of suicidal thought and behaviors that are comparable with the general population. Future research should continue to further clinicians’ understandings of which black Americans are most at risk for suicide (intra-group analyses). The information obtained from these types of studies is very different from what is gained from examining, relative to whites, which black Americans are most likely to attempt suicide. These lines of investigation are both important, but the latter cannot provide the same level of subpopulation specificity regarding the suicide risk factors. The higher rates of attempted suicide, notably among Caribbean black men, and the role of nativity vs ethnicity needs to be addressed in future research and considered by clinicians when screening, intervening, and treating black patients. There is a need to explore whether different immigration experiences (eg, type of acculturation, trans-migration experiences, specific origins of immigrants) are responsible for the higher attempt rates in Caribbean black men, and if this result is an example of a situation where a combination of black race and strong ethnic ties (Caribbean)combineto place a black ethnic group at greater risk than when race alone serves to produce a powerful homogenizing set of experiences that may be protective, (eg, among African American men). Future research should also explore how black American suicidal behavior is associated with psychological resources (eg, social support, connectedness), multiple measures of socioeconomic status (including material hardship) and the access to as well as the timing, duration, and adequacy of treatment for mental disorders.
Physicians have an important role to play in the prevention of suicide among black patients, given our results that a majority of attempters sought care from a health professional for their emotional problems and about a third sought care from a general medical professional specifically. Physicians and mental health professionals should be skilled in talking with black patients about the risk for suicide, providing interventions for those at imminent risk for suicidal behavior, and referring patients for expert assessment and treatment. The results of the study should influence clinicians who screen patients for suicide risk. For instance, clinicians should focus on modifiable risk factors (eg, anxiety, depression) and should engage blacks in aggressive treatment in the high-risk period of the first year after ideation onset and continue to observe patients who attempt suicide after making a plan. Clinicians must also consider, when screening blacks, the strong association of DSM-IV disorders with the risk for suicide attempts, the greater likelihood for young adults to be impulsive, and for older adults to engage in planned suicide attempts. It is also important that black patients at risk for impulsive attempts do not have access to firearms or medications that can be used to attempt suicide.
Acknowledgment
We appreciate the assistance provided in all aspects of the NSAL study by the Program for Research on Black Americans faculty and research staff including Myriam Torres, MS, Jamie Abelson, MSW, MS, Deborah Coral, BA, Nakesha Faison, MS, Jane Rafferty, MA, Phyllis Stillman, BA, and Julie Sweetman, MS. We thank the staff at the Survey Research Center’s Survey Research Operations department for their assistance with instrumentation and fieldwork for the NSAL study. We are grateful to Linda Chatters, PhD (School of Social Work, University of Michigan, Ann Arbor), for her helpful comments on an earlier draft. None of the aforementioned individuals in this acknowledgment received compensation for their contributions.
Funding/Support: The NSAL is supported by the National Institute of Mental Health (U01-MH57716) with supplemental support from the Office of Behavioral and Social Science Research and the National Institute on Drug Abuse at the National Institutes of Health and the University of Michigan. Dr Joe was supported by grant K01-MH65499 from the National Institute of Mental Health. Dr Neighbors was supported by the Health Policy Scholars Award from the Robert Wood Johnson Foundation.
Role of the Sponsors: None of the sponsoring organizations had any involvement in the design and conduct of study; in the collection, management, analysis, or interpretation of data; or preparation, review, or approval of the manuscript.
Collaborating NSAL Investigators include James S. Jackson, PhD (principal investigator, Institute for Social Research, University of Michigan, Ann Arbor), Harold W. Neighbors, PhD (coprincipal investigator, School of Public Health and Institute for Social Research, University of Michigan, Ann Arbor), Robert J. Taylor, PhD (coprincipal investigator, School of Social Work, University of Michigan, Ann Arbor), Cleopatra H. Caldwell, PhD (University of Michigan, Ann Arbor), Linda M. Chatters, PhD (University of Michigan, Ann Arbor), Randolph Nesse, MD (University of Michigan Medical School, Ann Arbor), and David R. Williams, PhD (Harvard University, Boston, Mass).
Footnotes
Financial Disclosures: None reported.
Additional Information: The full text of all NSAL instruments can be found at http://www.rcgd.isr.umich.edu/prba/survey.htm.
Reprints/E-prints reprints@ama-assn.org
REFERENCES
- 1.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 2.Anderson RN, Smith BL. Hyattsville, Md: National Center for Health Statistics; Deaths: Leading Causes for 2001. 2003;52(9) [PubMed]
- 3.Centers for Disease Control and Prevention. [Accessed September 29, 2006];Webbased injury statistics query and reporting system. http://www.cdc.gov/ncipc/wisqars.
- 4.Hoyert DL, Heron M, Murphy SL, Kung HC. Hyattsville, Md: National Center for Health Statistics; Deaths: Final Data for 2003. National Vital Statistics Reports; April 19, 2006. 2006;54(13) [PubMed]
- 5.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: Institute of Medicine, National Academies Press; 2002. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Suicide among African-American youths—United States, 1980–1995. MMWR Morb Mortal Wkly Rep. 1998;47:193–196. [PubMed] [Google Scholar]
- 7.US Public Health Service. Washington, DC: US Public Health Service; The Surgeon General’s Call to Action to Prevent Suicide, 1999. 2000
- 8.Eaton DK, Kann L, Kinchen S, et al. Youth Risk Behavior Surveillance–United States, 2005. SS05. Vol. 55. Atlanta, Ga: Centers for Disease Control and Prevention; 2006. pp. 1–108. [PubMed] [Google Scholar]
- 9.Griffith EE, Bell CC. Recent trends in suicide and homicide among blacks. JAMA. 1989;262:2265–2269. [PubMed] [Google Scholar]
- 10.Joe S, Kaplan MS. Suicide among African American men. Suicide Life Threat Behav. 2001;31 suppl:106–121. doi: 10.1521/suli.31.1.5.106.24223. [DOI] [PubMed] [Google Scholar]
- 11.Garlow SJ, Purselle D, Heninger M. Ethnic differences in patterns of suicide across the life cycle. Am J Psychiatry. 2005;162:319–323. doi: 10.1176/appi.ajp.162.2.319. [DOI] [PubMed] [Google Scholar]
- 12.Joe S, Marcus SC. Datapoints: trends by race and gender in suicide attempts among U.S. adolescents, 1991–2001. Psychiatr Serv. 2003;54:454. doi: 10.1176/appi.ps.54.4.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Census Bureau. [Accessed January 23, 2006];US interim projections by age, sex, race, and hispanic origin. http://www.census.gov/ipc/www/usinterimproj/.
- 14.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 15.US Public Health Service. Rockville, Md: US Dept of Health and Human Services; National Strategy for Suicide Prevention: Goals and Objectives for Action. 2001 [PubMed]
- 16.Bell CC, Clark DC. Adolescent suicide. Pediatr Clin North Am. 1998;45:365–380. doi: 10.1016/s0031-3955(05)70012-2. [DOI] [PubMed] [Google Scholar]
- 17.Maris RW, Berman AL, Silverman MS. Comprehensive Textbook of Suicidology. New York, NY: Guilford Press; 2000. [Google Scholar]
- 18.Moscicki EK. Epidemiology of suicidal behavior. Suicide Life Threat Behav. 1995;25:22–35. [PubMed] [Google Scholar]
- 19.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 20.Kessler RC, Borges G, Walters EE. Prevalence of risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 21.Moscicki EK, O’Carroll P, Rae DS, Locke BZ, Roy A, Regier D. Suicide attempts in the Epidemiologic Catchment Area Study. Yale J Biol Med. 1988;61:259–268. [PMC free article] [PubMed] [Google Scholar]
- 22.Pennell BE, Bowers A, Carr D. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. Int J Methods Psychiatr Res. 2004;13:241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jackson JS, Torres M, Caldwell CH, et al. The National Survey of American Life. Int J Methods Psychiatr Res. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 4th ed. [Accessed June 29, 2006]. http://www.aapor.org/pdfs/standarddefs_4.pdf. [Google Scholar]
- 26.Little RJA, Rubin DB. Statistical Analysis with Missing Data. 2nd ed. New York: John Wiley and Sons; 2002. [Google Scholar]
- 27.Kish L. A procedure for objective respondent selection with the household. J Am Stat Assoc. 1949;44:380–387. [Google Scholar]
- 28.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 30.WHO World Mental Health Survey Consortium. The prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 31.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication. [Accessed October 9, 2006];Int J Methods Psychiatr Res. 2004 13:60–68. doi: 10.1002/mpr.166. http://www.hcp.med.harvard.edu/ncs/ftpdir/Kessler%20Merikangas%20NCSRbackgroundaims.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.United States Census Bureau. [Accessed September 9, 2005];Census regions and divisions of the United States. http://www.census.gov/geo/www/us_regdiv.pdf.
- 33.SAS Institute. SAS/STAT User’s Guide, Version 9.1. Cary, NC: SAS Institute, Inc; 2005. [Google Scholar]
- 34.Hosmer DW, Lemeshow S. Applied Survival Analysis: Regression Modeling of Time to Event Data. New York, NY: John Wiley & Sons, Inc; 2000. [Google Scholar]
- 35.Kovar JG, Rao JNK, Wu CFJ. Bootstrap and other methods to measure error in survey estimates. Can J Stat. 1988;16 suppl:25–45. [Google Scholar]
- 36.Benjamini Y, Hochberg Y. Controlling the false discovery rate. J R Stat Soc Series B (Method) 1995;57:289–300. [Google Scholar]
- 37.Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Statist. 2001;29:1165–1188. [Google Scholar]
- 38.Institute of Medicine. Reducing Suicide: A National Imperative. Washington, DC: National Academy Press; 2002. [Google Scholar]
- 39.Garlow SJ. Age, gender, and ethnicity differences in patterns of cocaine and ethanol use preceding suicide. Am J Psychiatry. 2002;159:615–619. doi: 10.1176/appi.ajp.159.4.615. [DOI] [PubMed] [Google Scholar]
- 40.Hawton K. Studying survivors of nearly lethal suicide attempts. Suicide Life Threat Behav. 2001;32 suppl:76–84. doi: 10.1521/suli.32.1.5.76.24215. [DOI] [PubMed] [Google Scholar]
- 41.Shaffer D, Gould M, Hicks RC. Worsening suicide rate in black teenagers. Am J Psychiatry. 1994;151:1810–1812. doi: 10.1176/ajp.151.12.1810. [DOI] [PubMed] [Google Scholar]
- 42.Gibbs JT. Conceptual, methodological, and structural issues in black youth suicide. Suicide Life Threat Behav. 1988;18:73–89. doi: 10.1111/j.1943-278x.1988.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 43.Gibbs JT. African-American suicide. Suicide Life Threat Behav. 1997;27:68–79. [PubMed] [Google Scholar]
- 44.Joe S. Implications of focusing on black youth self-destructive behaviors instead of suicide when designing preventative interventions. In: Romer D, editor. Reducing Adolescent Risk: Toward an Integrated Approach. Thousand Oaks, Calif: SAGE Publications; 2003. pp. 325–332. [Google Scholar]
- 45.Willis LA, Coombs DW, Drentea P, Cockerham WC. Uncovering the mystery. Suicide Life Threat Behav. 2003;33:412–429. doi: 10.1521/suli.33.4.412.25230. [DOI] [PubMed] [Google Scholar]
- 46.Nisbet PA. Protective factors for suicidal black females. Suicide Life Threat Behav. 1996;26:325–341. [PubMed] [Google Scholar]
- 47.Slap GB, Vorters DF, Chaudhuri S, Centor RM. Risk factors for attempted suicide during adolescence. Pediatrics. 1989;84:762–772. [PubMed] [Google Scholar]
- 48.Shaffer D, Gould M, Fisher P, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53:339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- 49.Ialongo N, McCreary BK, Pearson JL, et al. Suicidal behavior among urban, African American young adults. Suicide Life Threat Behav. 2002;32:256–271. doi: 10.1521/suli.32.3.256.22176. [DOI] [PubMed] [Google Scholar]
- 50.Regier DA, Narrow WE. Defining clinically significant psychopathology with epidemiologic data. In: Helzer JE, Hudiak JJ, editors. Defining Psychopathology in the 21st Century: DSM-V and Beyond. Washington, DC: American Psychopathological Association; 2002. pp. 19–30. [Google Scholar]
- 51.Wakefield J, Spitzer R. Why requiring clinical significance does not solve epidemiology’s and DSM’s validity problem: response to Regier and Narrow. In: Helzer JE, Hudiak JJ, editors. Defining Psychopathology in the 21st Century: DSM-V and Beyond. Washington, DC: American Psychopathological Association; 2002. [Google Scholar]
- 52.First MB, Spitzer RL, Gibbon M, Williams JBW, editors. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) New York: New York Psychiatric Institute; 2002. [Google Scholar]