Abstract
Objective
To evaluate the impact of advanced pharmacy practice experiences (APPEs) on doctor of pharmacy (PharmD) students' readiness for self-directed learning.
Methods
The Self-Directed Learning Readiness Scale (SDLRS) was administered to students prior to and after completing their APPEs. SDLRS is a validated instrument that determines the relative degree to which students have the attitudes and motivation to engage in self-directed learning.
Results
Seventy-seven (64%) students completed the SDLRS prior to starting their APPEs and 80 (67%) students completed the instrument after completing their APPEs. Forty-six (38%) students completed both. Prior to starting their APPEs, 74% of students scored greater than 150 on the SDLRS, indicating a high level of readiness for self-directed learning. No significant difference was found between the mean scores of students who took the SDLRS both prior to (159 ± 20) and after completing their APPEs (159 ± 24; p > 0.05).
Conclusion
Students at our institution appear to be ready for self-directed learning but APPEs had a minimal impact on their readiness for self-directed learning.
Keywords: self-directed learning, advanced pharmacy practice experiences, self-directed learning readiness scale, assessment
INTRODUCTION
The 2007 Accreditation Standards and Guidelines adopted by the Accreditation Council for Pharmacy Education (ACPE) acknowledges the need for pharmacy students to become self-directed lifelong learners.1 Doctor of pharmacy curriculums are required to incorporate instructional methodology that will assist pharmacy students in developing the skills needed for lifelong learning.1 Self-directed learning is thought to promote lifelong learning and is built upon andragogical principles describing adult learners as self-directed, intrinsically motivated, and goal-oriented.2 Malcolm Knowles defines self-directed learning as:
…a process in which individuals take the initiative, with or without the help of others, in diagnosing their learning needs, formulating learning goals, identifying human and material resources for learning, choosing and implementing appropriate learning strategies, and evaluating learning outcomes.3(p18)
Garrison further expanded the self-directed learning model to include 3 interrelated dimensions known as self-monitoring, self-management, and motivation.4 Constructivism describes learning as the acquisition, organization, modification, and incorporation of information into existing or new mental schemes.5 Self-monitoring refers to students' ability to monitor the knowledge construction process, which requires skills in self-regulation, metacognition, and reflection.4-7 For example, students need to be able to implement appropriate learning strategies to acquire information (eg, self-regulation), recognize whether the information has been learned (eg, metacognition), and determine whether the new information fits within an existing mental scheme or a new one is needed (eg, reflection). Self-management refers to students' ability to implement their learning goals and manage learning resources.4 Self-management requires a collaborative learning environment in which students have some external control of their tasks.4,8 Motivation for self-directed learning involves both intrinsic and extrinsic components. Self-directed students have a desire to learn and believe they are capable of learning.9 Furthermore, the learning task needs to be of value to them and students need to assume responsibility for task completion.4
Self-directed learning is discussed in Standard 11 as well as Guideline 11.1 of the 2007 ACPE Accreditation Standards and Guidelines, which explicitly state that pharmacy students must transition from dependent to active, self-directed, lifelong learners.1 From a curricular perspective, APPEs occur after pharmacy students have completed all of their didactic coursework. Prior to their fourth year of study, the majority of instruction occurs in formal environments in which the educator decides the learning objectives and activities of the course with little input from pharmacy students. Beardsley and colleagues proposed a target student-to-faculty ratio of 10:1 to meet the future demands of faculty members within pharmacy education.10 Even if this target student-to-faculty ratio is attained, the customization of classroom learning experiences based on individual pharmacy student's prior knowledge and learning needs is difficult. However, the learning environment and the student-to-faculty ratio are more favorable for self-directed learning during APPEs. During APPEs, learning becomes more problem-oriented and relevant. Moreover, pharmacy students have more control over their learning in this environment. According to a survey of colleges and schools of pharmacy conducted in 2004, a majority of the institutions reported a student-to-preceptor ratio between 1:1 to 4:1 ratio.11 By supervising only a few pharmacy students at a time, there is a greater possibility for the preceptor to customize the learning experience based on the needs of individual students. For example, Slevin and Lavery suggest that faculty members develop a one-on-one relationship with nursing students and supervise no more than 12 students in order to provide adequate support for self-directed learning.12 Using a problem-based learning approach to develop self-directed lifelong learners, the Graduate School of Medicine at the University of Queensland assigns 5 students per clinical coaching session to allow the students to pursue their own learning objectives.13 Although these examples are not specific to experiential education, the development of a close relationship between preceptor and pharmacy student is important to foster the self-directed learning process. Given the variety of practice settings available, APPEs offer pharmacy students more flexibility in terms of the learning objectives and activities and greater opportunities to engage in self-directed learning. As such, it is important to evaluate pharmacy students' readiness to engage in self-directed learning during APPEs.
All adult learners should be capable of engaging in self-directed learning.2 Thus, all pharmacy students should exhibit some degree of self-directedness, but some pharmacy students may be more self-directed than others. The Self-Directed Learning Readiness Scale (SDLRS) measures “the degree the individual possesses the attitudes, abilities, and personality characteristics necessary for self-directed learning.”14(p517) There are 2 versions of the SDLRS; one developed by Guglielmino in 1977 and another developed by Fisher, King, and Tague in 2001.14-15 Both instruments were developed independently and used the Delphi technique to generate items for the scale. Guglielmino originally piloted the instrument in high school students, college undergraduates, and individuals in evening enrichment classes to establish the instrument's reliability and to identify its 8 underlying factors via principal component factor analysis.15 Fisher and colleagues piloted their SDLRS instrument in nursing students.14 The internal reliability of the Fisher SDLRS instrument was demonstrated (Cronbach's alpha = 0.92).14 The authors chose to use the Fisher SDLRS instrument because it is linked to the underlying components of Garrison's self-directed learning model (eg, self-management, self-control, and desire for learning) and its construct validity was determined by principal component factor analysis.4,14 For example, the self-control factor includes 15 items related to setting personal goals, evaluating one's performance, and being aware of one's limitations, which corresponds to the self-regulatory and metacognitive skill set described by the self-monitoring dimension. The self-management factor contains 13 items related to time management, information management, and learning plan development. The desire for learning factor contains 12 items related to intrinsic motivation for self-directed learning.
Both the Guglielmino and Fisher SDLRS instruments have been used by other investigators to evaluate the self-directedness of healthcare professionals and students. When examining the readiness of third-year medical students to engage in self-directed learning utilizing the Guglielmino SDLRS instrument, medical students demonstrated an “above average” readiness for self-directed learning compared to adult learners in the general population.16 Byrd and colleagues determined the mean SDLRS score of first-year pharmacy students to be similar to the general population as well.17 Furthermore, a positive correlation was established between the medical students' scores on the SDLRS and preceptor evaluations during clinical rotations.16 When the Fisher SDLRS instrument was used to examine the readiness of practicing nurses to engage in self-directed learning, the majority demonstrated a “high level” of readiness for self-directed learning.18 However, the readiness of nursing students for self-directed learning varies substantially between schools and degree programs.19 Some students may not be as self-directed; therefore, teaching methods that enable students to develop the knowledge, skills, and attitudes necessary to engage in self-directed learning should be utilized.
The readiness of pharmacy students to engage in self-directed learning during experiential education has not been reported in the literature. The primary objective of this study was to evaluate the impact of APPEs on students' readiness for self-directed learning. Secondary objectives were to measure the self-directedness of pharmacy students and to determine whether specific student characteristics are associated with higher levels of readiness for self-directed learning.
METHODS
During their third year, a convenience sample of 120 PharmD students from the class of 2008 were invited to voluntarily complete a questionnaire regarding their “learning habits” prior to a mandatory orientation session regarding their APPEs. Students were permitted to anonymously complete the SDLRS instrument. However, those students who were willing to participate in the primary analysis were asked to identify themselves on the questionnaire using their 4-digit University-assigned personal identification number (PIN). This study was approved by the Institutional Review Board at the University of Maryland, Baltimore.
The questionnaire was self-administered and consisted of 2 sections: the Self-Directed Learning Readiness Scale (SDLRS) developed by Fisher and colleagues and a Baseline Characteristics Survey. The Fisher SDLRS instrument contains 40 statements and uses a 5-point Likert scale anchored at 1 = strongly disagree and 5 = strongly agree.14
The 10-item Baseline Characteristics Survey was designed to collect information regarding characteristics that might influence a student's readiness for self-directed learning, including general demographics, prepharmacy coursework, elective interests, and leadership experiences during the PharmD program. Pharmacy students at the University of Maryland School of Pharmacy (UMSOP) have the option, but are not required, to pursue an elective pathway (a course of study intended to prepare them for specific careers in pharmacy). These pathways include: advanced pharmacy practice, geriatric pharmacy practice, management, pharmacotherapy, and research.
The pharmacy students were required to complete 4 full-time 4-week required APPEs and 3 elective APPEs beginning the summer after their third year. During the required APPEs, pharmacy students provided patient-centered care to a variety of patients in different clinical settings under the supervision of an experienced preceptor. Pharmacy students were expected to demonstrate proficiency in data collection, assessment of drug-related problems, development of pharmaceutical care plans, provision of patient education, and documentation of patient outcomes. They had to demonstrate their knowledge, skills, and ability to manage patients who were diagnosed with 1 or more of the 25 core disease states commonly encountered in pharmacy practice. For each APPE, pharmacy students were asked to self-assess their ability to manage patients with these 25 core disease states at the beginning, middle, and end of the experience. They were also asked to maintain a portfolio of all written assignments and evaluation forms. Preceptors were not required to verify students' self-assessments or review students' portfolios.
During their fourth year after completion of all required APPEs, pharmacy students in the class of 2008 again were asked to voluntarily complete the SDLRS questionnaire on the first day of a required didactic seminar. At that time, students were asked to identify their questionnaire using their campus identification number assigned to them by the University since their personal identification numbers were no longer valid. During each session in which the questionnaire was administered, the principal investigator entered the classroom, described the general premise of the study, and distributed the questionnaires. Students were given 30 minutes to complete and return the questionnaire. Completed questionnaires identified by student PIN were matched to questionnaires identified by campus identification number using information obtained from the Office of Student Affairs.
Pharmacy students' scores on the SDLRS prior to the start of APPEs (pre-APPEs) and after APPEs (post-APPEs) were compared using descriptive statistics. The paired t test and McNemar's test were used to compare changes in individual student's scores on SDLRS pre-APPEs and post-APPEs. The authors considered a 15-point change in the SDLRS score to be potentially meaningful based on data from the class of 2007 indicating a 15-point average score difference on the SDLRS between the first and second quartiles and the third and fourth quartiles. Based on this assumption, 16 students' scores were required to detect a 15-point change in SDLRS scores pre- and post-APPEs with β = 0.80 and α = 0.05. Categorical data between groups were analyzed using the Fisher exact test. P values < 0.05 were considered significant. Data analysis was performed using SAS, version 9.1 (SAS Institute, Cary, NC).
RESULTS
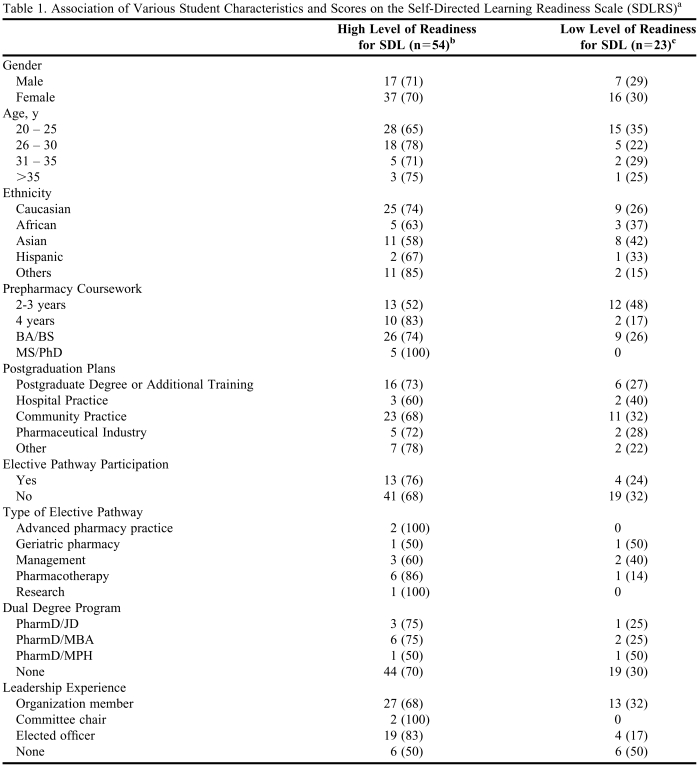
Of the 120 eligible pharmacy students in the class of 2008, 77 (64%) and 80 (67%) students completed the questionnaire in the third and fourth year respectively. Of these respondents, 46 (38%) matched pairs completed the questionnaire in both years and were included in the primary analysis. The baseline characteristics of the 77 participants who completed the questionnaire in the third year are shown in Table 1. None of the baseline characteristics, such as gender, age, ethnicity, prepharmacy coursework, postgraduation plans, elective pathway, participation in a dual degree program, or leadership experiences, were associated with high SDLRS scores (Table 1). Scores greater than 150 on the SDLRS indicated a high level of readiness for self-directed learning, while scores less than or equal to 150 on the SDLRS indicated a lower level of readiness for self-directed learning.14
Table 1.
Association of Various Student Characteristics and Scores on the Self-Directed Learning Readiness Scale (SDLRS)a
Abbreviations: SDL = self-directed learning; BA = bachelor of arts; BS = bachelor of science; MS = master of science; PhD = doctor of philosophy; PharmD = doctor of pharmacy; JD = juris doctor; MBA = master of business administration; MPH = master of public health.
Data includes the entire cohort of pharmacy students in the Class of 2008 who complete the questionnaire in their third year. None of the comparisons were found to be significant using the two tailed Fisher exact test at a level of significance of p < 0.05.
b High level of readiness for self-directed learning defined as scores greater than 150 on the SDLRS with a maximum score of 200.
c Low level of readiness for self-directed learning defined as scores less than or equal to 150 on the SDLRS.
The overall mean SDLRS score for the pharmacy students who completed the questionnaire in the third year and fourth year were 157 ± 21 (range: 61-196; n=77) and 162 ± 21 (range: 66-197; n=80) respectively. Prior to starting their APPEs, 70% of the students scored greater than 150 on the SDLRS, indicating a high level of readiness for self-directed learning. Eighty-one percent of the students scored greater than 150 on the SDLRS after completing their required APPEs. No difference was found between mean scores on the SDLRS for students in their third and fourth years (p > 0.05).
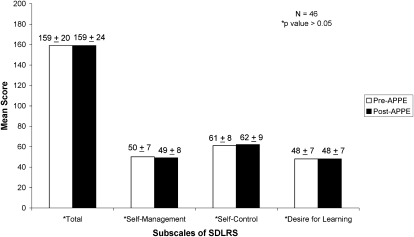
In the primary analysis that included 46 pharmacy students, the mean pre-APPEs and post-APPEs SDLRS scores were 159 ± 20 (range: 84-188) and 159 ± 24 (range: 66-195), respectively. No difference was found between the mean scores for the matched pairs (p = 0.97). Of these 46 students, 35 (76%) did not have a meaningful change in their SDLRS score, while 6 students (13%) had a meaningful improvement in their SDLRS score, and 5 students (11%) had a meaningful decline in their SDLRS score. Of the 6 students who had a meaningful improvement in their SDLRS score, 4 scored less than 150 on their SDLRS prior to their APPEs. Applying the McNemar's test, no significant difference was found between the percentage of students who scored greater than 150 on the SDLRS prior to or after APPEs (74% vs. 78%, respectively, p = 0.74).
The SDLRS is composed of 3 underlying subscales: self-management, self-control, and desire for learning.14 Figure 1 displays the changes in the mean scores for the total score and the 3 subscales of the SDLRS instrument prior to and after APPEs. No significant difference was found between the mean scores for all 3 subscales (p > 0.05). The median scores on the subscales pre- and post-APPEs were as follows: self-management, 52 vs. 50; self-control, 62 vs. 63; and desire for learning 49 vs. 49.
Figure 1.
The maximum score on the Self-Directed Learning Readiness Scale (SDLRS) is 200. The self-management subscale contains 13 items with a maximum score of 65 and a minimum score of 13. The self-control subscale contains 15 items with a maximum score of 75 and a minimum score of 15. The desire for learning subscale contains 12 items with a maximum score of 60 and a minimum score of 12. Changes in the mean score before and after advanced pharmacy practice experiences (APPEs) were not significant for the total and each subscale as determined by the paired t test.
DISCUSSION
The need for healthcare professionals to become lifelong learners seems inherently important because biomedical knowledge is rapidly expanding and practitioners must maintain competency throughout their careers. As such, instructional methodologies within the curriculum that facilitate the development of lifelong learners are recommended by various accrediting bodies for healthcare professional education programs.1,20-21 Self-directed learning strategies may facilitate the development of lifelong learners.2-3 Factors that can influence the engagement of learners in self-directed learning activities include: their innate propensity for self-directed learning, their familiarity with the subject matter, the possession of self-directed learning skills, and their motivation for self-directed learning.22 This study demonstrated that a majority of pharmacy students at UMSOP exhibit a high degree of readiness for self-directed learning, which suggest that they have the attitudes, abilities, and characteristics that are required for self-directed learning. The mean SDLRS score of the pharmacy students in our study were slightly higher than the mean SDLRS scores reported for a group of nursing students enrolled in a bachelor of nursing program (151 ± 18).14 Moreover, a greater percentage of fourth-year pharmacy students (81%) exhibited a high level of readiness for self-directed learning compared to the nursing students (50%).14 Although fourth-year pharmacy students exhibited a greater degree of readiness for self-directed learning, 19% had a low level of readiness for self-directed learning. This suggests that a substantial cohort of pharmacy students may not be prepared to become lifelong learners as pharmacists. When the SDLRS was administered to 33 nurses in a continuing education program, the mean score on the SDLRS was 167 ± 12, and a smaller percentage (8%) of nurses exhibited a low level of readiness for self-directed learning.18 Since practicing nurses conduct most of their learning in an informal learning environment to maintain their competency, not surprisingly, only a small percentage scored low on this scale. The readiness of practicing pharmacists to engage in self-directed learning is not known.
Since some variation exists in students' readiness for self-directed learning, it is helpful to identify student characteristics that might be associated with high or low levels of readiness for self-directed learning so that instruction can be tailored to these students. This study found no associations between various student characteristics and high SDLRS scores. When investigating the association of various student characteristics with readiness for self-directed learning in medical students, Frisby determined that age was positively associated and that physical science majors were more likely to have higher scores on the SDLRS developed by Guglielmino.15,23 Since age was measured as a categorical rather than a continuous variable in this study, the effect of pharmacy students' age on their readiness for self-directed learning may have been mitigated. Although a baccalaureate degree is not a prerequisite for entrance into most colleges and schools of pharmacy, 52.5% of applicants in 2006-2007 had a baccalaureate degree.24 In our study, a prior bachelor's degree was not associated with higher SDLRS scores. The impact of additional years of postsecondary education on pharmacy students' readiness for self-directed learning needs to be further investigated.
According to the 2007 ACPE Accreditation Standards and Guidelines, experiential education should comprise at least 30% of the PharmD curriculum.1 Based on the findings of this study, APPEs have a negligible impact on students' readiness for self-directed learning at UMSOP. When comparing individual student SDLRS scores before and after APPEs, most pharmacy students did not have a meaningful change on the SDLRS. At the UMSOP, pharmacy students are required to conduct self-assessments and to maintain a portfolio of activities for the required APPEs. Since these activities are related to the self-management and self-control component of the SDLRS, it was anticipated that these components would increase after the completion of APPEs. However, no changes were observed in pharmacy students' scores on these 2 components before and after APPEs. Similarly, Harvey and colleagues, using the SDLRS instrument developed by Guglielmino, found no differences in the readiness for self-directed learning among first-, second-, third-, and fourth-year medical students.25 However, unlike our study, Harvey and colleagues did not follow the same cohort of students as they progressed through the curriculum. Walker and colleagues investigated the impact of a 16-week problem-based learning curriculum on pharmacy students' readiness for self-directed learning and found an 11-point decrease in students' mean SDLRS scores from baseline.26 To further investigate the impact of the doctor of pharmacy curriculum on the readiness of pharmacy students for self-directed learning, a cohort of pharmacy students should be followed from entrance into pharmacy school through graduation.
One of the factors that influence a learner's engagement in self-directed learning includes the possession of self-directed learning skills.22 Patterson and colleagues identified the following competencies for self-directed learning in nursing education: assessment of learning needs, self- and peer evaluation, reflection, information management, critical thinking, and critical appraisal.27 Currently, pharmacy students at the UMSOP during their APPEs are not provided instruction regarding how to conduct self-assessments or engage in reflective activities. To enhance students' readiness for self-directed learning, perhaps more time needs to be focused on the development of the competencies required for self-directed learning throughout the curriculum.
The educator and learning environment can also influence a learner's engagement in self-directed learning.3,12-13 To facilitate self-directed learning, educators should foster a partnership with students and help them assess their learning needs, develop specific learning objectives, locate appropriate learning resources, and identify suitable methods of evaluation.28 Educators should also be cognizant of their students' learning styles.3,28 In addition, the learning environment should have a variety of resources available for students to use and the resources should match the students' learning styles.28 At UMSOP, there are 491 advanced pharmacy practice preceptors located at 322 experiential learning sites (H.A. Truong, written communication, August 27, 2008). Given the large number of preceptors and sites, each fourth-year pharmacy student's APPEs would presumably be different. For example, some preceptors are more likely to review their students' self-assessments and portfolios at the beginning of the APPE and adjust activities to meet the needs of their students. Some experiential learning sites may have more learning resources available, such as computer access, library, and pharmacy residents, that may facilitate the learning process. All of these factors may have an influence on students' readiness for self-directing learning.
This study has several limitations. Although the response rate for both years were greater than 60%, the percentage of pharmacy students with matched pair data represented only 38% of the class of 2008. As such, the results of this investigation may have been affected by selection bias. However, no significant differences were observed between the 46 students who completed the questionnaire twice and the other students who completed the questionnaire once with regard to gender, age, ethnicity, pre-pharmacy coursework, postgraduation plans, elective pathway, participation in a dual degree program or leadership experiences. Nevertheless, the small number of pharmacy students within some subgroups may have limited the statistical power of this study to detect meaningful associations. The Self-Directed Learning Readiness Scale used in this investigation was originally developed for nursing students, a group which closely matches our study population since both involve students from healthcare professional education programs.14 Furthermore, the 3 subscale components identified (ie, self-management, self-control, and desire for learning) are also congruent with the model of self-directed learning proposed by Garrison.4,14 However, one major limitation of this instrument is that it has not been used extensively and evaluated by other investigators. We chose not to use the SDLRS developed by Guglielmino, which has been used more frequently by other investigators in the medical literature because questions have been raised in the literature regarding its construct validity.29-31 However, Delahaye and Choy conducted a review of Guglielmino SDLRS and determined it to be an appropriate method to measure readiness for self-directed learning.32 Another limitation of the SDLRS is the possibility of a ceiling effect that limits the ability of the scale to detect significant changes in readiness for self-directed learning among high scorers. Harvey and colleagues suspected a ceiling effect when examining the readiness of medical students for self-directed learning.25 Finally, this study investigated pharmacy students' readiness for self-directed learning and not actual participation in self-directed learning activities. To maintain one's competency, one must not only be ready to engage in self-directed learning but must actually implement it. To meet the 2007 ACPE Accreditation Standards and Guidelines, schools and colleges of pharmacy will need to develop an assessment plan to evaluate their curriculum's ability to foster skills required for self-directed lifelong learning.1 The Self-Directed Learning Readiness Scale may be a useful quantitative metric within a curriculum assessment plan. However, due to the multidimensional aspects of self-directed learning, qualitative methods, as well as new assessment criteria during didactic and experiential courses, also will be necessary to fully assess pharmacy students' ability to become self-directed lifelong learners.
CONCLUSION
Readiness for self-directed learning varied widely among the pharmacy students in our study, but a majority exhibited a high level of readiness for self-directed learning. Advanced pharmacy practice experiences appeared to have a minimal impact on students' readiness for self-directed learning at our institution. Explicit instruction regarding the self-directed learning process may be needed in pharmacy curricula in order to foster the development of self-directed lifelong learners.
REFERENCES
- 1. Accreditation Standards and Guidelines for Professional Programs in Pharmacy Leading to the Doctor of Pharmacy Degree. Adopted January 15, 2006. Released February 17, 2006. Effective July 1 2007. Accreditation Council for Pharmacy Education. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed March 25, 2009.
- 2.Knowles MS, Holton EF, III, Swanson RA. The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development. 6th ed. New York City, NY: Elsevier; 2005. [Google Scholar]
- 3.Knowles M. Self-directed learning. A Guide for Learners and Teachers. Cambridge, NY: Pearson Learning Cambridge Adult Education; 1975. [Google Scholar]
- 4.Garrison D. Self-directed learning: toward a comprehensive model. Adult Educ Q. 1997;48:18–34. [Google Scholar]
- 5.Ormrod JE. Human Learning. 5th ed. Upper Saddle River, NJ: Pearson/Merrill Prentice Hall; 2008. pp. 163–5. [Google Scholar]
- 6. Owen T. Self-Directed Learning in Adulthood: A Literature Review [e-book]; Ipswich, MA: ERIC; 2002. http://www.eric.ed.gov/ERICWebPortal/contentdelivery/servlet/ERICServlet?accno=ED461050. Accessed May 21, 2008.
- 7.Dunlap J, Grabinger S. Preparing students for lifelong learning: a review of instructional features and teaching methodologies. Performance Improvement Q. 2003;16(2):6–25. [Google Scholar]
- 8.Boekaerts M, Cascallar E. How far have we moved toward the integration of theory and practice in self-regulation? Educ Psychol Rev. 2006;18(3):199–210. [Google Scholar]
- 9.McCombs B. Motivation and lifelong learning. Educ Psychol. 1991;26(2):117–28. [Google Scholar]
- 10.Beardsley R, Matzke G, Rospond R, et al. Factors influencing the pharmacy faculty workforce. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice experience placements: a 5-year update. Am J Pharm Educ. 2005;69(3) Article 45. [Google Scholar]
- 12.Slevin OD, Lavery MC. Self-directed learning and student supervision. Nurs Educ Today. 1991;11(5):368–77. doi: 10.1016/0260-6917(91)90037-b. [DOI] [PubMed] [Google Scholar]
- 13.Miflin BM, Campbell CB, Price DA. A conceptual framework to guide the development of self-directed, lifelong learning in problem-based medical curricula. Med Educ. 2000;34(4):299–306. doi: 10.1046/j.1365-2923.2000.00564.x. [DOI] [PubMed] [Google Scholar]
- 14.Fisher M, King J, Tague G. Development of a self-directed learning readiness scale for nursing education. Nurs Educ Today. 2001;21(7):516–25. doi: 10.1054/nedt.2001.0589. [DOI] [PubMed] [Google Scholar]
- 15.Guglielmino LM. Athens: University of Georgia; 1977. Development of the Self-directed Learning Readiness Scale [thesis] [Google Scholar]
- 16.Shokar G, Shokar N, Romero C, Bulik R. Self-directed learning: looking at outcomes with medical students. Fam Med. 2002;34(3):197–200. [PubMed] [Google Scholar]
- 17.Byrd DC, Kompella UB, Taylor CT, Wadibia EC. Assessment of self-learning ability [abstract]. Podium and Poster Abstracts of the 99th Annual Meeting; 1998 July 18-22; Snowmass Village, Aspen, CO. Am J Pharm Educ. 1998;62(4):88S. [Google Scholar]
- 18.Newman M. London: Middlesex University; 2004. Problem Based Learning: An exploration of the method and evaluation of its effectiveness in a continuing nursing education programme [thesis] [Google Scholar]
- 19.O'Shea E. Self-directed learning in nurse education: a review of the literature. J Adv Nurs. 2003;43(1):62–70. doi: 10.1046/j.1365-2648.2003.02673.x. [DOI] [PubMed] [Google Scholar]
- 20. LCME Accreditation Standards (with annotations) [Updated June 2008]. Liaison Committee on Medical Education. http://www.lcme.org/functionslist.htm. Accessed June 17, 2009.
- 21. Accreditation Manual with Interpretive Guidelines by Program Type for Post Secondary and Higher Degree Programs in Nursing. 2006 Edition. National League for Nursing Accrediting Commission. http://www.nlnac.org/manuals/NLNACManual2006.pdf. Accessed June 17, 2009.
- 22.Artis A, Harris E. Self-directed learning and sales force performance: an integrated framework. J Personal Selling Sales Manage. 2007;27(1):9–24. [Google Scholar]
- 23.Frisby AJ. Columbus, OH: The Ohio State University; 1991. Self-directed Learning Readiness in Medical Students at the Ohio State University [thesis] [Google Scholar]
- 24. Profile of Pharmacy Students Fall 2007. American Association of Colleges of Pharmacy. http://www.aacp.org/resources/research/institutionalresearch/Documents/07Introduction.pdf. Accessed June 17, 2009.
- 25.Harvey BJ, Rothman AI, Frecker RC. Effect of an undergraduate medical curriculum on students' self-directed learning. Acad Med. 2003;78:1259–65. doi: 10.1097/00001888-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 26. Walker JT, Lofton SP. Effect of a problem based learning curriculum on students' perception of self-directed learning. Issues Educ Res. 2003;13:71-100. http://www.iier.org.au/iier13/walker.html. Accessed March 25, 2009.
- 27.Patterson C, Crooks D, Lunyk-Child O. A new perspective on competencies for self-directed learning. J Nurs Educ. 2002;41(1):25–31. doi: 10.3928/0148-4834-20020101-06. [DOI] [PubMed] [Google Scholar]
- 28. Lowry CM. Supporting and Facilitating Self-Directed Learning. ERIC Digest No. 93 [e-book]. Columbus, OH: ERIC Clearinghouse on Adult Career and Vocational Education; 1989. http://www.eric.ed.gov/ERICWebPortal/contentdelivery/servlet/ERICServlet?accno=ED312457. Accessed April 18, 2007.
- 29.Bonham L. Guglielmino's self-directed learning readiness scale: what does it measure? Adult Educ Q. 1991;41(2):92–9. [Google Scholar]
- 30.Field L. An investigation into the structure, validity, and reliability of Guglielmino's self-directed learning readiness scale. Adult Educ Q. 1989;39(3):125–39. [Google Scholar]
- 31.Field L. Guglielmino's self-directed learning readiness scale: should it continue to be used? Adult Educ Q. 1991;41(2):100–3. [Google Scholar]
- 32.Delahaye B, Choy S. The Learning Preference Assessment. In: Maltby J, editor. Commissioned Reviews of 250 Psychological Tests. Vol. 2. Lewiston, NY: E. Mellen Press; 2000. pp. 857–64. [Google Scholar]