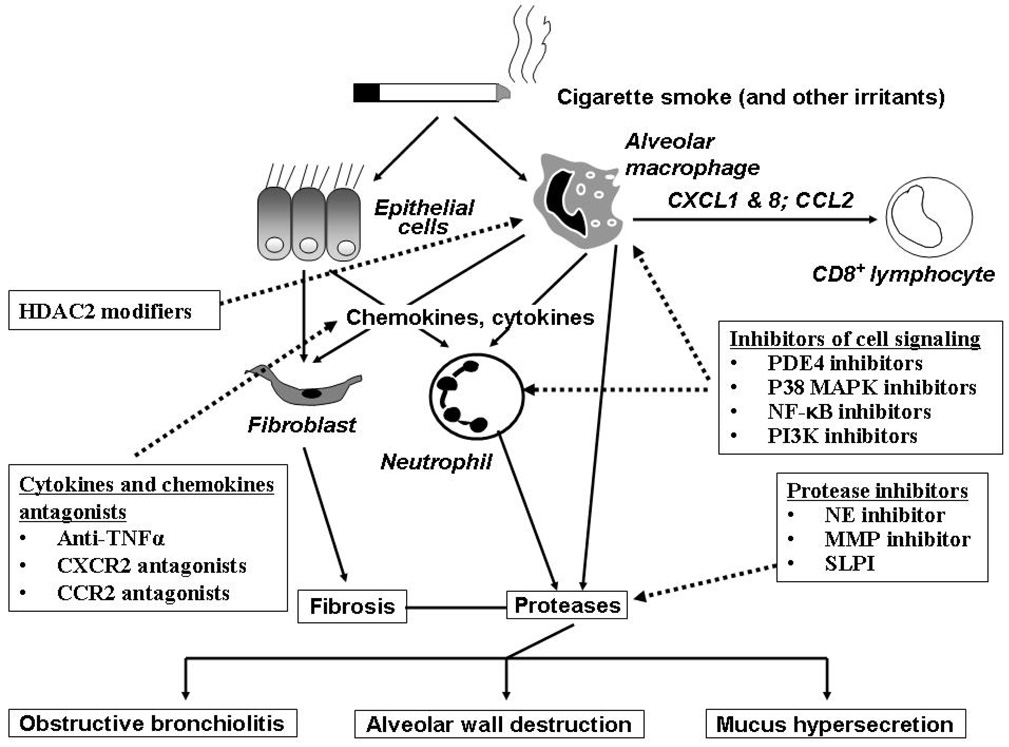
Figure 1. Pulmonary inflammation in COPD and emerging anti-inflammatory therapy.
Exposure to cigarette smoke in susceptible individuals leads to an abnormal inflammation which appears to be self-perpetuating and is perhaps linked to infection. Alveolar macrophages and pulmonary epithelial cells release all kinds of inflammatory mediators in response to cigarette smoke which activate and stimulate migration of pulmonary inflammatory cells including neutrophils, macrophages and lymphocytes. The chronic and persistent inflammation that ensues is thought to be responsible for both the symptoms of disease and also the progressive decline in lung function that is seen in COPD patients. The loss of airway function appears to be related to the destruction of alveoli resulting in a loss of elasticity linked to increased protease activity, and obstruction and fibrosis of the small airway as a result of inflammation and mucus hyper-secretion. Emerging anti-inflammatory therapies under clinical investigation attack this chronic pulmonary inflammation via several strategies. Signaling pathway inhibitors such as PDE4 inhibitors, p38 MAPK inhibitors, NF-κB signaling inhibitors and PI3K inhibitors are in development. Reduction of pleiotropic inflammatory cytokines such as TNF-α using monoclonal antibodies that target the ligands, or soluble receptors that bind and inactivate TNF-α may also reduce the inflammatory burden in the lung. Targeting chemokines such as MCP-1 and IL-8 may reduce the influx of inflammatory cells into the lungs from the circulation by reducing the chemotactic gradient. Inhibition of protease activity in the lung may attenuate lung tissue damage and reduce the numbers of lung neutrophils. Increase HDAC2 expression restores the steroids sensitivity for treatment of COPD. Reducing the severity of inflammation in the lung may improve lung function and slow the progression of COPD.