Abstract
A marked shift in tobacco-related workplace health promotion intervention involves the adoption of policies barring employment to smokers. We discuss the potential public health consequences of these policies on those affected – smokers, their families, the surrounding community, and society at large. We find a lack of published evidence evaluating the effectiveness and consequences of these policies. By developing a model of policy effects, we outline possible unintended consequences. With such large gaps in the evidence base and the potential for deleterious consequences, we argue for increased discussion about the use of smoker-free employment policies as a public health intervention and for increased engagement of employers by the public health community in worksite health promotion.
Keywords: tobacco cessation, tobacco prevention and control, worksite, promotion, health, organizational policy
The movement to promote smoke-free workplaces for all employees began in 1971, when Surgeon General Jesse Steinfeld called for a ban on smoking in public places, declaring that “Nonsmokers have as much right to clean air and wholesome air as smokers have to their so-called right to smoke, which I would define as a ‘right to pollute.’ It is high time to ban smoking from all confined public places such as restaurants, theaters, airplanes, trains and buses.”1 In 1975, Minnesota became the first state to enact a comprehensive smoke-free air law, which included restrictions on smoking in private workplaces.2 Since then, smoke-free workplace policies have spread widely, throughout the United States and the rest of the world.2 As of August 2008, 21 states and more than 400 U.S. cities had laws requiring 100% smoke-free workplaces.3 In addition, nine Canadian provinces, six Australian states and territories, and 14 other countries have banned smoking in workplaces, including bars and restaurants.4
The proliferation of clean indoor air laws has been described as occurring in four waves: (1) protection of the public from secondhand smoke in public places, such as elevators, movie theatres, retail stores, and public buildings; (2) smoke-free workplaces, focusing on office buildings while exempting service workplaces, such as restaurants and bars; (3) smoke-free restaurants; and (4) smoke-free bars and casinos.5
In recent years, a new trend in worksite smoking policies has emerged: a shift from “smoke-free” workplace policies to what have been termed “smoker-free” workplace policies.6,7 These policies, instituted by employers but often promoted by public health or tobacco control organizations, refuse employment to smokers; some even fire existing smoking employees if they do not quit in a prescribed time period.8,9
Examples of companies barring employment to smokers include Crown Laboratories10 in Tennessee and Truman Medical Centers11 in Kansas City. The Cleveland Clinic, Ohio’s second largest employer, also bars employment to smokers.12 Other examples include the Cleveland-based employer, Medical Mutual13 and Scotts Miracle Gro Company in Marysville, Ohio.14 Daytona-based The Homac Companies makes their policy plain on their hiring page, stating “Tobacco Free Candidates Only.”15 Weyco Inc., an employee benefits firm in Ohio, is an extreme example. In 2003, Weyco stopped hiring smokers. The company also made smoking off premises and outside work hours a firable offense.16 More recently Weyco went a step further and expanded the policy to spouses of employees.
Smoker-free hiring policies are not unique to the United States. In 2005, the World Health Organization (WHO) began barring employment to smokers.17,18
While smoker-free employment policies are adopted by employers, the tobacco control movement has played some role in promoting these policies. For example, the National Cancer Institute’s (NCI) ASSIST manual (Strategies to Control Tobacco Use In the United States: A Blueprint for Public Health Action in the 1990’s) specifically suggests preferential hiring of nonsmokers as a viable policy option to decrease cigarette consumption: “Economic incentives serve to reduce consumption of tobacco products by increasing, either directly or indirectly, the costs of using these products. In this section, three economic incentive policies are examined: (1) higher excise taxes on cigarettes, (2) preferential hiring and promotion of nonsmokers, and (3) insurance premium differentials for smokers and nonsmokers.”19
There are a number of reasons given for implementing smoker-free workplace policies. Some employers cite value-based reasons: aligning the workforce with organizational philosophy.11,18 Others state that they need to control rising health care costs.10,14 Malouff et al. expound a number of additional reasons an employer may want to adopt these policies.20 The National Cancer Institute adds that these policies may reduce cigarette consumption, both by promoting cessation among current smokers and by reducing the social acceptability of smoking.19
Opponents to the adoption of smoker-free workplace policies have focused mainly on issues of discrimination or privacy infringement.7,21 These arguments have been used, with support from the American Civil Liberties Union and the tobacco industry, to promote state laws that protect smokers from employment discrimination.20 Approximately 25 states have adopted such laws. However, the remaining states have at-will employment, meaning that refusal to hire smokers is legal in these states.20 International laws vary but the WHO’s adoption of a smoker-free employment policy indicate that this issue is a very real one internationally.
The promotion of smoker-free workplace policies has sparked a debate in the tobacco control community, captured in a 2005 point-counterpoint debate in Tobacco Control. 6,7 Gray supported such policies, arguing that they not only save employers money by reducing health care costs, but also encourage smokers to quit and set an exemplary policy that supports a smoke-free norm in society.6 Chapman countered, arguing that such policies represent a form of employment discrimination that is not justified.7
Despite the emergence of this issue into international tobacco control discussion sparked by the publication of these commentaries, we are not aware of much further published consideration of the issue. Moreover, we are not aware of any published attempts to define and outline the potential consequences of smoker-free hiring policies in an effort to analyze their likely effects and allow a more informed debate about the issue.
In this article, we hope to advance that debate by developing and presenting a model to consider the consequences – both positive and negative – of smoker-free workplace policies. Our goal is to call attention to, and engage public health professionals in a discourse on the possible effects and consequences of these new policies. Our goal is not necessarily to present an argument in favor of or against smoke-free workplace policies; instead, we hope to introduce a model that may be useful in informing debate and ensuring that all potential consequences of these policies are adequately considered.
Our interest in creating a model to consider the effects of smoker-free workplace policies is not just a theoretical one. There is empirical evidence that smoker-free as opposed to smoke-free workplace policies have a profoundly different impact on the public; in particular, on smokers.
Stuber et al. recently published an analysis of the determinants of smoker-related stigma among current and former smokers.22 They defined stigma as “the negative labels, pejorative assessments, social distancing and discrimination that can occur when individuals who lack power deviate from group norms.”22,p.421 Stigma was measured using a validated, 12-item scale that specifically considered the role of social policy and the perceived social acceptability of smoking. The authors found that smoke-free air laws actually lowered self-reported smoker-related stigma. In contrast, smoker-free workplace and similar discriminatory policies toward smokers significantly increased smoker-related stigma. The authors conclude that while smoke-free air laws alter social norms “without contributing to the stigmatization of individual smokers,”22,p.428 the same is not true for smoker-free workplace policies. They also conclude that the tobacco control community needs to explicitly address “the role of stigmatization in the epidemic and decide if it is something it wants to promote or discourage.”22,p.429
This is the first empirical evidence, to the best of our knowledge, demonstrating that the shift from smoke-free to smoker-free workplace policies might have an adverse effect on smokers by creating a negative self-image. Whether this stigma leads to smoking cessation – a positive outcome – or decreased self-esteem, which could make smokers more resistant to quitting and more likely to engage in other unhealthy behaviors,23 is not clear. What is clear, however, is that the potential consequences of this stigmatization must be considered.
In developing our model, we first outline the existing evidence base. Second, we assess the potential public health consequences using a broad-based perspective. Finally, we consider public health, legal, and ethical principles and their implications in evaluating smoker-free workplaces as a public health intervention strategy.
Evidence-base for smoker-free workplace policies
There are currently no published evaluations of workplace policies barring employment to smokers. However, there is substantial evidence that policies which ban smoking in the workplace reduce cigarette consumption, increase attempts to quit, as well as decrease overall tobacco use prevalence.24–31 Smoke-free workplaces have also been shown to lower exposure to environmental tobacco.32–34 The effects of workplace tobacco use policies on reducing increased health insurance costs incurred by smokers is unclear,25 as is the literature on more pervasive restrictions such as in the domestic environment.26
Model of policy effects
While it is currently unknown what effect smoker-free workplace policies would have on smokers, in Figure 1 we explore possible consequences using a causal loop diagram.35,36 In the figure directional arrows indicate causality. Positive signs note an increasing relationship, while negative signs signal a decreasing relationship. Thus, in a positive relationship if X increases then so does Y. In a negative relationship if X increases then Y decreases. Thick arrows represent stated goals of these workplace policies, thin arrows are potential ‘unintended consequences.’
Figure 1. Model of public health consequences of workplace policies barring employment to smokers.
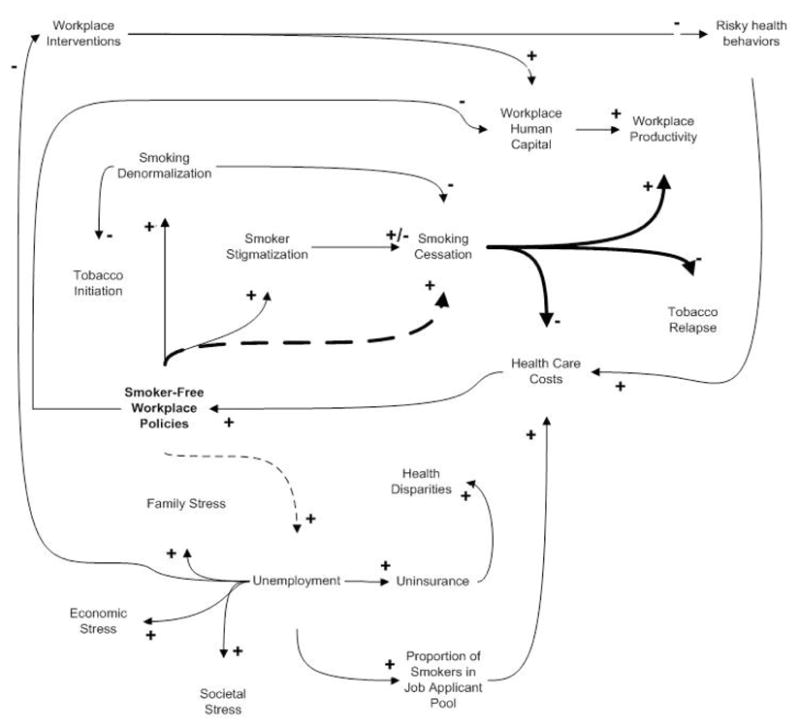
* Directional arrows indicate causality, signs indicate direction: positive indicates an increasing relationship, negative a decreasing relationship. Thus, an increase in X corresponds with an increase in Y. Thick arrows represent stated goals, thin arrows unintended consequences.’ Dotted lines indicate critical leverage points in the model.
In building our model we recognize that employers and their employees operate within dynamic economic, social, political, and other relationships. Our model is not meant to be exhaustive, but rather illustrative based on the related public health evidence base. The ultimate goal is to begin to recognize potential immediate, delayed and distal impacts of workplace policies barring employment to smokers within all levels of the socio-ecological framework.
Implementation of a workplace policy barring employment to smokers leads to two potential outcomes for employed smokers. First, some will quit smoking and maintain their current employment. Besides the obvious health benefits of tobacco cessation, these employees will also receive continued health insurance coverage (if provided by their employer). Moreover, it is likely that their potential to relapse would be reduced due to the consequences of resuming smoking. Further, they will continue to benefit from being exposed to other workplace health promotion programs that are offered.
For non-smoking employees at the worksite, tobacco cessation by fellow employees would lower exposure to environmental tobacco smoke if the worksite did not already have a smoke-free workplace policy in place.32–34 For employers, when smoking employees quit tobacco there may be several effects. The productivity of former smokers may increase,37 though the evidence is limited regarding the productivity effects of workplace smoking bans.26 In addition, these policies will likely reduce health insurance costs for employers since smokers incur increased costs.25,38 Conversely, employers may also experience a decrease in human capital, both from losing current employees who choose or are unable to quit, as well as future employees that smoke. For instance, in St. Cloud, FL a ban on smoking employees was rescinded by the city council after employers found it difficult to find qualified employees.39
As just noted, the second outcome for smokers working with employers who initiate a policy banning smoking is that they will either be terminated or resign. Some of these smokers may try to quit and be unsuccessful. Nicotine is addictive, recognized as being on par with cocaine or heroin.40 Theories of health behavior change such as the Stages of Change suggest that behavior change is not an all or nothing choice but rather a process.41 Only about 2.5% of current smokers successfully stop smoking permanently each year.42 Employers can help support smokers attempting to quit, however, by providing tobacco cessation aid. For example, an employer could offer nicotine replacement therapy to their current smoking employees to help improve the chances of quitting.43
For those smokers who are unable to or refuse to cease tobacco use, some will re-enter the job market and find new employment. The consequences of even brief unemployment are more fully discussed below. Those smokers that do find new employment alter the remaining risk pool for other employers,44 leading to rising health care costs for those workplaces. In other words, the employment market will represent an increased proportion of smokers who are more costly to insure than non-smokers. There is the potential that in response to the corresponding rise in health care costs, other employers may also begin initiating policies barring employment to smokers.
Smokers who are terminated or resign and are unable to find new employment represent the population at greatest risk for adverse health outcomes. If a smoker is unable to find new employment, however, this may also incentivize them to either attempt or re-attempt quitting smoking. Part of the likelihood of smokers being unemployed for longer time periods is the availability of employers who will still hire smokers. If these policies continue to proliferate, this can become a very real possibility. It is easier to imagine this scenario having a real effect in rural areas where there may be only one or a few major employers.
Unemployment can lead to personal, family, and economic stressors that adversely impact health outcomes.45 Since health insurance is often covered by employers – employer-sponsored insurance insures approximately 64.4% of adults in the US46 – many of these individuals will become uninsured. In a series of landmark reports, the Institute of Medicine illustrated the potential consequences of lack of insurance on multiple domains of society. The uninsured have a more difficult time finding and utilizing health care services, and the care provided is often non-reimbursed.45,47 Reduced access to care in turn leads to adverse economic, social, and health consequences for these smokers and their families. Further, a growing uninsured population can create financial stresses that affect the ability of health care providers to provide services to the community. Finally, the uninsured represent lost opportunities of those individuals to more fully participate in society.
In broader social terms, smokers may feel stigmatized as well. Modified labeling theory posits that when social forces about behavior are communicated individuals may experience social devaluation and discrimination.48 These feelings may increase social isolation, rejection, and perceived lack of personal control. Work by Marmot and others has shown that people with the least feeling of control over their lives have the poorest health outcomes.49 While this would not apply to all smokers, some may experience these situations. A recent study on smoker stigma also shows that stigma effects may differentially impact smokers – those with greater education and whites perceived greater stigma than those with lower education and racial minorities.22
Effects of labeling on individuals with mental illness and infectious and chronic diseases has been shown to impact health outcomes.50,51 Further, people with the highest rates of smoking are those with mental illness or substance abuse problems.52 Since they are already stigmatized by their underlying psychiatric condition, smoking stigmatization may further burden these individuals and their families.53
Related to stigmatization, these policies may also have a broader social effect in continuing the denormalizaiton of tobacco use. Public health policies such as local ordinances against smoking at public parks and other measures represent a societal shift in how smoking is viewed. Numerous studies point to the power of these policies to reduce tobacco use.54 Smoker-free workplace policies may demonstrate similar benefits in reducing smoking initiation and relapse, and increasing cessation attempts.
Using data from the Framingham Heart Study, Christakis and Fowler have recently shown that smokers have become increasingly marginalized socially and clustered together.55 Smoker-free workplace policies would likely have an additive effect in moving those who refused or were unable to quit to the social periphery, both through displacement from employment as well as smoker stigmatization. This marginalization may produce positive or negative outcomes. For instance, perhaps this would encourage remaining smokers to quit, including increasing social pressure from friends and family who have been shown to influence smoking behavior. On the other hand, increasing social marginalization may make it harder to stop smoking – smokers may remain in social pockets where smoking is still normalized.53
Unemployment and potential lack of access to health insurance among some smokers may also increase health disparities. Disparities already exist among those who smoke, their risk factors, insurance coverage, access to health care, health outcomes, disease burden, and educational and social status.56 Further, those races which over-represent smokers, such as Native Americans and African Americans,57 also suffer greater health burdens themselves.58 Smokers are among the most disadvantaged groups in the US, including the poor, lower educated,57 and racial minorities.59 Increasing the proportion of smokers who are unemployed will affect their socio-economic status and health outcomes.60 Moreover, those smokers who also lose insurance will receive less care and have worse health outcomes.61
Critical leverage points in model and need for future research
There are two critical leverage points in the model, indicated in Figure 1 with dotted lines. On the upside (positive effects), the key arrow is that leading from smoker-free workplace policies to smoking cessation. On the downside (negative effects), the key arrow is that leading from smoker-free workplace policies to unemployment. Thus, there are two critical questions that need to be answered: (1) Will smoker-free policies encourage smokers to quit smoking or will these policies simply shift smokers to other worksites or to unemployment? (2) If smokers do not quit in order to obtain jobs at smoker-free workplaces, will they simply shift to other workplaces or will there be an increase in unemployment?
Neither of these research questions has been studied. Our model suggests that these are the two key areas of research that need to be conducted in order to be able to evaluate the potential public health effects of smoker-free workplace policies in an informed way.
Smoker-free policies in a legal, ethical, and public health context
Our model highlights potential positive and negative outcomes of smoker-free workplace policies, as well as important points that could be leveraged both to increase tobacco cessation and mitigate associated harms. In considering the model, it is important to frame these policies within a legal, ethical, and public health context. Our goal is not to make an argument about “morality” but rather situate these policies within the normative structure of social, medical, and public health norms, values, and ideals.
Legal context
The legality of barring employment to those engaging in a legal behavior on their own time is debateable. Courts have consistently ruled against a fundamental right to smoke in the sphere of privacy.62 However, some view these policies as discriminatory.7,9,16,21 While certain groups (e.g., women, racial/ethnic minorities, etc.) are intrinsically protected by federal law,63 some states have actively put in place employment antidiscrimination laws protecting voluntary, off duty behavior. For smokers, 26 states have enacted legislation prohibiting policies barring employment due to off-duty tobacco use.63 These statutes vary considerably; some prohibit discrimination based on use of any lawful products during nonworking hours and off employer property. In other states, especially those with at-will employment policies, there may be little recourse for smokers who suffer employment discrimination. A lawsuit currently being heard in Massachusetts may have substantial bearing on the legality of smoker-free hiring policies.64 In this case, a man who was fired for smoking off the job is suing the Scotts Company. A state judge has allowed the suit to go forward on the grounds of invasion of privacy.
Ethical context
These workplace policies must also be considered in light of ethical principles that underlie public health conduct.65,66 Below we briefly outline potential arguments both for and against these policies.
Beneficence
We violate the obligation to help people in poor health by excluding smokers who become unemployed from accessing employer-based health insurance. Conversely, we support the wellness of non-smokers by reducing their exposure to second-hand smoke from fellow smoking employees.
Nonmaleficence
No evidence exists to evaluate the policies. However, we may be doing both individual and societal harm by placing smokers into poor circumstances for their health. On the other hand, these policies may support denormalization of tobacco use, resulting in decreased smoking initation and increased smoking cessation.
Autonomy
These policies violate the right of smokers to choose and follow their own actions. If smokers are engaging in high-risk but legal behaviors, is it appropriate to restrict their autonomy? However, we have noted that nicotine addiction is not a choice, and instituting these policies may help confront this addiction.
Justice
These policies treat smokers as different from people who engage in other high-risk behaviors, such as poor nutrition, lack of physical activity, and alcohol and other drug abuse. However, these policies also assure that justice is provided to nonsmokers and that their health is protected.
Public health context
Finally, we discuss the appropriateness of these policies in a public health context. Successful methods for smoking cessation address the determinants of smoking, including psychological, social, economic, and biological factors.67 Moreover, evidence suggests that workplace health promotion programs targeting tobacco cessation are effective.26 A review of the major public health “calls to action” illustrates the field’s focus on providing more comprehensive policies68 that target the “fundamental causes of disease”69 and work to reduce tobacco-related disparities.56,70 These policies, if they do place smokers, their families, and communities at increased risk (Figure 1) may be excluding smokers from continued support.71 Conversely, from the viewpoint of weak paternalism these policies may be justifiable, both in terms of preventing smokers from continuing to harm themselves and protecting the health of non-smokers.71
Public health norms on workplace health promotion have encouraged comprehensive rather than restrictive approaches to chronic disease management.72 These workplace policies barring employment to smokers represent a marked shift in workplace health promotion strategies. As an example, consider the public health response to workplace health promotion in reducing obesity. A recent study by Duke University researchers found that obese workers had greater lost workdays and medical claims.73 The authors noted “It is increasingly common for employers to support healthy lifestyle interventions such as healthy cafeteria food, on-site fitness facilities, and encouragement of physical activity during work breaks. Our study lends support to the notion that such programs may not only improve the health of employees but also be financially beneficial.” Further, when the media covered the study, “New York employment attorney Richard Corenthal cautioned employers not to overreact with discriminatory policies. ‘Employers need to be careful not to view this study as a green light to treat obese or overweight workers differently,’ Corenthal said.”74
Shifting public health norms in how we respond to smokers versus other groups can have real consequences. For instance, in 2006 a primary care trust announced that it would remove smokers from surgery wait lists, citing an effort to contain costs.75 Moreover, by not responding to the changing norm in treating smoking as a different high-risk behavior than others, norms of other unhealthy behavior could also start to shift and socially justify barring employment to other groups. As an example, Indianapolis-based Clarian Health, a hospital system, will begin fining employees for smoking, having a BMI greater than 30, and if their blood pressure, cholesterol, and glucose levels are too high.76
Concluding thoughts
We have developed a model of the potential positive and negative effects on public health of workplace policies barring employment to smokers. If “all models are wrong”77 ours is certainly no exception. However, our goal has been to argue that greater engagement by the public health community in evaluating and assessing the appropriateness of these policies in workplace tobacco control is necessary. The potential unintended side effects of such policies could be far-reaching, especially since many of the model’s dynamics are non-linear and time-delayed.36 Putting these policies into legal, medical, and public health practice contexts further supports the need to weigh the evidence for and against these policies to ensure that we are addressing the fundamental determinants of tobacco use and reducing related health disparities. This essay is hopefully the first step towards an active, informed, and engaged debate on the public health appropriateness of barring employment to smokers as part of tobacco control policy.
Footnotes
Competing interest declaration: We have no competing interests to disclose.
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article to be published in Tobacco Control editions and any other BMJPGL products to exploit all subsidary rights, as set out in our licence http://tc.bmjjournals.com/ifora/licence.dtl”
References
- 1.Steinfeld JL. Women and children last? Attitudes toward cigarette smoking and nonsmokers’ rights, 1971. NY State J Med. 1983;83:1257–1258. [PubMed] [Google Scholar]
- 2.Eriksen M, Chaloupka F. The economic impact of clean indoor air laws. CA Cancer J Clin. 2007;57:367–378. doi: 10.3322/CA.57.6.367. [DOI] [PubMed] [Google Scholar]
- 3.American Nonsmokers’ Rights Foundation. States, commonwealths, and municipalities with 100% smokefree laws in workplaces, restaurants, or bars. Berkeley, CA: American Nonsmokers’ Rights Foundation; 2008. [Accessed August 11, 2008]. http://www.no-smoke.org/pdf/100ordlist.pdf. [Google Scholar]
- 4.American Nonsmokers’ Rights Foundation. Smokefree status of hospitality venues around the world. Berkeley, CA: American Nonsmokers’ Rights Foundation; 2008. [Accessed August 11, 2008]. http://www.no-smoke.org/pdf/internationalbarsandrestaurants.pdf. [Google Scholar]
- 5.Siegel M, Skeer M. Exposure to secondhand smoke and excess lung cancer mortality risk among workers in the “5 B’s”: bars, bowling alleys, billiard halls, betting establishments, and bingo parlours. Tob Control. 2003;12:333–338. doi: 10.1136/tc.12.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gray NJ. The case for smoker-free workplaces. Tob Control. 2005;14:143–144. doi: 10.1136/tc.2004.010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman S. The smoker-free workplace: the case against. Tob Control. 2005;14:144. doi: 10.1136/tc.2004.010348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snow M. [Accessed August 11, 2008];No smoking. http://www.cnn.com/2005/US/01/26/no.smoking/index.html.
- 9.American Civil Liberties Union. [Accessed January 7, 2008];Lifestyle discrimination in the workplace: your right to privacy under attack. http://www.aclu.org/workplacerights/gen/13384res19981231.html.
- 10.Hicks T. Where there’s smoke, there’s not a new hire: local company unveils tough new smoking policy. Johnson City Press. 2005 December 18; [Google Scholar]
- 11.Gish J. Some employers refusing to hire smokers. [Accessed January 7, 2008];KMBC-TV. 2007 November 22; http://www.kmbc.com/news/14671023/detail.html.
- 12.Vanac M. Clinic will not hire any smokers. The Plain Dealer. 2007 June 28; [Google Scholar]
- 13.Medical Mutual. [Accessed January 7, 2008];Hiring of non-tobacco users. http://www.medmutual.com/gls.aspxobal/careers/nonewsmoker.
- 14.Curet M, Stammen K. Your smokes or your job. The Columbus Dispatch. 2005 December 9; [Google Scholar]
- 15.The Homac Companies. [Accessed January 7, 2008];Careers. http://www.homac.com/careers/careers.htm.
- 16.Joyce A. So much for ‘personal’ habits. Washington Post. 2006 October 15; [Google Scholar]
- 17.Dyer O. WHO will not hire smokers. BMJ. 2005;331:1360. [Google Scholar]
- 18.World Health Organization. WHO policy on non-recruitment of smokers or other tobacco users: Frequently asked questions. Geneva: World Health Organization; [Accessed January 7, 2008]. http://www.who.int/employment/FAQs_smoking_English.pdf. [Google Scholar]
- 19.National Cancer Institute. Strategies to control tobacco use in the United States: a blueprint for public health action in the 1990’s (Smoking and Tobacco Control Monograph #1) Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 1991. NIH Publication No. 92–3316. [Google Scholar]
- 20.Malouff J, Slade J, Nielsen C, Schutte N, Lawson E. US laws that protect tobacco users from employment discrimination. Tob Control. 1993;2:132–138. [Google Scholar]
- 21.Glantz L. Smoke got in their eyes. Washington Post. 2005 December 18; [Google Scholar]
- 22.Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Soc Sci Med. 2008;67:420–430. doi: 10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burris S. Stigma, ethics and policy: A commentary on Bayer’s “stigma and the ethics of public health: not can we but should we”. Soc Sci Med. 2008;67:473–475. doi: 10.1016/j.socscimed.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Moskowitz JM, Lin Z, Hudes ES. The impact of workplace smoking ordinances in California on smoking cessation. AJPH. 2000;90(5):757–61. doi: 10.2105/ajph.90.5.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande-Kulis VG, Fielding JE, Alao MO, McKenna JW, Sharp DJ, Harris JR, Woollery TA, Harris KW The Task Force on Community Preventive Services. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. AJPM. 2001;20(S2):16–66. doi: 10.1016/s0749-3797(00)00297-x. [DOI] [PubMed] [Google Scholar]
- 26.Brownson RC, Hopkins DP, Wakefield MA. Effects of smoking restrictions in the workplace. Annu Rev Public Health. 2002;23:333–348. doi: 10.1146/annurev.publhealth.23.100901.140551. [DOI] [PubMed] [Google Scholar]
- 27.Woodruff TJ, Rosbrook, Pierce J, et al. Lower levels of cigarette consumption found in smoke-free workplaces in California. Arch Intern Med. 1993;153:1485–93. [PubMed] [Google Scholar]
- 28.Farrelly MC, Evans WN, Sfekas AE. The impact of workplace smoking bans: Results from a national survey. Tobacco Control. 1999;8:272–7. doi: 10.1136/tc.8.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eriksen MP, Gottlieb NH. A review of the health impact of smoking control at the workplace. Am J Hlth Promot. 1998;13:83–104. doi: 10.4278/0890-1171-13.2.83. [DOI] [PubMed] [Google Scholar]
- 30.Wakefield MA, Wilson D, Owen N, et al. Workplace smoking restrictions, occupational status, and reduced cigarette consumption. JOM. 1992;34:693–7. [PubMed] [Google Scholar]
- 31.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325:188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borland R, Pierce JP, Burns DM, Gilpin E, Johnson M, Bal D. Protection from environmental tobacco smoke in California: the case for a smoke-free workplace. JAMA. 1992;268(6):749–52. [PubMed] [Google Scholar]
- 33.Moskowitz JM, Lin Z, Hudes ES. The impact of California’s smoking ordinances on worksite smoking policy and exposure to environmental tobacco smoke. Am J Health Promot. 1999;13(5):278–81. doi: 10.4278/0890-1171-13.5.278. [DOI] [PubMed] [Google Scholar]
- 34.Marcus BH, Emmons KM, Abrams DB, et al. Restrictive workplace smoking policies: Impact on nonsmokers’ tobacco exposure. J Pub Hlth Pol. 1992;13:42–51. [PubMed] [Google Scholar]
- 35.National Cancer Institute. Tobacco Control Monograph No. 18. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; Apr, 2007. Greater Than the Sum: Systems Thinking in Tobacco Control. NIH Pub. No. 06-6085. [Google Scholar]
- 36.Sterman JD. Learning from evidence in a complex world. AJPH. 2006;96(3):505–514. doi: 10.2105/AJPH.2005.066043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bertera R. Effects of behavioral risks on absenteeism and health care costs in the workplace. Journal of Occupational Medicine. 1991;33(11):1119–1124. doi: 10.1097/00043764-199111000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Sofian N, Mcafee T, Doctor J, Carson D. Tobacco control and cessation. In: O’Donnell M, Harris JS, editors. Health Promotion in the Workplace. 2. Albany, NY: Delmar; 1994. p. 346. [Google Scholar]
- 39.Florea L. St. Cloud hires smokers again. Orlando Sentinel. 2006 May 24; [Google Scholar]
- 40.U.S. Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress. A Report of the Surgeon General. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. DHHS Publication No. (CDC) 89–8411. [Google Scholar]
- 41.National Cancer Institute. Theory at a Glance: A Guide for Health Promotion Practice. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2005. NIH Pub. No. 05-3896. [Google Scholar]
- 42.Centers for Disease Control and Prevention. Smoking cessation during previous year among adults—United States, 1990 and 1991. MMWR. 1993;42:504–507. [PubMed] [Google Scholar]
- 43.Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic Reviews. 2008;(1) doi: 10.1002/1465.CD000146.pub.3. Art. No.: CD000146. [DOI] [PubMed] [Google Scholar]
- 44.Blumenthal D. Employer-sponsored insurance – Riding the health care tiger. NEJM. 2006;355(2):195–202. doi: 10.1056/NEJMhpr060704. [DOI] [PubMed] [Google Scholar]
- 45.Institute of Medicine. Hidden Costs, Value Lost: Uninsurance in America. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 46.Holahan J, Cook A. The U.S. economy and changes in health insurance coverage, 2000–2006. Health Affairs. 2008;27:w135–144. doi: 10.1377/hlthaff.27.2.w135. [DOI] [PubMed] [Google Scholar]
- 47.Institute of Medicine. A Shared Destiny: Community Effects of Uninsurance. Washington, DC: National Academy Press; 2003. [Google Scholar]
- 48.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: An empirical assessment. ASR. 1989;54(3):400–423. [Google Scholar]
- 49.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 50.Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock LY. On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior. 1997;38:177–190. [PubMed] [Google Scholar]
- 51.Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior. 2000;41:50–67. [PubMed] [Google Scholar]
- 52.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 53.Schroeder S. Stranded in the periphery – The increasing marginalization of smokers. NEJM. 2008;358:2284–2286. doi: 10.1056/NEJMe0802708. [DOI] [PubMed] [Google Scholar]
- 54.Centers for Disease Control and Prevention. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000. [Google Scholar]
- 55.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. NEJM. 2008;358:2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Centers for Disease Control and Prevention. Advancing the Nation’s Health: A Guide to Public Health Research Needs, 2006–2015. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2006. [Google Scholar]
- 57.Giovino GA. Epidemiology of tobacco use in the United States. Oncogene. 2002;21(48):7326–7340. doi: 10.1038/sj.onc.1205808. [DOI] [PubMed] [Google Scholar]
- 58.National Center for Health Statistics. Health, United States, 2000. Hyattsville, MD: 2000. [Google Scholar]
- 59.CDC. Tobacco use among adults --- United States, 2005. MMWR. 2006;55:1145–1148. [PubMed] [Google Scholar]
- 60.Evans RG, Barer M, Marmor TR, editors. Why Are Some People Healthy and Others Not?: The Determinants of Health of Populations. New York: Walter de Gruyter, Inc; 1994. [Google Scholar]
- 61.American College of Physicians. No Health Insurance? It’s Enough to Make You Sick. 2000 http://www.acponline.org/uninsured/lack-contents.htmRetrieved September 23, 2008.
- 62.City of North Miami v. Kurtz. 653 So.2d 1025, 1028, (FL 1995)
- 63.Coil JH, III, Rice CM. When off-duty conduct becomes off limits: State laws expand to protect employees outside the workplace. Employment Relations Today. 2004;31:75–84. [Google Scholar]
- 64.Scott Rodrigues v. The Scotts Company, LLC. Civil action no. 07-1004-GAO, (MA 2008)
- 65.Fox BJ. Framing tobacco control efforts within an ethical context. Tob Control. 2005;14:38–44. doi: 10.1136/tc.2004.008300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Beauchamp T, Childress JF. Principles of Biomedical Ethics. Oxford Univ Press; 2001. [Google Scholar]
- 67.Fisher E, Lichtenstein E, Haire-Joshu D, Morgan GD, Rehberg HR. Methods, successes, and failures of smoking cessation programs. Annual Review of Medicine. 1993;44:481–513. doi: 10.1146/annurev.me.44.020193.002405. [DOI] [PubMed] [Google Scholar]
- 68.U.S. Department of Health and Human Services. With Understanding and Improving Health and Objectives for Improving Health. 2. Vol. 2. Washington, DC: U.S. Government Printing Office; Nov, 2000. Healthy People 2010. [Google Scholar]
- 69.Public Health Leadership Society. Principles of Ethical Practice of Public Health. 2002 http://www.apha.org/NR/rdonlyres/1CED3CEA-287E-4185-9CBD-BD405FC60856/0/ethicsbrochure.pdf. Retrieved April 11, 2008.
- 70.U.S. Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevetion and Health Promotion, Office on Smoking and Health; 2000. [Google Scholar]
- 71.Buchanan DR. Autonomy, paternalism, and justice: Ethical priorities in public health. AJPH. 2008;98:15–21. doi: 10.2105/AJPH.2007.110361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gottlieb NH. Tobacco control and cessation. In: O’Donnell M, editor. Health Promotion in the Workplace. 3. Albany, NY: Delmar Publishing; 2001. pp. 338–362. [Google Scholar]
- 73.Ostbye T, Dement JM, Krause KM. Obesity and workers’ compensation: Results from the Duke Health and Safety Surveillance System. Arch Intern Med. 2007;167:766–773. doi: 10.1001/archinte.167.8.766. [DOI] [PubMed] [Google Scholar]
- 74.Johnson CK. Study: Fat workers cost employers more. Boston Globe. 2007 April 23; [Google Scholar]
- 75.Glantz L. Should smokers be refused surgery? BMJ. 2007;334:21. doi: 10.1136/bmj.39059.532095.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McGregor J. Being unhealthy could cost you - Money. Business Week. 2007 August 2; [Google Scholar]
- 77.Sterman JD. All models are wrong: Reflections on becoming a systems scientist. System Dynamics Review. 2002;18:501–531. [Google Scholar]


