Abstract
Three cases of human infection by Trichinella spiralis were first confirmed by detecting encysted larvae in the biopsied muscle in December 1997, in Korea. The patients were one 35- and two 39-year-old males residing in Kochang-gun, Kyongsangnam-do. They had a common past history of eating raw liver, spleen, blood and muscle of a badger, Meles meles melanogenys, and complained of high fever, facial and periorbital edema, and myalgia. Hematologic and biochemical examinations revealed leukocytosis and eosinophilia, and highly elevated levels of GOT, GPT, LDH and CPK. In the gastrocnemius muscle of a patient, roundly coiled nematode larvae were detected. The larvae measured 0.775-1.050 (av. 0.908) mm in length, and 0.026-0.042 (av. 0.035) mm in maximum width. The specific IgG antibody levels in three patients' sera were significantly higher when compared with those of normal controls. The patients were treated with flubendazole and albendazole for 15-30 days, and discharged at 13-34 days post-admission. From the above findings, it was confirmed that T. spiralis is present in Korea, and the badger plays a role of as the natural host.
Keywords: epidemiology, Trichinella spiralis, Korea, human, badger
Trichinosis is one of the most widespread helminthic zoonoses. Unlike other parasite infections, it has been the main public health problem in advanced countries where there is a great amount of meat consumption such as European countries and USA. This nematode infection has been reported in all of the continents except Australia (Despommier, 1998). Due to the widespread of trichinosis in many Asian countries including China and Japan (Yamaguti, 1989; Miyazaki, 1991), it has been suspected to be prevalent in Korea for a long time. However, trichinosis had not been reported in Korea until 1997. In December 1997, the first human infection with Trichinella spiralis was confirmed by detecting encysted larvae in the biopsied muscle.
A 35- and two 39-year-old men residing in Kochang-up were admitted to Seokyong Hospital in Kochang-gun, Kyongsangnam-do on December 4, 1997. They chiefly complained of high fever, facial and periorbital edema, and myalgia, and had a common past history of eating raw liver, spleen, blood and muscle of a badger, Meles meles melanogenys. They mentioned that the severe symptoms such as abdominal pain, watery diarrhea, high fever, chill, headache, facial and periorbital edema, general pain, and myalgia, appeared 3-14 days after eating a badger.
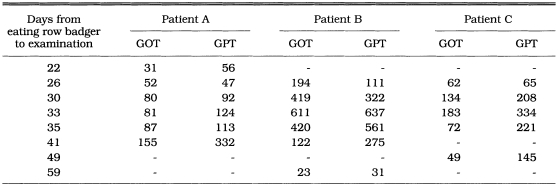
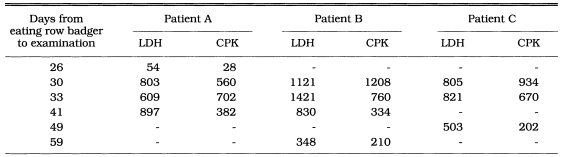
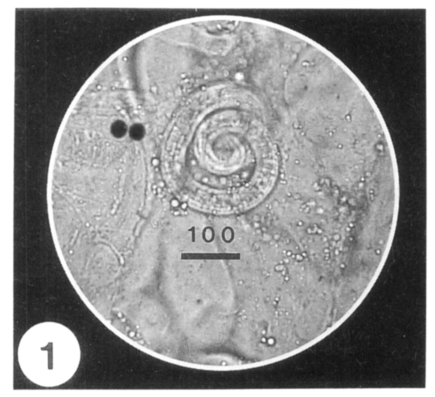
Hematologic examinations performed at 26, 30, 33 and 35 days after infection revealed eosinophilia (2-19%, 7-16% and 0-6% in each patients) and leukocytosis (18,000, 26,550 and 12,500/mm3 in average). Biochemical examinations showed highly elevated levels of GOT, GPT, LDH (lactic dehydrogenase) and CPK (creatine phosphokinase) (Table 1, 2). Becuase the symptoms and the laboratory findings were highly suggestive of trichinosis, muscle biopsy was performed to verify it. The biopsied muscles were examined by the pressure method using two slide glasses. Roundly coiled nematode larvae were detected in the gastrocnemius muscle of a patient at 34 days after eating raw badger flesh (Fig. 1). Larvae were measured to be 0.775-1.050 (0.908 in average) mm in length, and 0.026-0.042 (0.035 in average) mm in the maximum width. In sectioned specimen of the biopsied muscle, the worm cyst was surrounded by numerous inflammatory cells and a nurse cell-larva complex was observed (Figs. 2, 3).
Table 1.
Results of the biochemical examination on GOTa) and GPTb)
a)normal value, 3-40 unit; b)normal value, 5-35 unit.
Table 2.
Results of the biochemical examination on LDHa) and CPKb)
a)normal value, 50-400 unit; b)normal value, 5-50 unit.
Fig. 1.
A coiled Trichinella spiralis larva in the biopsied gastrocnemius muscle of a patient at 34 days after eating raw badger.
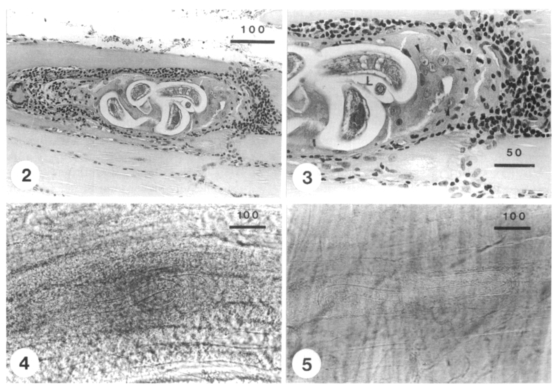
Figs. 2-5.
Larvae of Trichinella spiralis detected from muscle biopsy of the patient.
Fig. 2. A sectioned larva in the worm cyst of muscle biopsied at 34 days after infection (H-E stained). Fig. 3. Enlarged view of Fig. 2, showing the intense inflammatory response around the nurse cells (arrow heads)-larva (L) complex (H-E stained). Figs. 4 & 5. Two larvae in press preparation of muscle biopsyed at 41 days after eating raw badger (at 10 days after treatment with flubendazole and albendazole). The larvae detected at the same day were uncoiled and did not show the infectivity in mice and a hamster. The bar represents µm in length.
The muscle biopsied at 34 days after eating raw badger was artificially digested with pepsin-HCl solution to investigate the intensity of infection. A total of 212 larvae per gram of muscle was recovered. The recovered larvae were given orally to a ICR mouse. At 50 days after experimental infection, a large number of larval T. spiralis was harvested from the mouse. However, after treatment with flubendazole for 7 days and with albendazole for 3 days, the larvae in biopsied muscle were uncoiled (Figs. 4, 5), and they did not infect four mice and a hamster experimentally
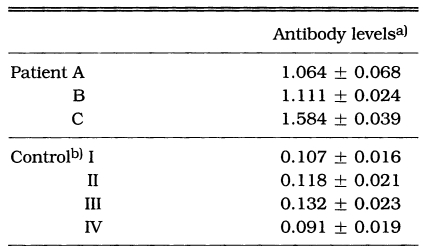
To alleviate symptoms, antibiotics and steroids were administered. Praziquantel, flubendazole and albendazole were also given orally to eradicate helminths. All patients were discharged at 13-34 days post-admission because most of symptoms disappeared. We measured the specific IgG antibody levels in three patients' sera sampled at 32 days after infection. The absorbances were measured by ELISA. As a normal control, the sera from four adults were used. The values were significantly higher when compared with those of normal controls (Table 3).
Table 3.
Specific IgG antibody levels in sera of three patients sampled at 32 days after infection
a)Absorbance were measured by ELISA. b)Control I: 40-year old male; II: 25-year old male; III: 23-year old female; IV: 22-year old female.
By the present study, it was confirmed for the first time that T. spiralis is distributed in Korea. This nematode infection has been found in humans and various mammals in many Asian countries such as Far East USSR, China, Japan, Tailand, Indonesia, Vietnam and Laos (Yamaguti, 1989). The presence of T. spiralis in Korea has been suspected for a long time; however, this nematode infection has not been reported before the present study.
The prevalence of human trichinosis in endemic countries cannot be estimated because there are no recent systematic surveys. However, sporadic outbreaks are still common in Spain, France, Italy, Yugoslavia, USA and Canada, and it recently occurred in China, Japan, and the Middle East (MacLean et al., 1989; Olaison and it Ljungstrom, 1992; Pozio et al., 1993; Dworkin et al., 1996). Especially, it is noteworthy that the recent incidence of human trichinosis in China (about 10,000 cases annually) is the highest in the world (Markell et al., 1999). The present study showed that an outbreak of trichinosis occurred in a nearby country of China.
Until recently, T. spiralis was the only human infecting species in the genus Trichinella. However, four other distinct species, i.e. T. pseudospiralis, T. britovi, T. nativa and T. nelsoni, have been recognized (Pozio et al., 1992). They can be distinguished from T. spiralis by the inability to form cysts, pathogenicity and regional medical importance. While T. spiralis is the most important species among these parasites in most part of the world due to the widespread distribution and higher pathogenicity, T. pseudospiralis does not form the worm cyst and is infectious to avian hosts. The remaining three species are of more regional importance (Markell et al., 1999). On the basis of the aforementioned characteristics, the nematode parasite isolated in this study was identified as T. spiralis.
Trichinosis is definitely diagnosed by the detection of larvae in the biopsied muscle. However, prior to diagnosis, past histories, manifesting symptoms and laboratory findings provide helpful information in making a decision before conducting a muscle biopsy (Despommier, 1998). Because the patients in this study showed symptoms and laboratory findings suggesting the trichinosis, and had a common past history of eating raw badger, muscle biopsy was undertaken for definite diagnosis.
A laboratory finging that is always associated with T. spiralis infection is eosinophilia in the blood examination (Gould, 1970). In severely infected cases, eosinophils may be as high as 80-95%. Overall, the total WBC count is slightly elevated. In patients moderately or severely infected with this nematode, muscle enzymes such as CPK and LDH are released into the circulating blood and their presence in the serum can be another clue to the diagnosis of trichinosis (Murrell and Bruschi, 1994; Capo and Despommier, 1996). In the present study, although eosinophilia was not so high, other laboratory findings such as leukocytosis and elevated enzyme levels were similar to those of previous reports.
ELISA can detect antibodies in some patients as early as 12 days after infection (Ljungstrom, 1983). In the present study, the specific IgG antibody levels were measured in three patients' sera sampled at 32 days after infection by the ELISA. The antibody levels were significantly higher than those of normal controls. Two out of three patients, who were larva negative in biopsied muscles, were serologically confirmed to be infected with T. spiralis.
It has been known that thiabendazole and mebendazole are useful for treatment against trichinosis (Miyazaki, 1991). Albendazole may be effective, but its role is not yet established (Markell et al., 1999). On the other hand, during an outbreak of T. pseudospiralis in Thailand, treatment with albendazole for 2 weeks was found to be effective, but administration of thiabendazole and mebendazole was ineffective (Jongwutiwes et al., 1998). The present cases were ultimately treated by flubendazole and albendazole from the 6th day after admission for 15-30 days. After treatment for 10 days, the larvae were uncoiled, and they did not show the infectivity in experimental animals. They were probably damaged by the antihelminthics, and lost their coilings and infectivities.
Footnotes
This work was supported by a research grant for basic medical sciences, Ministry of Education (1996-1998), Republic of Korea.
References
- 1.Capo V, Despommier DD. Clinical aspects of infection with Trichinella spp. Clin Microbiol Rev. 1996 Jan;:47–54. doi: 10.1128/cmr.9.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Despommier DD. Trichinella and Toxocara. In: Cox FEG, Kreier JP, Wakelin D, editors. Parasitology (Vol 5) of Topley & Wilson's Microbiology and Microbial Infections. 9th ed. London, UK: Arnold; 1998. pp. 597–602. [Google Scholar]
- 3.Dworkin MS, Gamble HR, Zarlenga DS, Tennican PO. Outbreak of trichinellosis associated with eating cougar jerky. J Infect Dis. 1996;174:663–666. doi: 10.1093/infdis/174.3.663. [DOI] [PubMed] [Google Scholar]
- 4.Gould SE. In: Clinical pathology: diagnostic laboratory procedures, Trichinosis in man and animals. Gould SE, Thomas CC, editors. Illinois, USA: Springfield; 1970. pp. 191–221. [Google Scholar]
- 5.Jongwutiwes S, Chantachum N, Kraivichian P, et al. First outbreak of human trichinellosis caused by Trichinella pseudospiralis. Clin Infect Dis. 1998;26:111–115. doi: 10.1086/516278. [DOI] [PubMed] [Google Scholar]
- 6.Ljungstrom I. In: Immunodiagnosis in man, Trichinella and trichinosis. Campbell WC, editor. New York, USA: Plenum Press; 1983. pp. 403–424. [Google Scholar]
- 7.MacLean JD, Viallet J, Law C, Staudt M. Trichinosis in the Canadian Arctic: report of five outbreaks and a new clinical syndrome. J Infect Dis. 1989;160:513–520. doi: 10.1093/infdis/160.3.513. [DOI] [PubMed] [Google Scholar]
- 8.Markell EK, John DT, Krotoski WA. Markell and Voge's Medical Parasitology. 8th ed. Philadelphia, USA: W.B. Saunders; 1999. pp. 340–345. [Google Scholar]
- 9.Miyazaki I. Helminthic Zoonoses. Tokyo, Japan: International Medical Foundation of Japan; 1991. pp. 452–459. [Google Scholar]
- 10.Murrell D, Bruschi F. Clinical trichinellosis. In: Tsien Sun., editor. Progress in Clinical Parasitology. Boca Raton: CRC Press; 1994. pp. 117–150. [PubMed] [Google Scholar]
- 11.Olaison L, Ljungstrom I. An outbreak of trichinosis in Lebanon. Trans Roy Soc Trop Med Hyg. 1992;86:658–660. doi: 10.1016/0035-9203(92)90178-f. [DOI] [PubMed] [Google Scholar]
- 12.Pozio E, La Rosa G, Murrell KD, Lichtenfels JR. Taxonomic revisions of the genus Trichinella. J Parasitol. 1992;78:654–659. [PubMed] [Google Scholar]
- 13.Pozio E, Varese P, Morales MA, Croppo GP, Pelliccia D, Bruschi F. Comparison of human trichinellosis caused by Trichinella spiralis and by Trichinella britovi. Am J Trop Med Hyg. 1993;48:568–575. doi: 10.4269/ajtmh.1993.48.568. [DOI] [PubMed] [Google Scholar]
- 14.Yamaguti T. Trichinella and trichinelliasis in Japan. Tokyo, Japan: NKD; 1989. [Google Scholar]