Abstract
Carpal instabilities continue to be a controversial topic in hand surgery. Accurate diagnosis of the ligament injuries is usually difficult without an arthroscopic evaluation. Few studies have focused on the diagnosis and proper management of simultaneous scapholunate (SL) and lunotriquetral (LT) ligament tears. This is an uncommon injury that leads to marked disability and chronic wrist pain. This is essentially a “floating lunate” and indicates a severe ligamentous lesion. Thirteen patients (six female and seven male) with complete SL and LT tears and with gross arthroscopic dynamic carpal instability were included in the present study. None of the patients showed radiographic evidence of lunate dislocation. One patient presented acutely and was operated on 3 days after the injury. The average time from the initial injury to the arthroscopy for the other 12 patients was 13.5 months (range 1.5–84 months). All patients underwent arthroscopic debridement of the SL and LT ligaments coupled with percutaneous pinning (two 0.045-in. Kirschner wires) in both joints. At the final follow-up, the average range of motion was 50° of flexion, 54° of extension, 77° of pronation, 80° of supination, 25° of ulnar deviation, and 15° of radial deviation. The average final grip strength was 67% from the non-affected side. All patients had negative shifting tests at final follow-up. Furthermore, there was no evidence of any static or dynamic instability in all the patients except for one patient who developed a volar intercalated segment instability 8 months after the surgery. At the final follow-up, ten patients had no pain, one had mild pain, and two experienced moderate pain.
Keywords: Carpal instabilities, Arthroscopy, Ligamentous tears, Lunate instability
Introduction
Carpal instabilities result from common injuries often associated with high energy trauma and sports-related activities [26]. They continue to be one of the most controversial topics in hand surgery. The absence of obvious clinical findings and radiological parameters has made the establishment of an accurate diagnosis of specific ligament injuries difficult [19]. The provocative maneuvers described to assess instability remain largely physician dependent [10, 18, 25]. There are no definitive radiographic criteria to evaluate and classify carpal instabilities. Moreover, magnetic resonance imaging, arthrography, and bone scans do not reliably differentiate true complete ligamentous injuries [19, 27]. On the other hand, it has been demonstrated that arthroscopy provides superior evaluation of the intrinsic ligaments of the wrist even when compared to open arthrotomy [4, 5, 17, 21].
The stability of the scapholunate (SL) and lunotriquetral (LT) complexes depends on both the interosseous ligaments and extrinsic capsular elements [23]. The most critical region of the scapholunate complex is the dorsal area of the interosseous ligament, while the stoutest region of the LT ligament is the palmar [23]. The central and proximal segments of the SL and LT ligaments are slim fibrocartilaginous structures with inadequate vascular supply [3, 22].
Ruch and Poehling [20] presented their experience with arthroscopic management of isolated partial SL and LT ligament injuries without any evidence of instability. However, no studies are found with the use of this technique on complete SL and LT ligament tears. Due to the presence of both scapholunate and lunotriquetral instabilities, we term this condition as the “floating lunate”. The purpose of this study is to present the outcome of patients who underwent arthroscopic treatment of complete SL and LT ligament tears associated with dynamic carpal instability.
Materials and Methods
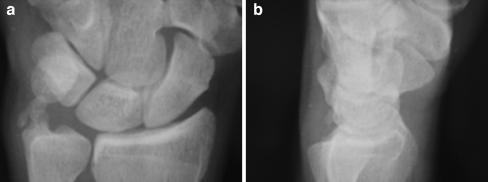
A retrospective review of the wrist arthroscopic procedures performed between January 1996 and November 2002 revealed 13 patients (six female and seven male; Table 1) with complete SL and LT tears and gross arthroscopic dynamic carpal instability. All the surgical procedures were performed by the senior author. The operative notes and arthroscopic images from these 13 patients were thoroughly reviewed. The average age was 39 years old (range 22–57). The right wrist was injured in nine patients and it was the dominant hand in all of them. The left wrist was involved in the remaining four patients (one dominant and three non-dominant). The mechanism of injury in most of the patients was a fall leading to hyperextension injury at the wrist; however, few patients could not specify the mechanism of injury. One out of the 13 patients was treated acutely (3 days after the trauma) due to severity of the symptoms. The average time from the initial injury to the arthroscopy for the other 12 patients was 13.5 months (range 1.5–84 months). Conservative treatment in all the patients had included a short arm cast or splint for 4–6 weeks, pain medications, and occupational therapy. One patient had received a steroid injection besides the immobilization. Preoperative studies included standard postero-anterior (PA) and true lateral views (Fig. 1a, b), radial, and ulnar deviation views.
Table 1.
Demographic profiles of the patients.
| Case | Sex | Age | Occupation | Dominant hand | Injured hand | Mechanism of injury | Time since injury (months) |
|---|---|---|---|---|---|---|---|
| 1 | F | 50 | Professor | R | R | Torsion | 7 |
| 2 | F | 36 | Security | R | R | Torsion | 20 |
| 3 | F | 33 | Secretary | R | R | Minor trauma | 84 |
| 4 | M | 42 | Cashier | R | L | Fall | 3.5 |
| 5 | M | 37 | Travel agent | R | R | Torsion | 8 |
| 6 | M | 42 | Exporter | R | R | Hyperflexion | 2.5 |
| 7 | F | 29 | Professor | R | R | Fall | 2 |
| 8 | M | 42 | Inspector | R | R | Not clear | 6 |
| 9 | F | 22 | Student | R | R | Hyperextension + rotation | 10 |
| 10 | M | 40 | Human resources | R | R | Not clear | 12 |
| 11 | M | 27 | Loader | R | L | Fall | 3 days |
| 12 | M | 52 | Mailman | L | L | Torsion | 5 |
| 13 | F | 57 | Custodian | R | L | Hyperextension | 1.5 |
Figure 1.
a, b Preoperative radiographs in PA and lateral views. Note that the radiographs look essentially normal as the lunate remains in a neutral position since both the SL and LT ligaments are torn.
Average follow-up after surgery was 52 months (range 20–84 months). Patients were evaluated at final follow-up for wrist motion, pain, and grip strength using the Disabilities of the Arm, Shoulder and Hand (DASH) [9] score system.
Surgical Technique
All patients underwent a thorough arthroscopic examination of the radiocarpal joint with a 2.7-mm 30° scope in the 3–4 working portal, the in-flow cannula being attached to the scope. Ten pounds of traction was applied via two Chinese finger traps secured to a shoulder holder device.
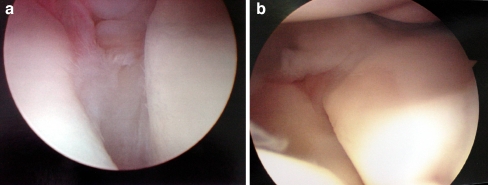
Generally, a diffuse synovitis was seen and a 4–5 or 6R portal was used to initiate a synovectomy using a 2.9 full radius shaver. This allowed better inspection of the interosseous ligaments and gave better access to the triangular fibrocartilage complex (TFCC). Radiofrequency ablator probes (Smith & Nephew) were often used as well to assist in this process. Scapholunate tears were much easier to identify and often consisted of frayed ligamentous tissue in the scapholunate interval. A probe was used to elucidate the extent of the tear and the same was done for the lunotriquetral interval, but this was much more difficult to distinguish and changing portals for the scope was often necessary. To determine the true extent of the tear and to easily inspect the SL and LT intervals, the midcarpal portals (usually radial midcarpal) were established. In the scapholunate tears, the instability was detected as follows: with the arthroscope looking directly down on the SL interval in the midcarpal joint, the scaphoid tubercle is gently pressed with the other hand while the carpus is stabilized. One will see rocking or a clear step off between the scaphoid and lunate in cases of dynamic instability (Fig. 2a). This is an indication for stabilization after debridement. The same maneuver is applied to the lunotriquetral interval (Fig. 2b), the pressure being applied over the pisiform bone. Instability at either interval is an indication for debridement and stabilization using pin fixation.
Figure 2.
a Intraoperative photograph showing the diastasis at the scapholunate interval, as seen from the midcarpal portal. b Intraoperative photograph showing the diastasis at the lunotriquetral interval, as seen from the midcarpal portal.
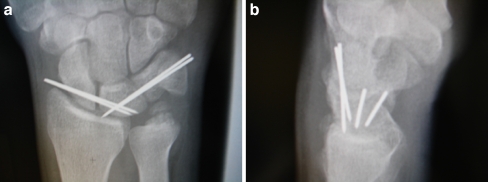
Once the debridement of the torn ligament is completed, two 0.045 Kirschner wires are driven across both the SL and LT intervals under fluoroscopic control (Fig. 3a, b). The ligament debridement must be aggressive enough to encourage bleeding at the site and stimulate ligament healing. Due to collagen crosslinking, this process will take approximately 8 weeks and then the pins can be removed. During this time, the patient’s wrist, including the buried pin sites under the skin, are protected by a well-padded thumb spica short arm fiberglass cast. Pin removal with fluoroscopic assistance can be coupled with gentle passive manipulation of the wrist, in some cases, which is then followed by 6–8 weeks of hand therapy. A removable splint can be used for more vigorous activities of daily living. Grip strength testing and wrist range of motion are carefully monitored throughout the rehabilitation.
Figure 3.
a, b Radiographs showing the pinning of scapholunate and lunotriquetral intervals in PA and lateral views, respectively.
Results
Two of the patients had a healed ulnar styloid fracture as an incidental finding. Eight patients complained of tenderness at scapholunate interval; however, all the patients presented with some degree of mechanical symptoms like “clicking” or “catching” with wrist motion. On physical examination, the scaphoid shift test was positive in nine and negative in four patients. Surprisingly, none of the patients showed abnormal lunotriquetral shear test.
During the arthroscopic procedure, complete or nearly complete tear of the scapholunate and lunotriquetral interosseous ligaments and dynamic carpal instability were found in all the patients. The instabilities were graded according to Geissler’s classification (nine grade III and four grade II) [6]. Local synovitis was demonstrated in the area of the torn ligaments and throughout the dorsal capsule. Associated injuries included TFCC tears in eight patients [one (I A) and seven (I B)] [14, 15]. One of the patients had ulnar variance >+1 (1 mm positive), so an oblique ulnar shortening osteotomy was performed. In this patient, ulnar impaction signs were also noted on the articular surface of the lunate.
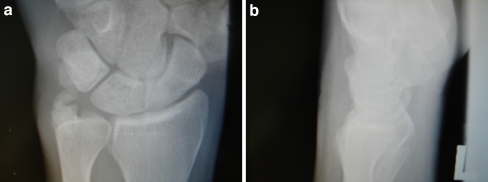
Debridement was performed for the central TFCC tear and suture repair with PDS was indicated for the peripheral tears while several patients underwent suture welding using nylon for the TFCC repair [2]. Radiographic studies (Fig. 4a, b) demonstrated no instability at final follow-up in all but one patient who displayed a volar intercalated segment instability (VISI) pattern on the lateral radiograph. At the final follow-up, ten patients had no pain, one had mild pain, and two had moderate pain. The average final range of motion (Fig. 5a, b) was 50° of flexion, 54° of extension, 77° of pronation, 80° of supination, 25° of ulnar deviation, and 15° of radial deviation. The average final grip strength was 67% from the non-affected side. All patients had negative shifting tests at final follow-up. The average DASH [9] score at final follow-up was 10.7 (general population ~5).
Figure 4.
a, b Radiographs at the final follow-up in PA and lateral views.
Figure 5.
a, b Clinical photographs at the final follow-up showing wrist ROM. c Clinical photograph showing the minimal scars of the arthroscopic portals at the final follow-up.
An early complication encountered was superficial infection around a prominent pin site in one patient that responded well to antibiotics. One of the patients who complained of moderate pain ended up with 50 lb lifting limitation due to SL tenderness and lack of adequate wrist extension. After 8 months from the first procedure, one patient developed VISI. Open reduction and internal fixation of the SL and LT intervals were performed by dorsal capsulodesis and bone suture anchors on the dorsal aspect of the SL joint along with pinning of both the SL and LT intervals. Intraoperative findings at the time of the second surgery included scarring of the majority of the SL ligament fibers, an unstable SL interval, a full-thickness lesion of the radiolunate ligament, a flexed lunate, and an unstable LT joint.
Discussion
Carpal instability has been recognized as the absence of proper skeletal and ligamentous support to keep the wrist stable to external loads involved in pinching and grasping. This phenomenon can be either static (at rest) or dynamic (with use), and is usually due to ligament tears, fractures, or both [5, 11]. Cooney et al. proposed a classification based on the compromise of static and dynamic components of the wrist [5]. Mayfield et al. [13] described the simultaneous involvement of the SL and LT as stage III in the progressive injury pattern of perilunate instability. There are multiple studies about the treatment of isolated injuries of the SL or LT ligaments [1, 7, 8, 12, 24]. However, there are few reports on the treatment of concurrent tears of these structures without perilunate dislocation [20, 27]. Ping et al. [16] presented their results on eight patients with wrist pain due to coincident SL and LT disruptions in the absence of perilunate dislocation. Seven patients were treated by simultaneous scapho-trapezio-trapezoid fusion and LT fusion. At final follow-up, three out of seven patients did not have any pain, two complained of pain with extremes of motion, and two needed further surgery. In the same study, they confirmed by biomechanical testing that the intrinsic ligaments could be entirely disrupted while the extrinsics are partially injured. Ruch and Poehling [20] reported on the outcome of 14 patients with chronic wrist pain with arthroscopic debridement and early mobilization for the management of concomitant partial SL and LT ligaments tears. Eleven patients in this series had complete pain relief and returned to work within a period of 7 weeks. The other three patients complained of occasional mild pain. Radiographic studies obtained at final follow-up showed no evidence of abnormalities.
As opposed to the study of Ruch and Poehling [20], our series was comprised of 13 patients with complete disruption of the SL and LT ligaments in the absence of lunate dislocation and our results are comparable. Furthermore, our results are better than the results reported by Ping et al. [16]. We agree with Ping et al. [16] that this condition precedes perilunate dislocation; however, treatment by two different intercarpal fusions (STT and LT) can be fraught with complications. There can be failure of fusion, persistent pain, or severe motion restriction. We decided to name this traumatic anomaly the “floating lunate” since the ligamentous attachments on both sides of the lunate are devoid and the lunate floats in a neutral position, hence the deceivingly normal plain radiograph (Fig. 1a, b). The results of the present study indicate that thorough arthroscopic debridement of the SL and LT intervals coupled with assisted reduction and percutaneous pinning provided satisfactory results in the majority of the patients. This procedure does not have complications presumably due to its minimally invasive nature; more so, it results in a better cosmetic scar as compared to an open procedure (Fig. 5c). Only one patient required additional surgery due to the development of a static instability pattern (VISI).
Conclusion
Our retrospective clinical study indicates that patients with persistent wrist pain after blunt trauma may have a “floating lunate” type lesion, namely concomitant scapholunate and lunotriquetral ligament dynamic tears. These are frequently missed on imaging studies and plain radiographs are usually normal due to a neutral position of the lunate. It can be thought of as a precursor lesion to a perilunate or even lunate dislocation. Our analyses of the functional results indicate that patients recover the majority of their range of motion and go back to previous work or sports activity. Simultaneous tears with instability that require pinning have not been described in the literature and our assessment suggests these injuries are relatively uncommon and can be effectively managed with arthroscopic means.
Contributor Information
Alejandro Badia, Email: alejandro@drbadia.com.
Prakash Khanchandani, Phone: +1-305-6613000, FAX: +1-305-6613054, Email: drprakashk@hotmail.com.
References
- 1.Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res 1982;164:199–207. [PubMed]
- 2.Badia A, Jimenez A. Arthroscopic repair of peripheral triangular fibrocartilage complex tears with suture welding: a technical report. J Hand Surg [Am] 2006;31 8:1303–7. doi:10.1016/j.jhsa.2006.05.016. [DOI] [PubMed]
- 3.Berger RA. General anatomy of the wrist. In: An K-N, Berger RA, Cooney SP III, editors. Biomechanics of the wrist joint. New York: Springer; 1991. p. 1–22.
- 4.Botte MJ, Cooney WP, Linscheid RL. Arthroscopy of the wrist: anatomy and technique. J Hand Surg [A] 1989;14:313–6. doi:10.1016/0363-5023(89)90029-4. [DOI] [PubMed]
- 5.Cooney WP, Dobyns JH, Linscheid RL. Arthroscopy of the wrist: anatomy and classification of carpal instability. Arthroscopy 1990;6:133–40. doi:10.1016/0749-8063(90)90014-5. [DOI] [PubMed]
- 6.Geissler WB, Freeland AE, Savoie F, et al. Intra-carpal soft tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg 1996;78-A 3:357–65. [DOI] [PubMed]
- 7.Glickel SZ, Millender L. Ligamentous reconstruction for chronic intercarpal instability. J Hand Surg [A] 1984;9A:514–27. [DOI] [PubMed]
- 8.Goldner JL. Treatment of carpal instability without joint fusion: current assessment. J Hand Surg [A] 1982;7:325–6. [DOI] [PubMed]
- 9.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disability of the Arm, Shoulder and Hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602–8. doi:10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed]
- 10.Lane LB. The scaphoid shift test. J Hand Surg [A] 1993;18A:366–8. doi:10.1016/0363-5023(93)90377-F. [DOI] [PubMed]
- 11.Lichtman DM, Schneider JR, Swafford AR, Mack GR. Ulnar midcarpal instability. Clinical and laboratory analysis. J Hand Surg [A] 1981;6:515–23. [DOI] [PubMed]
- 12.Lichtman DM, Noble WH III, Alexander CE. Dynamic lunotriquetral instability: case report. J Hand Surg [A] 1984;9A:185–7. [DOI] [PubMed]
- 13.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [A] 1980;5:226–41. [DOI] [PubMed]
- 14.Palmer AK. Triangular fibrocartilage disorders: injury patterns and treatment. Arthroscopy 1990;6 2:25–32. doi:10.1016/0749-8063(90)90013-4. [DOI] [PubMed]
- 15.Palmer AK, Dobyns JH, Linscheid RL. Management of posttraumatic instability of the wrist secondary to ligament rupture. J Hand Surg [A] 1978;3:507–32. [DOI] [PubMed]
- 16.Ping PG, Nowak M, Logan SE, Young VL, Gilula LA, Weeks PM. Coincident rupture of the scapholunate and lunotriquetral ligaments without perilunate dislocation: pathomechanics and management. J Hand Surg [A] 1990;15A:110–9. [DOI] [PubMed]
- 17.Poehling G, Whipple TL, Roth J, Koman LA. AAOS Instructional Course Lectures 1988, St Louis, Mosby. [PubMed]
- 18.Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg [A] 1984;9A:502–14. [DOI] [PubMed]
- 19.Ruby LK, Cooney WP, An KN, Linscheid RL, Chao EYS. Relative motion of selective carpal bones: a kinematic analysis of the normal wrist. J Hand Surg [A] 1988;3:1–10. doi:10.1016/0363-5023(88)90189-X. [DOI] [PubMed]
- 20.Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg [A] 1996;21A:412–7. doi:10.1016/S0363-5023(96)80354-6. [DOI] [PubMed]
- 21.Ruch DS, Bowling J. Arthroscopic assessment of carpal instability. J Arthro Rel Surg A 1998;14:675–81. doi:10.1016/S0749-8063(98)70093-3. [DOI] [PubMed]
- 22.Viegas SF, Patterson RM, Peterson PD, et al. Ulnar-sided peri lunate instability: an anatomic and biomechanical study. J Hand Surg [A] 1990;15A:268–78. doi:10.1016/0363-5023(90)90107-3. [DOI] [PubMed]
- 23.Walsh JJ, Berger RA, Cooney WP. Current status of scapholunate interosseous ligament injuries. J Am Acad Orthop Surg 2002;10:32–42. [DOI] [PubMed]
- 24.Watson HK, Ashmead D IV, Makhlouf MV. Examination of the scaphoid. J Hand Surg [A] 1988;13A:657–60. [DOI] [PubMed]
- 25.Watson HK, Goodman ML, Johnson TR. Limited wrist arthrodesis: II. Intercarpal and radiocarpal combinations. J Hand Surg [A] 1981;6:223–33. [DOI] [PubMed]
- 26.Weiss LS, Taras JS, Sweet S, Osterman AL. Lunotriquetral injuries in the athlete. Hand Clin 2000;16:433–8. [PubMed]
- 27.Zlatkin MB, Chao PC, Osterman AL, et al. Chronic wrist pain: evaluation with high resolution MR imaging. Musculoskelet Radiol 1989;173:723–9. [DOI] [PubMed]