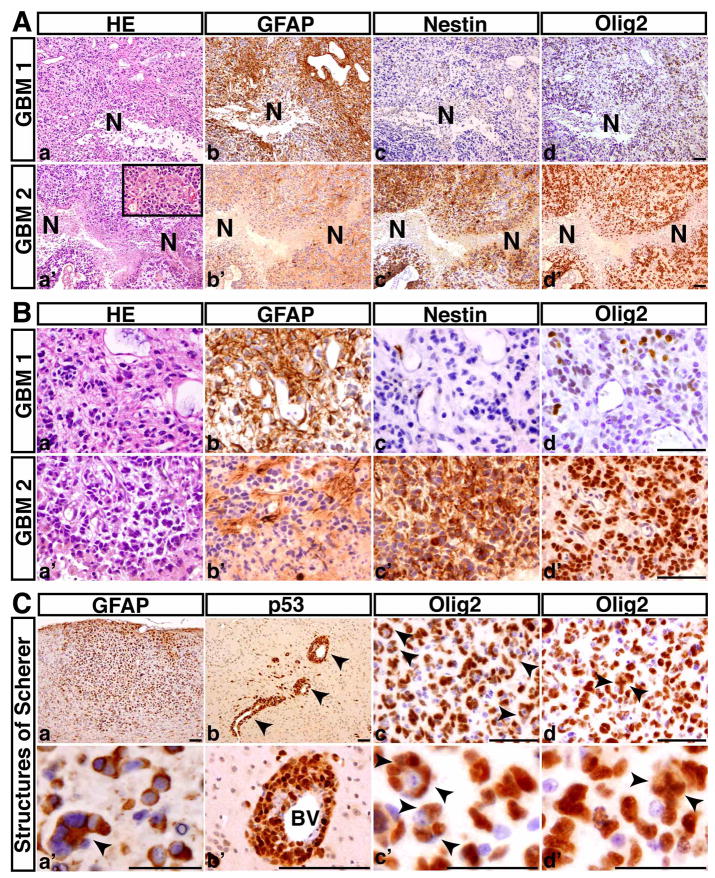
Figure 3. The p53ΔE5-6 mutant mice develop GBMs.
(A) Serial sections from two representative p53ΔE5-6 GBMs (GBM1, 2) were stained with H&E (a, a′), anti-GFAP (b, b′), anti-Nestin (c, c′), and anti-Olig2 (d, d′). N, necrosis. There are regions of coagulation necrosis (a–d), and pseudopalisades of malignant GBM cells adjacent to necrosis (a′-d′). The inset in (a′) shows microvascular proliferation in this GBM. (B) High-magnification views of (A) illustrate that both malignant cells and nuclei are highly pleomorphic. Many GBM cells have substantial cytoplasm and some have eccentric nuclei (a, a′). (C) The p53ΔE5-6 gliomas exhibit the secondary structures of Scherer: accumulation of GFAP-positive tumor cells in the subpial zone of the cerebral cortex (a, a′); perivascular satellitosis (arrowheads) (b, b′); and perineuronal satellitosis (arrowheads, c, c′). (d, d′) The examples of Olig2+ tumor cells with abnormal mitoses (arrowheads). BV, blood vessels. Scale bar, (A, B, Cad), 50 μm; (Ca′-d′), 25 μm.