Abstract
Ten cases of aneurysmal bone cysts are presented. Patients ranged in age from five years to 64 years. Treatment was resection or curettage; four patients had preoperative embolization. Treatment results were excellent. Six patients had no recurrence while recurrences in the other four patients were successfully treated by recurretage, two with adjunctive CyberKnife therapy. All ten patients are currently disease free for at least two years. Only two patients have residual neurologic deficit in the form of bowel or bladder dysfunction.
INTRODUCTION
Aneurysmal bone cysts are destructive, expansile bone lesions characterized by a reactive proliferation of connective tissue containing multiple blood filled cavities. Presumably due to the local hemodynamic disturbances, the process arises de novo in bone or is engrafted on preexisting bone lesions histologically identifiable in 30 percent of cases.1 Conventional therapy is curettage and bone grafting, although lesions may recur in anywhere from 12 to 59% of cases.2,3,4
Aneurysmal bone cysts most commonly occur in the distal femur or proximal tibia. The pelvis and posterior elements of the spine are also commonly involved. Rarely, aneurysmal bone cysts occur in the sacrum. In this location, therapy is limited by lesion's close association with sacral nerve roots and the possibility of resultant neurologic deficit. We are reporting ten cases of aneurysmal bone cyst of the sacrum, and we will describe the clinicopathologic features, therapy, and follow-up of these lesions.
MATERIALS AND METHODS
The ten cases were from the personal files of one of us (EFM).
In all cases, images and histologic slides were available for review. All patients had detailed clinical history with long term follow-up (Table 1).
TABLE 1.
| Patient | Age/Gender | Treatment | Recurrence | Disease free follow-up | Neurologic Deficit |
|---|---|---|---|---|---|
| 1 | 64F | Resection | None | 4 years | None |
| 2 | 26F | Curettage | 1.5 years – | 2 years | None |
| 3 | 39M | Resection | 6 years Curettage 6 months –Embolization & Curettage ? Giant Cell Tumor | 2 years | Bowel & Bladder Dysfunction |
| 4 | 16 F | Embolization & Curettage | None | 12 years | None |
| 5 | 32 M | Curettage | 2 Years –Embolization, Radiation, Resection | 5 years | None |
| 6 | 60 F | Mid-Sacral Amputation | None | 2 years | None |
| 7 | 57 M | Embolization & Mid-Sacral Amputation | 3.5 years –Curettage? Osteoblastoma | 2 years | Bowel Bladder Dysfunction |
| 8 | 10 F | Embolization & Curettage | None | 2 years | None |
| 9 | 5F | Curettage | None | 2 years | None |
| 10 | 17 F | Mid-Sacral Amputation | None | 2 years | None |
PATIENTS
Patient 1
A 64 year-old woman had low-back pain for eight to ten years. Recently, there had been a history of a right sciatic sciatica, and there had been difficulty walking due to weakness of the right foot. She also had a loss of sensation and some tingling in the right foot. She had no history of bowel or bladder dysfunction. An MRI demonstrated a destructive lesion in the S1 vertebral body with extension into the sacral ala. The lesion contained multiple fluid-fluid levels. She underwent a partial resection of the left side of the sacrum with a curettage. She also underwent a posterior lumbar fusion with fixation. She had a year of post-operative pain. Four years after surgery, the patient is without recurrence or neurological deficit.
Patient 2
A 26 year-old woman had a three month history of low back pain. An MRI showed a lesion in her sacrum with multiple fluid-fluid levels consistent with an aneurysmal bone cyst. She had no evidence of weakness, but there was some intermittent posterior leg numbness. She had no difficulty with bladder or bowel function. After preoperative embolization she underwent a thorough intralesional curettage. One and a half years post curettage she developed a recurrence in the sacrum and adjacent soft tissue. She had a resection of the soft-tissue portion of this mass followed by a curettage of the sacrum underneath. Six years after surgery she had a second recurrence in the S1 sacral ala. She had a third curettage of this lesion followed by packing with bone graft. Three years after this third surgery she is without recurrent disease or neurologic deficit.
Patient 3
A 39 year-old male had a one year history of constipation and bladder dysfunction. His MRI showed a mutliloculated sacral tumor at the S2-3 level. The patient underwent a laminectomy at S2, S3 with corpectomy of these segments. The diagnosis was aneurysmal bone cyst with a suggestion of an underlying giant cell tumor. The patient developed a significant recurrence of this lesion six months after surgery. Patient underwent embolization, radiotherapy, and another excision of the mass. The patient continues to have bowel and bladder dysfunction, but there is no evidence of recurrence two years after the last surgery.
Patient 4
A 16 year-old woman had a three month history of low-back pain. There were no neurological symptoms and no bowel or bladder dysfunction. MRI's demonstrated a destructive lesion of the sacrum consistent with an aneurysmal bone cyst. An open biopsy confirmed this. After preoperative embolization the patient underwent a thorough curettage of this lesion. There was resolution of the symptoms following surgery and no evidence of recurrence after 12 years.
Patient 5
A 32 year-old man had low-back pain and radiation to his right leg. He was found to have a destructive lesion involving his sacrum and a portion of the adjacent pelvis. After a needle biopsy, he underwent a curettage of this lesion. However, two months following curettage he developed a recurrence. The patient had an embolization followed by therapy with the CyberKnife. He has had no recurrence and no neurological defect after five years.
Patient 6
A 60 year-old woman had a seven month history of pain in the lower back with a 30 pound weight loss. There was a mild bowel and bladder dysfunction. Imaging studies revealed a multi-locular cyst which on needle biopsy proved to be a aneurysmal bone cyst. The patient underwent a mid-sacral amputation with an en bloc resection of the tumor. She recovered from the surgery well and has no abnormal bowel and bladder function. She has no evidence of recurrence two years post-operatively.
Patient 7
A 57 year-old man who presented with severe pain in the low back and difficulty walking for 5 months. Imaging studies demonstrated a destructive sacral lesion. The biopsy showed aneurysmal bone cyst. The patient underwent an embolization followed by sacral resection with sparing of the L5-5, nerve roots. Histologic study of the entire neoplasm showed aneurysmal bone cyst with a suggestion of an underlying osteoblastoma. Three and one half years later there was a recurrence which was reembolized and curetted. Two years after the last surgery, the patient has residual bowel and bladder dysfunction but no evidence of recurrence.
Patient 8
A ten year-old girl had increasing left leg extremity pain. An MRI showed a multi-locular cyst consistent with aneurysmal bone cyst. She had a preoperatively embolization followed by a laminectomy of S1 and S2 with an extensive curettage and bone grafting of the lesion. Two years after surgery there is no neurologic deficit and no recurrence.
Patient 9
A five year old girl had back pain and difficulty walking for 3 months. An MRI showed a lesion consistent with an aneurysmal bone cyst. After a needle biopsy, she underwent a curettage with bone grafting and has been without evidence of recurrence or neurologic deficit for two years.
Patient 10
A 17 year old woman presented with low back pain and bowel and bladder dysfunction. An MRI showed a lesion consistent with aneurysmal bone cyst. The patient underwent a mid sacral amputation at the S2 level. Two years post op there is no evidence of recurrence and no bowel and bladder dysfunction.
CONICAL PRESENTATION
Patients ranged in age from five years to 64 years old. There were six women and four men. All patients presented with low back pain from three months to 10 years duration. Two patients had numbness and tingling in a leg, and four patients had bowel or bladder symptoms.
RADIOLOGIC FEATURES
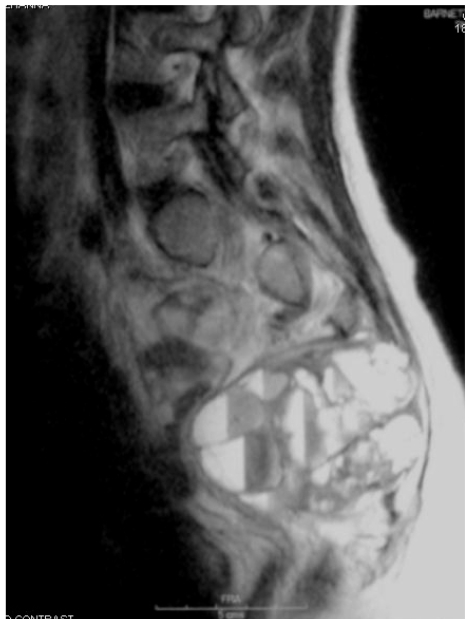
In all patients, the diagnosis of aneurysmal bone cyst was suspected on imaging studies. All patients had an MRI which showed a mutli-locular cystic lesion with fluid-fluid lines on T2-weighted images (Figure 1). Several patients had an associate soft tissue mass (Figure 2). Seven patients also had a CT scan, a modality best suited for evaluating the degree of bone destruction (Figure 3).
Figure 1.
A T2-weighted MRI showing the aneurysmal bone cyst of patient #8. The characteristic fluid-filled lines are present.
Figure 2.
A T2-weighted MRI showing the aneurysmal bone cyst of patient #6. There is a large soft tissue extension of the mass.
Figure 3.
An axial cut with the CT scan of patient #4. The image shows the extent of bone invasion.
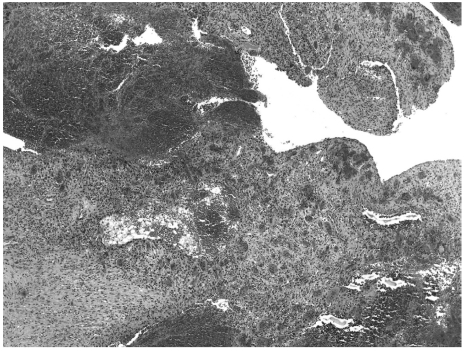
PATHOLOGIC FEATURES
Seven patients had CT guided needle biopsies. Three of these procedures did not provide diagnostic material and the patients required open biopsy. The other four needle biopsy procedures provided enough tissue to be interpreted as aneurysmal bone cyst only because the MRI image was highly characteristic. In the remaining three patients, the diagnosis was made by frozen section at the time of surgery.
All lesions showed multiple blood filled cavities, the characteristic feature of aneurysmal bone cyst best seen on low power. The cavities lacked an endothelial lining, and the stroma showed proliferating fibroblasts and scattered multinucleated giant cells. Reactive bone was often abundant (Figure 4).
Figure 4.
Medium power photomicrograph (H+E x 40) of the aneurysmal bone cyst of patient #3. Characteristic blood lakes are present.
In two patients, after meticulous study of many histologic slides, there was evidence of an underlying neoplasm. One patient had areas highly suggestive of a giant cell tumor and the other patient showed a few areas with features of osteoblastoma.
TREATMENT AND RESULTS
Six patients had no recurrence after the initial treatment. Three of these six had curettage. Two of these six patients had pre-operative embolization. The other three patients with no recurrence had resections or mid-sacral amputations; one of these had pre-op embolization.
Four patients suffered a recurrence from 6 months to 3.5 years following surgery. Patient 2 had a second recurrence. Recurrences were treated by curettage. One patient also had pre-op embolization, and two patients had CyberKnife therapy. All ten patients are currently disease free from two years to 12 years post surgery.
Two patients have residual bowel and bladder impairment and must catheterize themselves. These were the two patients who had histologic features suggesting an underlying primary bone tumor. All other patients are neurologically intact.
DISCUSSION
Prior discussions of sacral aneurysmal bone cysts has been limited. A few cases have been included in broad discussions of sacral tumors or as anecdotal case reports.5,6,7,8
Pagoda et al. described a single case of sacral aneurysmal bone cyst and reviewed the literature.9 This reported case was successfully treated by resection. Papagelapoulos et al. described 44 cases of pelvic aneurysmal bone cyst, twelve of which were in the sacrum.10 Those twelve cases were discussed with only limited detail, although the authors noted that there were no recurrences.
Despite the difficulties of achieving total extirpation of an aneurysmal bone cyst of the sacrum, these 10 cases confirm previous suggestions that surgical results are excellent. Six patients had no recurrence. These patients had distal sacral amputation if the lesions were caudal. Those lesions that involved the upper sacrum were curetted after careful dissection and preservation of the nerve roots. Of the patients who had recurrence, the recurrent lesions were successfully treated with recurettage. All patients are currently disease free for at least two years.
Five patients had adjunctive preoperative embolization, either for the primary lesion or for a recurrence. This modality is frequently used in the treatment of aneurysmal bone cysts because lesions are highly vascular, and embolization prevents heavy bleeding at surgery.5,11,12 This modality may have contributed to the excellent results of these cases.
In two cases, recurrent treatment of recurrent lesions included CyberKnife therapy. Conventional radiotherapy has been performed for sacral neoplasms. However, because aneurysmal bone cysts are benign, the possibility of malignant transformation after convention radiotherapy cannot be excluded. The CyberKnife system, used in our two patients, may be a safer modality.13
Neurologic manifestations are common in sacral neoplasms.14 However, in this series of sacral aneurysmal bone cysts, neurologic symptoms were mild. These included mild leg weakness and numbness in two patients. Four patients had bowel or bladder symptoms. These neurologic symptoms resolved in all but two patients who continue to have bowel or bladder dysfunction (patients 3 and 7). These two were patients who were found to have underlying benign neoplasms, a factor which possibly made the process more aggressive.
In summary, these ten cases suggest some management principles. First, the diagnosis is most strongly suggested by the MRI study. If the MRI findings are characteristic, a needle biopsy may be confirmatory. Occasionally, an open biopsy must be performed. Second, preoperative embolization is desirable. This significantly reduces intra-osseous bleeding and allows more meticulous surgery. Third, L5-S1 nerve roots must be preserved where possible. Caudal lesions can be treated by mid sacral amputation. More proximal lesions can be treated with a careful curettage which preserves nerve roots. Recurrences can be recuretted. Finally, the entire specimen must be examined histologically to rule out an underlying more aggressive neoplasm. Using these principles, therapeutic results for sacral aneurysmal bone cysts are excellent.
REFERENCES
- 1.Martinez V, Sissons HA. Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other bone pathology. Cancer. 1988;61:2291–304. doi: 10.1002/1097-0142(19880601)61:11<2291::aid-cncr2820611125>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 2.Capanna R, Bertoni F, Bettelli G, Present D, Biagini R, Ruggieri R, et al. Aneurysmal bone cysts of the pelvis. Arch Orthop Trauma Surg. 1986;105(5):279–84. doi: 10.1007/BF00449926. [DOI] [PubMed] [Google Scholar]
- 3.Marcove RC, Sheth DS, Takemoto S, Healey JH. The treatment of aneurysmal bone cyst. Clin Orthop. 1995;311:157–63. [PubMed] [Google Scholar]
- 4.Ruiter DJ, van Rijssel TG, van der Velde EA. Aneurysmal bone cysts: a clinicopathological study of 105 cases. Cancer. 1977;39(5):2231–9. doi: 10.1002/1097-0142(197705)39:5<2231::aid-cncr2820390541>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 5.Yildirim E, Ersözlü S, Kirbas I, Özgür AF, Akkaya T, Karadeli E. Treatment of pelvic aneurysmal bone cysts in two children: selective arterial embolization as an adjunct to curettage and bone grafting. Diagn Interv Radiol. 2007;13(l):49–52. [PubMed] [Google Scholar]
- 6.Rajadhyaksha C, Connolly LP, Connolly SA, Treves ST. Aneurysmal bone cyst of the sacrum: value of three-phase imaging. Clin Nucl Med. 2003;28(11):933–5. doi: 10.1097/01.rlu.0000093092.31401.5c. [DOI] [PubMed] [Google Scholar]
- 7.Gloss DS, Wilson S, Rodgers B, Nietzchman HR. Radiology case of the month. Leg Pain. Radiologic diagnosis: giant cell tumor of sacrum with aneurysmal bone cyst. J La State Med Soc. 2006;158(6):271–3. [PubMed] [Google Scholar]
- 8.Puri A, Agarwal MG, Shah M, Srinivas CH, Shukla PJ, Shrikhande SV, et al. Decision making in primary tumors. The Spine Journal. 2008 Dec 5; doi: 10.1016/j.spinee.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Pogoda P, Linhart W, Priemel M, Rueger J, Amling M. Aneurysmal bone cysts of the sacrum. Clinical report and review of the literature. Arch Orthop Trauma Surg. 2003 1;123(5):247–51. doi: 10.1007/s00402-003-0496-x. [DOI] [PubMed] [Google Scholar]
- 10.Papagelopoulos PJ, Choudhury SN, Frassica FJ, Bond JR, Unni KK, Sim FH. Treatment of aneurysmal bone cysts of the pelvis and sacrum. J Bone Joint Surg Am. 2001;86(A(ll)):1674–81. doi: 10.2106/00004623-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 11.De Cristofaro R, Biagini R, Boriani S, Ricci S, Ruggieri P, Rossi G, Fabbri N, Roversi R. Selective arterial embolization in the treatment of aneurysmal bone cyst and angioma of bone. Skeletal Radiol. 1992;21:523–7. doi: 10.1007/BF00195235. [DOI] [PubMed] [Google Scholar]
- 12.Konya A, Szendroi M. Aneurysmal bone cysts treated by superselective embolization. Skeletal Radiol. 1992;21:167–72. doi: 10.1007/BF00242130. [DOI] [PubMed] [Google Scholar]
- 13.Gibbs IC, Chang SD. Radiosurgery and radiotherapy for sacral tumors. Neurosurg Focus. 2003;15(2:E8):1–5. doi: 10.3171/foc.2003.15.2.8. [DOI] [PubMed] [Google Scholar]
- 14.Payer M. Neurological manifestation of sacral tumors. Neurosurg Focus. 2003;15(2:E1):1–6. doi: 10.3171/foc.2003.15.2.1. [DOI] [PubMed] [Google Scholar]